
IOL exchanges are becoming a more frequent solution for patients who experience dysphotopsias or dissatisfaction following cataract surgery. This article presents a case in which an IOL exchange was performed with a Light Adjustable Lens (LAL; RxSight; off-label indication), an approach I am considering implementing more often in the future.
CASE EXAMPLE
Presentation
A 66-year-old woman presented whose primary goal was achieving near vision sharp enough to groom her dog and improving her distance vision. She had a history of pseudoexfoliation and primary open-angle glaucoma, and she had undergone a trabeculectomy paired with concurrent bleb revision and toric posterior chamber IOL (PCIOL) implantation in the right eye.
The intended axis of implantation at 165º had drifted to approximately 110º postoperatively in the right eye (Figure 1). This shift underscores the unpredictability of outcomes when operating on eyes with existing blebs, even when the surgical modifications are minimal. Additionally, the earlier surgery had resulted in unintended iris tissue removal, leading to significant postoperative glare.
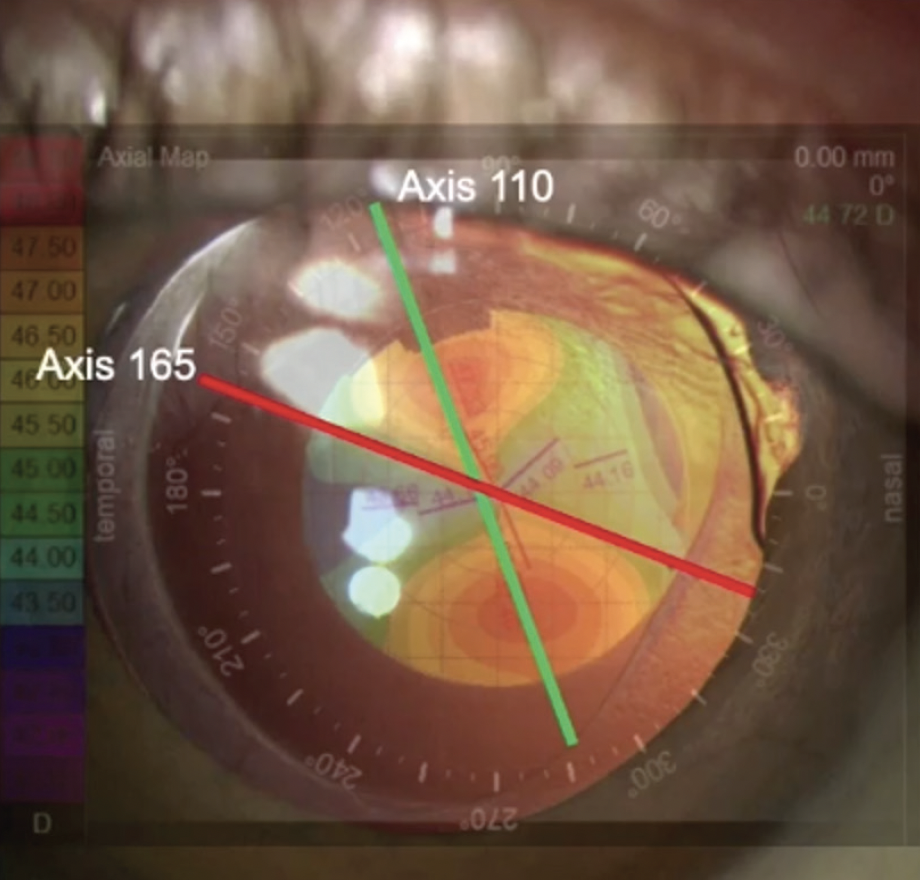
Figure 1. Postoperative shift in the toric IOL axis. The red line at 165º indicates the intended axis of implantation; the green line at 110º shows the actual axis postoperatively.
