During the past decade, improved diagnostics and advanced-generation IOL formulas have increased the accuracy of IOL power calculations, yet refractive surprises still occur. Measurement variability, ocular surface disease, prior refractive surgery, and surgeon-specific factors introduce noise that traditional static calculators were not designed to manage. The ever-increasing complexity of the data we now obtain through biometry, tomography, wavefront analysis, tear film analysis, and OCT, among others, compounds the challenge.
AT A GLANCE
- Cloud-based surgical planning platforms are moving from organizing measurements to interpreting them.
- AI is beginning to guide preoperative decisions. Platforms can now predict refractive outcomes or suggest the most appropriate traditional formula for an eye’s biometric profile.
- As outcomes databases grow, AI could learn surgeon- and eye-specific patterns (eg, effective lens position behavior) to refine recommendations.
The latest generation of cloud-based surgical planning platforms represents a first step toward organizing these data so they can be used more effectively.
CURRENT PLATFORMS
Platforms such as Eyetelligence (Bausch + Lomb), SmartCataract (Alcon), and Veracity (Carl Zeiss Meditec) integrate data from multiple diagnostic devices by pulling measurements directly from those devices and organizing them in the cloud to create the infrastructure on which future AI features can build. Many platforms also integrate with electronic health record systems, improving interoperability, although the depth and breadth of electronic health record connectivity can vary by platform and practice environment.
Workflow Efficiency and Error Reduction
A key advantage of the latest surgical planning platforms is improved efficiency and fewer transcription errors. Historically, running a case through multiple advanced IOL formulas often meant visiting several websites and reentering the same data repeatedly. The process was tedious, slow, and prone to error.
From Static Calculators to Adaptive Planning
Current platforms allow surgeons to compare data across devices, add customized inputs, and average measurements when appropriate. Axial length, anterior and posterior corneal data, refraction, and prior outcomes can be entered into a planning environment that is increasingly adaptive rather than static. The consolidated dataset can then be run through multiple advanced IOL formulas quickly, making IOL calculation more precise and expanding the options available to refine lens selection.
HOW AI IS BEING APPLIED TODAY
Phase 1: Solve the Data Problem
Structured data capture is the foundation on which meaningful AI must be built. The first step was creating a centralized, safe, and secure data repository. Platforms such as SmartCataract, Veracity, and Eyetelligence have focused on this phase 1 work by aggregating measurements, reducing manual transcription, and creating a consistent planning workspace.
By solving the data problem first, cloud-based planning platforms are well positioned to support more advanced AI-driven decision support as their capabilities evolve. Once the data infrastructure is in place, AI becomes a practical next step.
Phase 2: Early Clinical Decision Support
Still in its infancy, this second phase focuses on determining how best to apply AI to support the surgeon without replacing clinical judgment. In this context, the key distinction is between connectivity and workflow (phase 1) and preoperative, AI-driven decision support (phase 2), such as predictive modeling or formula guidance.
