CASE PRESENTATION
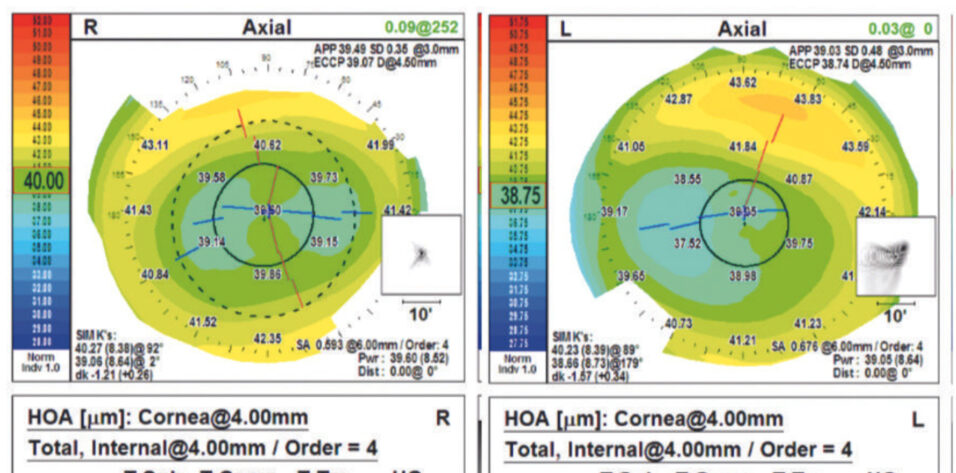
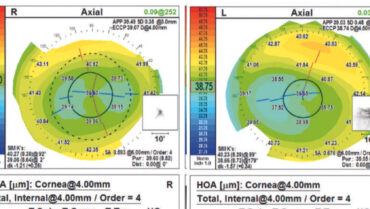
A 30-year-old man presents for a refractive surgery screening. The patient’s history is unremarkable. He has stable refractions of -3.50 -1.50 x 89° = 1.25 (decimal) OD and -4.00 -1.50 x 93° = 1.25 OS. Measurements with the Orbscan (Bausch + Lomb; Figure 1), including with the Screening Corneal Objective Risk of Ectasia (SCORE) Analyzer software (Figure 2), are normal (values of -0.1 OD and -0.6 OS).
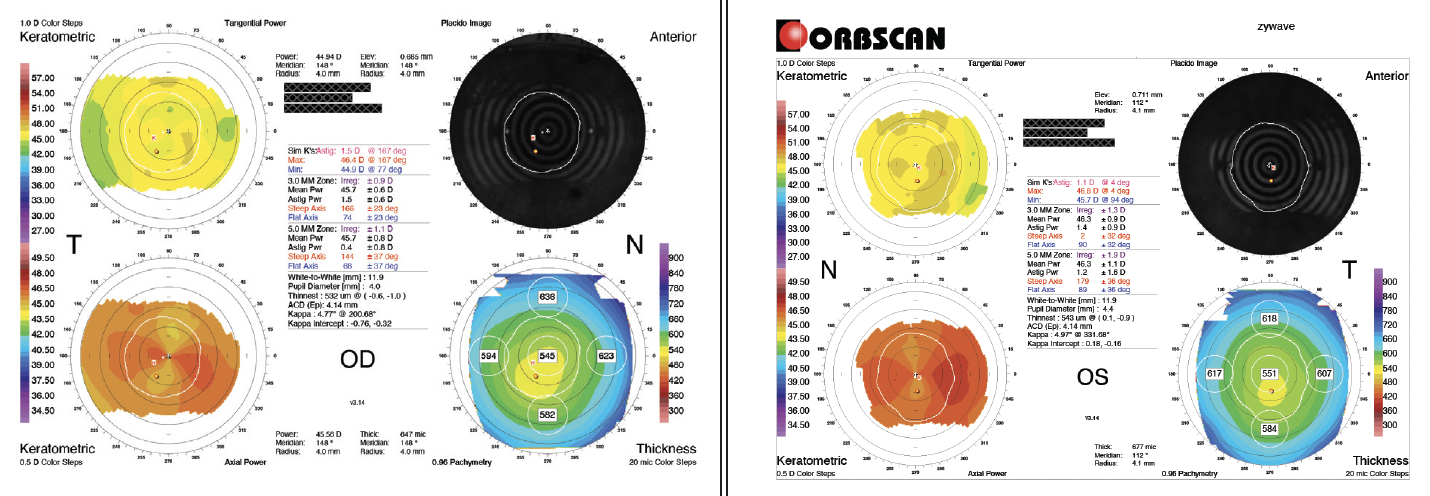
Figure 1. Preoperative measurements of both eyes with the Orbscan appear to be normal. Topography is regular without significant inferior steepening or thinning. There is no asymmetry between the eyes.