A comprehensive workup of the patient was performed that included retinal nerve fiber layer analysis and visual field testing to assess optic nerve health, endothelial cell counts to evaluate corneal integrity, and a macular assessment to rule out hypotony maculopathy, a concern after trabeculectomy. Corneal topography was performed to evaluate the corneal shape, and higher-order aberrations and refractive error were measured with the iTrace (Tracey Technologies; Figure 2).

Figure 2. The toric data revealed that a 53º rotation would be recommended to decrease the cylinder with rotation. This, however, would not have met the need for a -2.50 D spherical equivalent and would have resulted in a hyperopic outcome. An IOL exchange was therefore the preferred approach.
I initially considered a simple rotation of the toric PCIOL. It soon became evident, however, that this strategy would not meet the patient’s visual requirements, because it would result in a hyperopic outcome, contrary to her preference for moderate myopia.
After thorough consideration and analysis, a decision was made to exchange the PCIOL for an LAL. The aim was to address the patient’s specific refractive needs and repair the small iris defect causing glare.
Surgery
For IOL removal in this case, I utilized a small cannula I am developing—the Framula (Epsilon USA). The instrument incorporates a tip similar to that of a Donnenfeld spatula to help get under the anterior capsule, but the OVD deployed through a cannula opens downward to propagate into the capsular bag. In accordance with methodologies taught by the late Alan S. Crandall, MD, instead of simple rotation, the haptics are lifted, and their movement is assessed before they are rotated or amputated (for pearls on haptic removal with different lenses, see the sidebar). An OVD is then injected down the haptic-optic junction.
Troubleshooting Haptic Removal
In cases of fibrosis involving the terminal bulb of a haptic of an AcrySof/Clareon lens platform (Alcon), a bimanual technique is often required to strip the haptic and terminal bulb from the equator effectively (Figure A). In contrast, with the Tecnis platform (Johnson & Johnson Vision), fibrosis often presents precisely at the notch of the optic-haptic junction (Figure B). In this situation, it may be necessary to sever the fibrotic band before amputating the haptic. With an MX60E lens (Bausch + Lomb), fibrosis is often located within the eyelet (Figure C).

Figure. Examples of fibrosis encountered during haptic removal in an IOL exchange with different lens platforms. AcrySof/Clareon with fibrosis at the terminal bulb (A), Tecnis with fibrosis at the optic-haptic notch (B), and MX60E with fibrosis within the haptic islet (C).
The procedure proved to be straightforward. Fibrosis was evident superiorly where the anterior and posterior capsules were in direct contact (Figure 3).
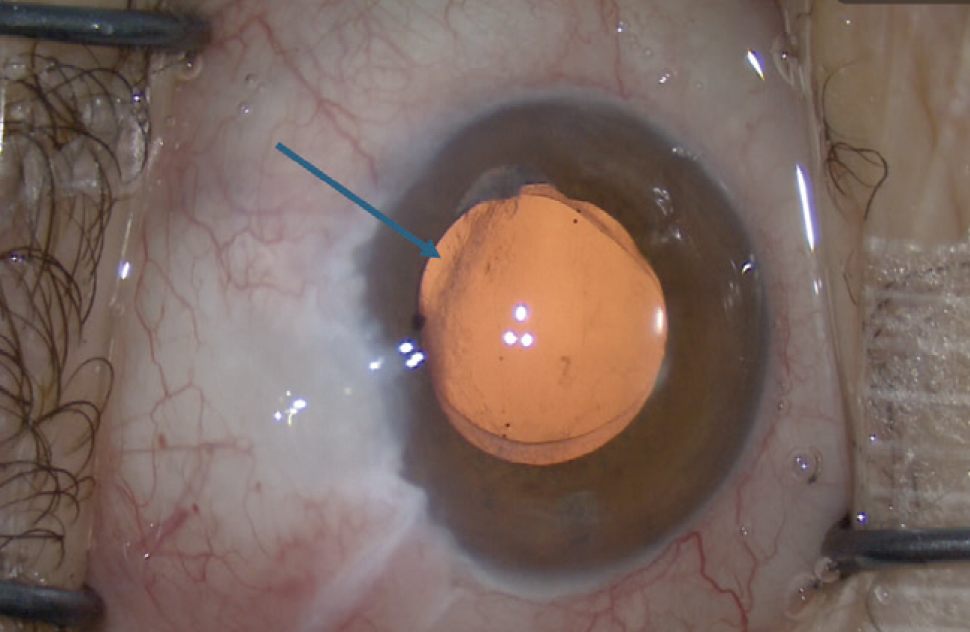
Figure 3. Fibrosis where the anterior and posterior capsules are in contact is visible at the superior aspect.
