CASE PRESENTATION
A 26-year-old man presented in 2011 with moderately advanced keratoconus in his left eye. His UCVA was 20/25 OD. His BCVA with a scleral contact lens was 20/25 OS.
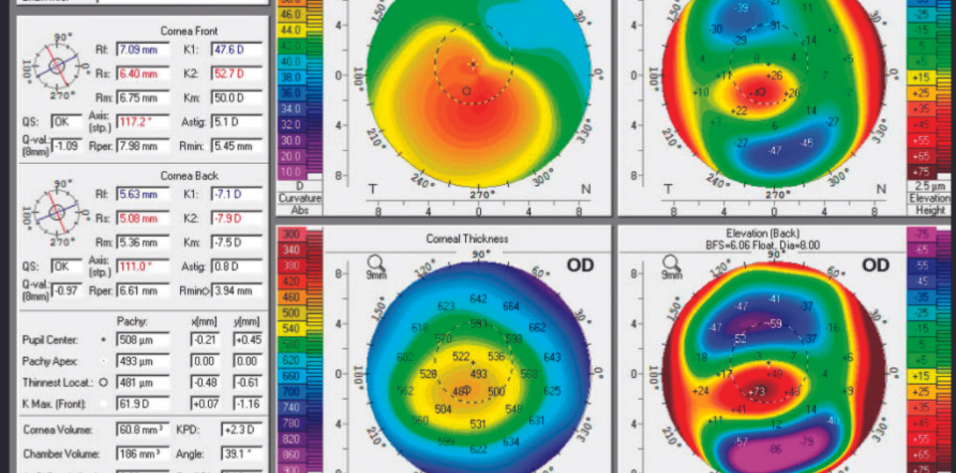
In 2018, the patient returned with significant keratoconic progression in both eyes (Figure 1). Surgery was recommended. He received 450-µm intrastromal corneal ring segments (ICRSs; Intacs, CorneaGen) in the left eye first, followed by the right eye 3 months later. The patient was subsequently able to resume wearing contact lenses for 2 years but then developed giant papillary conjunctivitis (GPC) and contact lens intolerance.

Figure 1. Imaging with the Pentacam demonstrates keratoconic progression in the left (A) and right (B) eyes.
He wished to be free of contact lenses and able to wear spectacles. CXL was performed on the right eye, followed by the left. Each eye demonstrated stability 3 to 4 months after CXL (Figure 2). Bilateral PRK was performed off label. A wavefront-guided procedure targeting -0.64 -5.46 x 014º was performed on the right eye, and traditional PRK targeting -0.50 -5.50 x 156º was performed on the left eye.

Figure 2. Images of the left (A) and right (B) eyes obtained with the Pentacam (Oculus Optikgeräte) before PRK was performed to reduce the patient's corneal astigmatism.
A small keloid scar developed in the left eye 5 months after PRK and was easily removed in a minor procedure room. The patient was treated with low-dose topical steroids and oral vitamin C. A Prokera device (BioTissue) was placed on the left eye to treat epithelial breakdown in the setting of reduced corneal sensation.
The left eye continues to heal. The patient’s BCVA is currently 20/50-2 OS. His BCVA is 20/25+1 OD with a manifest refraction of +4.25 -4.75 x 050º.
How would you approach a patient like this one who has keratoconus, develops contact lens intolerance, and wishes to wear spectacles? What recommendations do you make to these individuals if they are willing to undergo off-label refractive treatment for keratoconus?
—Case prepared by Alan N. Carlson, MD

BHARAT GURNANI, MBBS, DNB, FCRS, FAICO, FICO, MRCSED, MNAMS
In situations like this, contact lens wear is discontinued. Treatment with a topical corticosteroid (loteprednol or dexamethasone), a topical antihistamine (olopatadine hydrochloride ophthalmic solution 0.1% [Olopat, Ajanta Pharma]), and ocular lubricants (hydroxypropyl methylcellulose or carboxymethylcellulose) is initiated. After the GPC is under control and the patient is asymptomatic (about 1–2 months), CXL is performed to stabilize the cornea. During the first month after CXL, patients can continue wearing spectacles; those who require high degrees of astigmatic correction or have high anisometropia may benefit from optical techniques such as undercorrection or a slab-off to improve their spectacle tolerance.
In the current case, the cone is nearly central and the astigmatism is irregular and oblique. If the patient is highly motivated to undergo refractive surgery, three options could be considered after refractive and corneal stability is achieved.
No. 1: A toric phakic IOL. Most individuals with keratoconus also have myopic astigmatism and a deep anterior chamber. For them, an EVO Toric ICL (STAAR Surgical) can be an effective strategy. Postoperative recovery is rapid. Surface ablation may be performed in the future if the keratoconus progresses. This approach would be my first choice in the current case, although I would anticipate some residual astigmatism.
No. 2: CXL combined with topography-guided surface ablation. Traditional PRK removes a lot of tissue, and the patient’s corneal thickness is marginal. Topography-guided surface ablation would therefore be preferable and could significantly reduce the refractive error. Given the patient’s high astigmatism, this surgical approach offers two additional advantages—eye tracking and cyclotorsion control—that could help reduce higher-order aberrations and the refractive error. Results can be variable, but topography-guided PRK would be my second choice in the current case.
No. 3: Refractive lens exchange for a toric IOL. A toric extended depth of focus IOL could provide the patient with good-quality vision. Given his age and the procedure’s impact on accommodation, however, it would be my third choice.
No. 4: Scleral contact lenses and penetrating keratoplasty (PKP). These would be my last resort given the patient’s contact lens intolerance and problems associated with PKP such as irregular astigmatism and graft rejection.