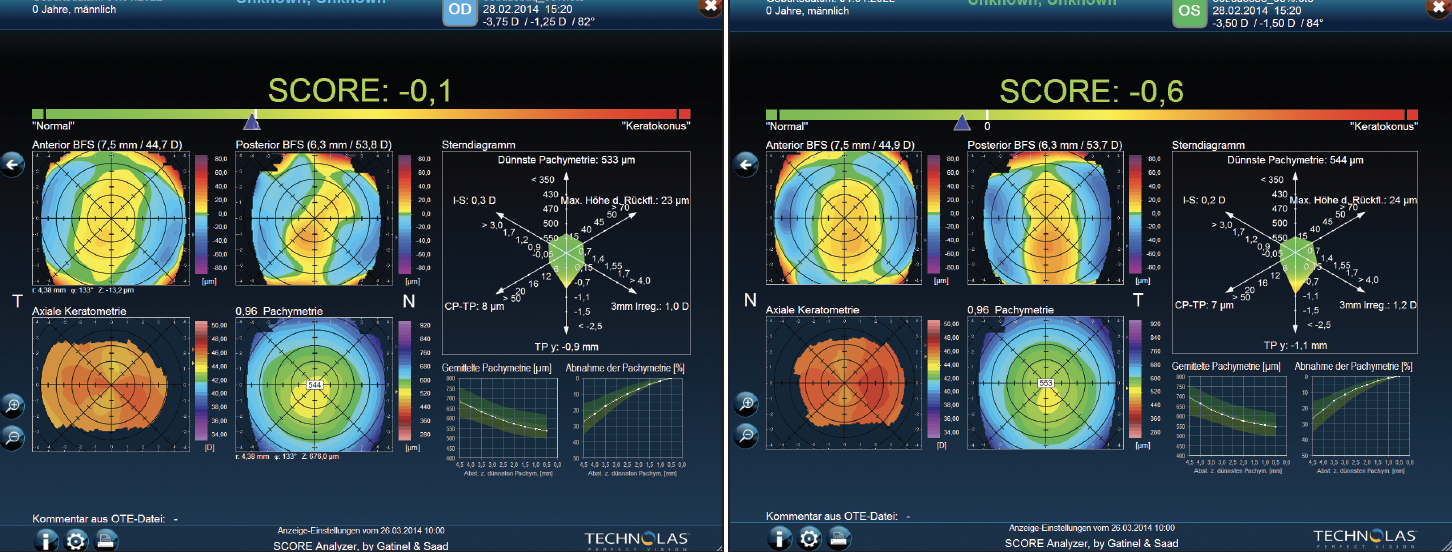
Figure 2. Automatic evaluation with the SCORE Analyzer software produces values within normal limits.
What form of treatment would you recommend? Would you obtain additional diagnostic testing preoperatively? If so, how would the results inform your recommendation?
—Case prepared by Suphi Taneri, MD, FEBOS-CR

JOHN F. DOANE, MD, FACS
The patient’s stable refraction and adequate corneal thickness notwithstanding, the against-the-rule (ATR) topographic pattern is of concern. The skewed ends of the dumbbell, which essentially turn downward to kiss at the 270º meridian, have the appearance of pellucid marginal degeneration (PMD). My thoughts on this pattern solidified years ago when Howard V. Gimbel, MD, MPH, FRCSC, and John van Westenbrugge, MD, FRCSC, of the Gimbel Eye Center in Calgary, Canada, described treating ATR astigmatism patterns with laser vision correction.