The capsular opening was expanded to the equator in preparation for implanting an LAL. Occasionally, an LAL may be inadvertently propelled outward at this stage. Should displacement occur, optic capture of the lens is a viable option. In this case, the anterior capsule was slightly larger than usual, so I was ready with a plan B, which would have involved a sulcus-fixated IOL.
The LAL was implanted in the sulcus and then carefully placed into the capsular bag bimanually to minimize stress on the zonules. The OVD was removed, and a small amount of washed and diluted triamcinolone acetonide was instilled to ensure there was no vitreous prolapse. Carbachol intraocular solution 0.01% (Miostat, Alcon) was administered to bring down the pupil.
To address the small iris defect, I employed a four-throw pupilloplasty. This technique—popularized by Amar Agarwal, MD—involves retrieving a loop of suture that was passed through the iris and wrapping the free end of the suture around the loop four times. I find this technique to be helpful in most eyes and particularly effective in highly pigmented eyes because of its ability to gather tissue tightly (Figure 4).1
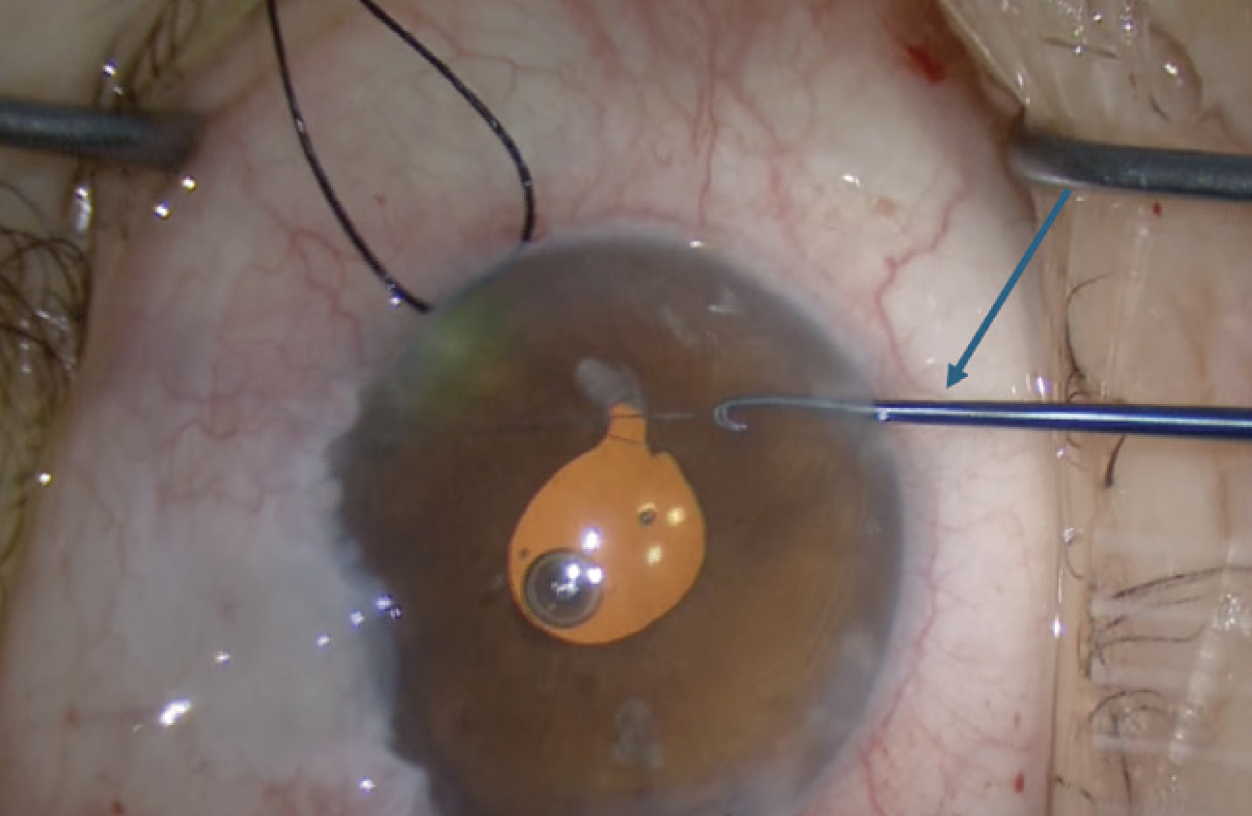
Figure 4. Intraoperative view of a single pass four-throw pupilloplasty using the iris retrieval hooks modified by Epsilon USA.
Outcome
