

In 1992, Waring introduced the first standards for reporting refractive surgery outcomes with six graphs that show the accuracy, efficacy, safety, and stability of a surgical intervention.1 The number of graphs was later expanded to nine to address astigmatism.2 Similar guidelines were recently developed for lens-based refractive surgery, and the Journal of Refractive Surgery, Journal of Cataract & Refractive Surgery, and Cornea now require these standard graphs for submissions that evaluate refractive surgery outcomes. The AAO’s journal Ophthalmology also recommends the adoption of these graphs in their author guidelines.3
Adhering to these standards helps ensure that the results of various surgical techniques, studies, case reports, and series are formatted consistently and are readily comparable across different studies. Unfortunately, currently available web-based and standalone software solutions are often expensive and require manual data entry or calculations, all of which limits their widespread adoption.
A lack of specialized, free software that can automate the production of standard graphs has hampered ophthalmologists’ ability to understand the results of surgical interventions empirically and hindered efficient comparative analyses in the field. In response to these challenges, we developed mEYEstro, a tool to simplify and enhance the accuracy, reproducibility, and standardization of refractive surgery outcomes analysis.
SOFTWARE OVERVIEW
Our aim with mEYEstro is to transform the complexity of refractive surgery data analysis into a seamless, user-friendly experience. Designed specifically for corneal and intraocular procedures, this tool offers automated generation of journal-standard graphs and robust statistical analysis within 30 seconds and with minimal user input. The mEYEstro software has been fully tested, and its results were reported in a peer-reviewed journal.4
Core Functionality
The software currently produces 11 standard graphs that fall into four categories (Table). Percent proportions, means, standard deviations, effect sizes, and P values are calculated and displayed on each graph. All graphs can easily be exported as high-resolution images to illustrate scientific manuscripts and presentations (Figure).
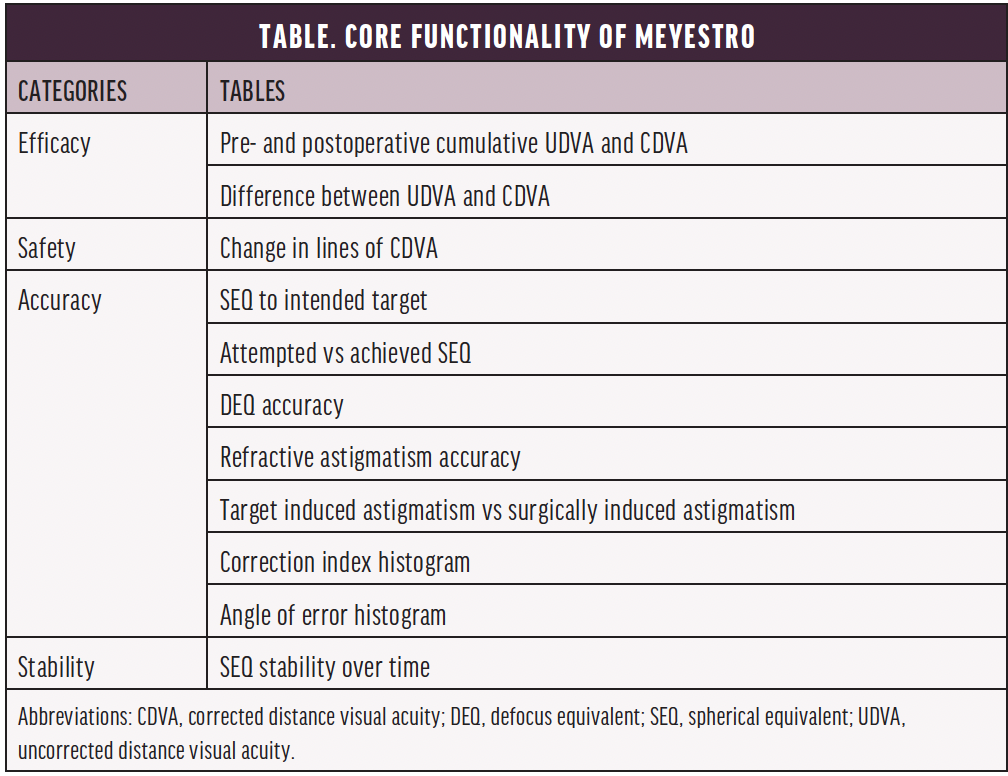

Figure. Graphs were automatically generated by mEYEstro from the provided trial 1 dataset. The first simulated trial dataset (trial 1) included two Excel files (groups A and B) and investigated the outcomes of a laser vision correction contralateral eye study comparing two treatment protocols in hyperopic eyes with astigmatism.
Program Workflow
The software is controlled with a few simple steps. Users begin by choosing the type of refractive surgery (eg, laser vision correction, refractive lens exchange), the type of study (single group, unpaired groups, paired groups), the name of the groups, and the color of the graphs. Next, they choose the Microsoft Excel (Microsoft) data file that will be imported for each group. The selected graphs and statistical analyses are then automatically generated and saved in a folder.
PRACTICAL BENEFITS
Refractive surgery analyses are extensive, and subtle nuances cannot be fully captured in a single graphical display. Instead, several graphs are used to answer questions about the efficacy, safety, accuracy, and stability of a procedure. This depth of analysis helps elucidate the cause of inaccurate outcomes and evaluate the effectiveness of treatment.
By simplifying data analysis, this tool can help clinicians and surgeons understand and improve on their outcomes, providing added benefits to patients. The high-resolution images the software generates are appropriate for academic presentations and publications, which makes it easier to share findings with colleagues. Because mEYEstro is free to use, it is more accessible than paid alternatives. Further information on mEYEstro and our research may be found at www.refractivesurgery.ca. The software may be downloaded here.
1. Waring GO. Standardized data collection and reporting for refractive surgery. Refract Corneal Surg. 1992;8:1-42.
2. Reinstein DZ, Archer TJ, Randleman JB. JRS standard for reporting astigmatism outcomes of refractive surgery. J Refract Surg. 2014;30(10):654-659.
3. Author information. Ophthalmology. Accessed May 31, 2024. www.aaojournal.org/content/authorinfo
4. Gauvin M, Wallerstein A. mEYEstro software: an automatic tool for standardized refractive surgery outcomes reporting. BMC Ophthalmol. 2023;23(1):171.