Measurements with the Atlas 9000 Corneal Topography System (Carl Zeiss Meditec) and corneal OCT scans would be obtained. The goal would be to determine if the PMD pattern can be confirmed and if a pattern of abnormal thickness is present at the epithelial surface. I would inquire about a family history of corneal disease such as keratoconus and PMD. I would also ask the patient whether any family members have undergone laser vision correction and, if so, how they did postoperatively.
Based on the case presentation, I would counsel the patient against undergoing a lamellar procedure in favor of bilateral PRK. After surgery, he would be monitored annually with refraction, topography, and OCT imaging and advised to return sooner if a concern arises. CXL would be an option if there is any indication of postoperative ectasia.

DAMIEN GATINEL, MD, PHD
Topographic findings present some compelling reasons to recommend a surface laser technique rather than LASIK or laser-assisted lenticule extraction. Inferior decentration of the thinnest point of the cornea, ATR corneal astigmatism, and increased elevation of the posterior surface against the best fit sphere inferiorly—all suggest forme fruste keratoconus.1,2
In my experience, these topographic patterns are associated with chronic, excessive eye rubbing rather than primary pathology. Friction causes paracentral thinning and vertical weakening of the corneal wall, which, through a torque effect, can increase horizontal steepening (hence the induction of or increase in ATR astigmatism and the lower decentration of the thinnest point). In this context, the SCORE Analyzer software, which I developed with Alain Saad, MD, can be useful. It detects values close to the positivity threshold. The software’s radar map also reveals indices that are near or slightly beyond the anomaly threshold.
Potential causes of excessive ocular friction such as allergy, blepharitis, and discomfort associated with contact lens wear would be evaluated. He would be asked about his sleeping position because it is frequently associated with irregular topography. He would also be advised to avoid rubbing his eyes excessively.
PRK does not pose a risk of corneal ectasia when performed on eyes with thin or irregular corneas.3 The procedure can also improve eye hygiene by eliminating patients’ need for contact lenses and decreasing corneal sensitivity, thereby reducing their desire to rub their eyes.


DHIVYA ASHOK KUMAR, MD, FRCS, FICO, FAICO, AND PRIYA NARANG, MS
The AI-based SCORE Analyzer assists with the early diagnosis and follow-up of corneal ectasia.4 The tool’s radar map uses six of the most discriminant topographic indices to calculate a SCORE Analyzer value. The analysis of this patient seems to be negative for ectasia, but details on higher-order aberrations (HOAs) are not mentioned.
Scheimpflug imaging would be obtained to determine the total and corneal HOA root mean square values. Considering the patient’s age, some physical changes to the crystalline lenses might have occurred. He would be counseled that retaining slight myopia is likely to benefit him as he ages. If the crystalline lenses are clear, HOA root mean square values are within 0.3 µm, and the patient demonstrates refractive stability for more than 6 months, SMILE would be offered.5
Although the SCORE Analyzer has demonstrated good sensitivity and specificity in the detection of forme fruste keratoconus, false negatives have been reported.6 Scheimpflug imaging can improve the accuracy of the aberration profile and the detection of changes in posterior corneal elevation. The Pentacam (Oculus Optikgeräte) has demonstrated 98.6% sensitivity and 100% specificity with an area under the curve of 0.999.7 The device would therefore be used to evaluate the patient for specific posterior corneal changes and HOAs before laser-assisted lenticule extraction to improve the functional outcome. Regular postoperative follow-up would be advised.

ARTEMIS MATSOU, MD, MRCP(UK), FEBO, PGDIP CRS
The patient’s refractive error seems straightforward, and his SCORE Analyzer values appear to be normal. The SCORE Analyzer value in the right eye is only slightly negative (-0.1). This is not a red flag but warrants careful consideration. The radar map reveals borderline or suspicious findings: vertical displacement of the thinnest point (-0.9 mm), posterior elevation, and 3-mm irregularity. The SCORE Analyzer value for the left eye is also normal at -0.6. That said, vertical displacement of the thinnest point (-1.1 mm) is more pronounced in this eye, increasing the risk profile. At 1.20 D, the 3-mm irregularity is also higher.