Upon examination 3 weeks postoperatively, the glare was markedly improved, and the astigmatism was still stabilizing; however, the IOL haptics were not visible owing to the pupilloplasty (Figure 5). Clear visibility of both haptic optic junctions is crucial for precise postoperative light adjustments of an LAL. It was decided to release the pupilloplasty sutures surgically because argon laser treatment was not possible. Fortunately, both haptics of the IOL were clearly visible. The amount of astigmatism had changed from 2.40 D at an axis of 110º preoperatively to 3.00 D at an axis of approximately 50º, indicating instability (Figure 6). In situations like this, I find it advisable to wait until the eye settles (usually 4–6 weeks postoperatively) before performing a light adjustment.

Figure 5. The eye in an undilated (A) and dilated state (B) 3 weeks after surgery. The IOL haptics are not visible because of the small pupilloplasty.
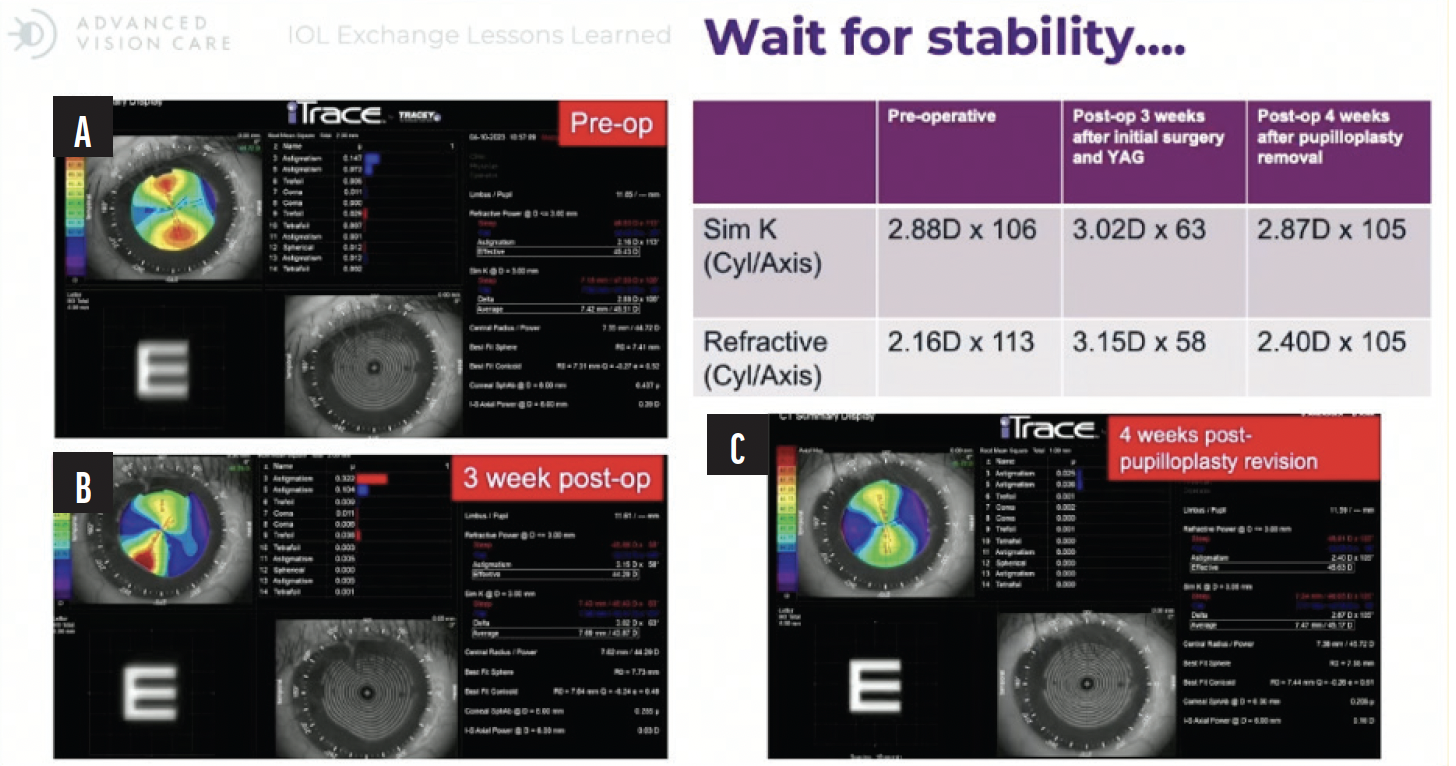
Figure 6. A composite of iTrace scans illustrating the changes in corneal astigmatism: preoperatively (A), 3 weeks postoperatively (B; demonstrating significant instability), and final stability 4 weeks after pupilloplasty revision (C; demonstrating stabilization). Abbreviations: Cyl, cylinder; Sim K, simulated keratometry.
After the cornea stabilized—confirmed by a return to the initial axis of 110º and magnitude of astigmatism—and following a successful Nd:YAG laser capsulotomy, light treatments were performed. The patient subsequently achieved 20/40-2 uncorrected distance visual acuity and J1 uncorrected near visual acuity (Figure 7).

Figure 7. Final postoperative visual outcomes following LAL treatment and second pupilloplasty.