To date, clear, preoperative phase 2 steps have been taken with two platforms. Veracity’s AI-based IOL calculator uses data-driven modeling to generate refractive predictions alongside traditional formulas (Figure 1). Eyetelligence applies AI differently; the platform uses biometric patterns to help determine which standard IOL formula may be most appropriate for a given eye instead of replacing formulas outright (Figure 2).
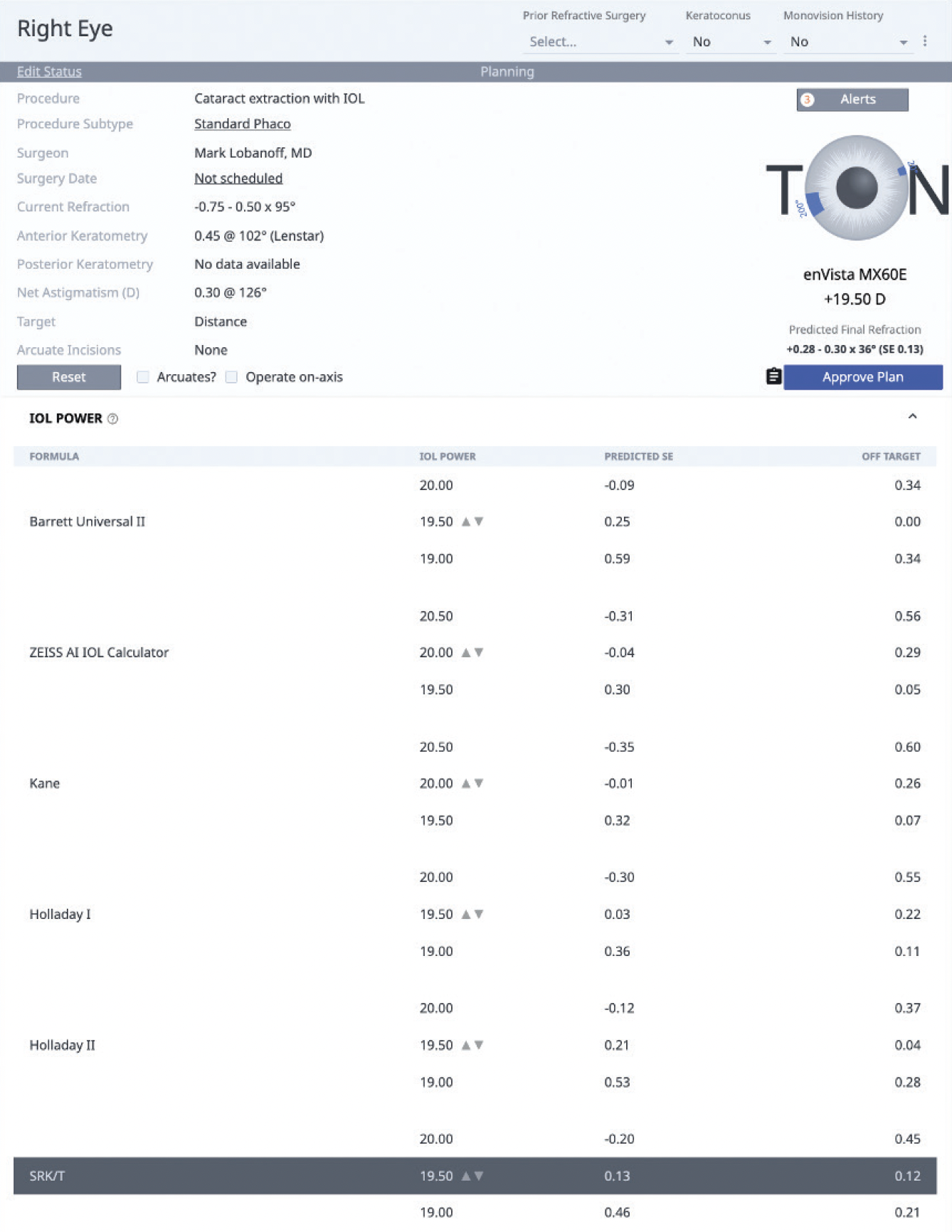
Figure 1. Veracity display of an AI–based IOL calculator output, with data-driven refractive predictions shown alongside traditional formula results.

Figure 2. Eyetelligence AI–assisted tool that recommends an IOL formula based on an eye’s biometric profile.
CUSTOMIZATION AT EVERY LEVEL
AI has the potential to customize IOL planning. In the past, surgeons asked a simple question: “Which formula should I use?” Modern platforms ask, “What do eyes exactly like this eye, with this surgeon, tend to do?” As each surgeon’s database of cases grows in the cloud, AI may be able to learn the effective lens position patterns associated with that surgeon and technique. Over time, this could enable the creation of surgeon- and clinic-specific lens constants.
Perhaps in the future, an AI model could learn that using the anterior chamber depth from one biometer and the keratometry values from another produces the best outcomes for a given surgeon. The software could evaluate large numbers of associations, identify those that are relevant, and improve performance through back-testing against outcomes. The benefit might be modest for routine, average eyes but substantial for nonaverage eyes, for which small assumptions can have outsized refractive consequences.
REAL-WORLD SURGICAL APPLICATIONS OF AI
Measurement Variability
Measurement variability remains a common challenge. AI does not correct poor-quality inputs, but it can reduce the penalty of imperfect data by recognizing patterns across multiple diagnostic sources. It can also flag measurements that appear suspicious or internally inconsistent. In some settings, AI can identify that one device’s measurements are less reliable than another’s and weight the inputs accordingly. This approach might lessen the influence of outlier values, particularly in premium IOL candidates.
Premium IOL Risk Stratification
AI might also improve premium IOL risk stratification. By identifying eyes at increased risk of residual refractive error or postoperative astigmatism, AI can support more nuanced lens selection and strengthen preoperative patient counseling.
WHAT AI STILL DOES POORLY
Garbage in, Garbage out
AI-powered platforms are limited by the quantity and quality of the data they ingest. Inaccurate postoperative refractions, inconsistent data entry, and systematic measurement bias can degrade performance.
The Risk of Overautomation
If surgeons disengage from critical thinking, outcomes could suffer. AI should narrow the decision space, not make the decision.
AI can be misled and may generate erroneous conclusions. Surgeons should review each analysis and confirm that it aligns with their clinical assessment. At least one platform allows the surgeon to apply a stamp to indicate review and approval of the surgical plan (Figure 3).

Figure 3. Eyetelligence interface showing a surgeon-applied stamp indicating review and approval of the surgical plan.
CONCLUSION
AI-powered surgical planning platforms are not replacing surgeons or IOL formulas. Instead, they are improving workflow by functioning as a digital copilot that integrates data, learns from outcomes, and helps manage increasing complexity. The best outcomes occur when AI manages complexity and surgeons apply their judgment. Key challenges include not only developing robust models but also meeting expectations for transparency, explainability, and audit trails.