The quad map of the right eye shows 3- and 5-mm irregularities of ±0.90 and ±1.10 D, respectively, which are not quite abnormal but hint at asymmetric astigmatism when combined with the SCORE Analyzer values. The 3- and 5-mm irregularities of ±1.30 and ±1.90 D in the left eye are higher, consistent with the eye’s higher risk profile. These values signal that surgery should be approached with caution.
Additional diagnostic tests would be obtained. Epithelial thickness mapping could reveal subtle corneal ectasia that might be difficult to detect with standard topographic/tomographic imaging. For such evaluations, I favor the Pentacam and anterior segment OCT with the MS39 (CSO), which integrates epithelial thickness mapping into its keratoconus detection algorithm. An assessment of corneal biomechanics, such as with the Corvis ST (Oculus Optikgeräte), could also be useful.
If additional testing supports my initial suspicion of early ectasia, I would counsel the patient against corneal refractive surgery as a first-line intervention. Implantation of an EVO ICL (STAAR Surgical) may be an option if the patient’s refractions are stable and he meets the safety criteria. If the additional testing does not confirm keratoconus but suspicion from the initial assessment lingers, PRK may be a safer choice than LASIK.

WHAT I DID: SUPHI TANERI, MD, FEBOS-CR
The patient presented for a free screening at our clinic in February 2014. His refraction was stable and well within the range for laser vision correction. Because the patient history was unremarkable and Orbscan measurements were normal, the technician deemed him to be a suitable candidate for laser vision correction and recommended he receive a more comprehensive examination and repeat refraction on another day. Instead, the patient underwent LASIK at another clinic. At 2.5 months postoperatively, his BCVA was 1.25 OD with a manifest refraction of 0.00 -0.25 x 90° and 0.80 OS with a manifest refraction of 0.00 -0.25 x 135°.
The patient was satisfied with his results for several years. In early 2020, he noticed that his vision was deteriorating. In June 2021, increasing bilateral astigmatism was detected, and the patient was referred to our practice.
He had no known allergies or systemic disease and stated that he still did not rub his eyes. On examination, his BCVA was +2.00 -5.00 x 83° = 0.80 OD and +0.50 -4.50 x 84° = 1.25 OS. Scheimpflug tomography detected bilateral corneal ectasia, with thinning and protrusion in the inferotemporal quadrant typical of a virgin keratoconic cornea (Figure 3).
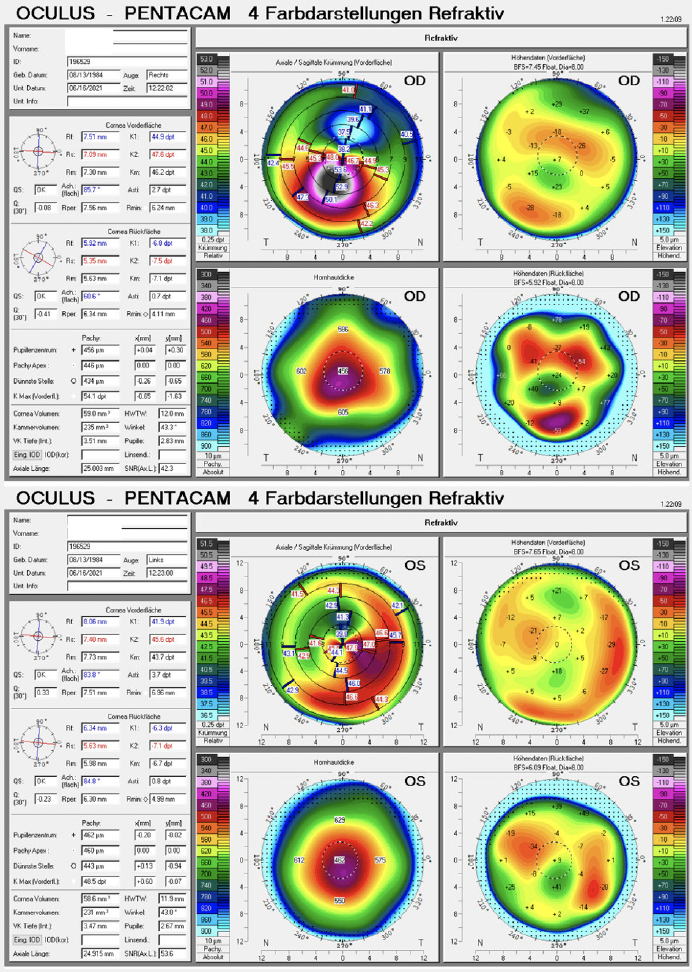
Figure 3. Scheimpflug tomography with the Pentacam shows thinning and irregular steepening of the cornea in each eye 7 years after LASIK.