WILLIAM B. TRATTLER, MD
Keratoconus is a progressive condition. The first step is to strengthen the cornea and prevent disease progression with CXL. If the procedure had been performed soon after the patient’s initial diagnosis, he would likely have maintained his 20/25 UCVA OD and been spared the multiple procedures performed on the eye.
CXL can prevent further deterioration in and often improves the shape of the cornea. In some instances, the corneal reshaping improves patients’ UCVA and BCVA. ICRSs also reshape the cornea, but they typically do not prevent disease progression.1
One of my main concerns upon reading the case presentation is that severe irregular astigmatism was present within the visual axis before the planned PRK procedure. The Pentacam allows us to focus on the four central keratometry readings within the visual axis. Two of these areas are labeled 40.80 D and 54.00 D (a 13.20 D gradient; Figure 2A) in the left eye, and two are labeled 37.60 D and 54.40 D (a 16.80 D gradient; Figure 2B) in the right eye. Wavefront- or topography-guided PRK is unlikely to regularize this degree of irregular astigmatism effectively. I am hopeful that topography-guided reshaping with technologies such as Phorcides (Alcon) can improve corneas with this high level of irregular astigmatism, but more evidence is needed.
I hope that advances in topography-guided PRK will allow patients with advanced keratoconus and significant irregular astigmatism to experience an improvement in their corneal shape and vision. I also hope that the results will be stable, which is a concern in eyes with keratoconus. Currently, the most effective way to halt further disease progression in patients with advanced keratoconus is to perform CXL and then fit them with scleral lenses, which can dramatically improve the vision of most of these individuals.
In the current case, the patient was successful with scleral lenses but developed GPC. This condition can be a challenge to treat, but a number of medications can be effective. Topical agents may then be prescribed to prevent recurrent GPC. I would expect scleral lenses to offer the patient the best possible visual results and with significantly less risk of complications than surgery.

WHAT I DID: LLOYD WILLIAMS, MD, PHD
Scleral contact lenses have revolutionized the correction of irregular astigmatism. They frequently provide patients—even those who have extremely abnormal corneas—with excellent vision. The patient in this case, however, could not wear contact lenses.
PKP was an option but one I reserve as a last resort because it can introduce problems such as irregular astigmatism, transplant rejection, and increased susceptibility to trauma. Moreover, PKP often does not eliminate a patient’s need for a scleral contact lens, which was the individual’s goal.
Wavefront-guided surface ablation was performed to reduce the topographic irregularity of the cornea. (My clinic does not have a topography-guided laser system.) The ICRSs presented a problem. Light was used to adjust the pupil size and thereby reduce the wavefront size to include only the cornea within the rings. The amount of astigmatism in the left eye exceeded the limit for a wavefront-guided treatment. In the worst-case scenario, a PKP would still have been possible.
Keloid scarring prolonged and complicated the postoperative healing and outcome. Pre- and postoperative tomography with the Pentacam failed to demonstrate the desired change from the PRK treatment. I attributed the failure to epithelial remodeling and a mild recurrence of the patient’s keloid. His goal of recovering his vision with spectacle correction was nevertheless ultimately achieved.

DISCUSSION: ALAN N. CARLSON, MD
The patient presented uncommon challenges. General principles of keratoconus management, however, remain relevant. Eye rubbing and mechanical pressure from certain sleeping positions can contribute to floppy eyelid syndrome and keratoconus, working against CXL treatment. Dry eye disease (DED) can be more prevalent in patients with unusually steep corneas, potentially complicating contact lens wear. Specifically, DED can aggravate the mechanical interaction between the eyelid and the contact lens, resulting in GPC and contact lens intolerance, as in the current case. Additionally, obstructive sleep apnea is more common in patients with keratoconus,2 and a poor-sealing continuous positive airway pressure mask can exacerbate DED. It is exciting that an expansion in keratoconus treatment options has made the requirement for a full-thickness PKP relatively rare.
1. Vega-Estrada A, Alió JL, Plaza-Puche AB. Keratoconus progression after intrastromal corneal ring segment implantation in young patients: five-year follow-up. J Cataract Refract Surg. 2015;41(6):1145-1152.
2. Gupta PK, Stinnett SS, Carlson AN. Prevalence of sleep apnea in patients with keratoconus. Cornea. 2012;31(6):595-599.