LESSONS LEARNED
Suturing the iris after implanting an LAL was problematic primarily because it prevented the pupillary dilation required for postoperative UV light treatments, which are essential for adjusting the lens to refine a patient’s vision. The ability to fine-tune visual outcomes with the LAL postoperatively is a significant advantage of its use. Maintaining clear optical access during the postoperative period is crucial for achieving the intended refractive results. Prepare the patient for a potential Nd:YAG laser capsulotomy before adjustments.
When performing an IOL exchange with an LAL, the following actions are important:
- Avoid combining a pupilloplasty with an LAL IOL exchange (even if you believe it is small);
- Set realistic patient expectations preoperatively. Explain that postoperative recovery can be more prolonged (8–10 weeks) after LAL implantation compared to standard IOL procedures (5–6 weeks). Up to 4 weeks may be necessary to ensure the eye has healed properly and stabilized before further treatment is performed;
- Inform patients that an Nd:YAG laser capsulotomy is often required to address fibrosis and that a stable refraction is expected only at 2 weeks following this procedure; and
- State that, once refractive stability is confirmed, the light treatments necessary to fine-tune the LAL and lock in the desired refraction can be performed.
1. Narang P, Agarwal A. Single-pass four-throw pupilloplasty knot mechanics. J Refract Surg. 2019;35(3):207-208.