Pachymetry with the Cirrus 5000 (Carl Zeiss Meditec; Figure 4) found a perfectly centered LASIK ablation in each eye. Epithelial masking around each cone was not located at the center but inferotemporally. The panelists are therefore arguably correct that the eyes had subclinical keratoconus preoperatively despite the seemingly normal Orbscan measurements. As the panelists note, additional testing of the eyes’ biomechanical properties and epithelial thickness might have detected the condition preoperatively. (Recently, my colleagues and I participated in a study to improve the automatic analysis of combined Pentacam and Corvis ST data.8)
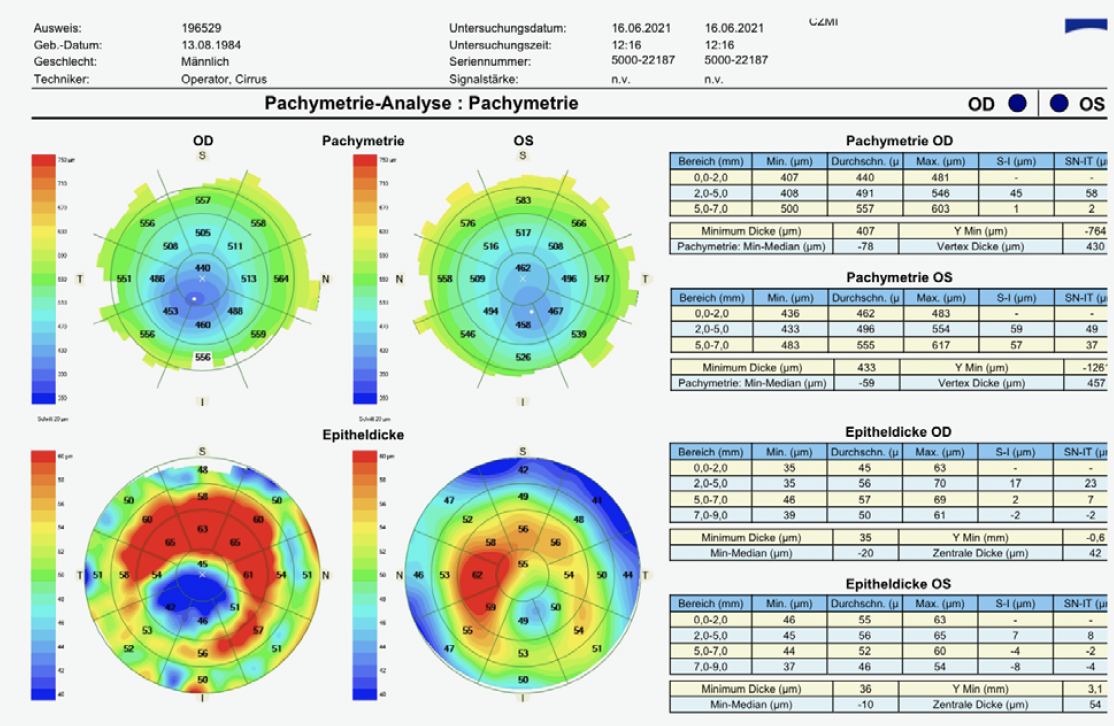
Figure 4. Pachymetric analysis with OCT of the total cornea (upper maps) and the epithelium only (lower maps) 7 years after LASIK. The ablation in each eye appears to have been perfectly centered, as shown by the central light blue area of corneal thinning. The maps, however, reveal inferior temporal thinning of the total cornea within the centered area of laser ablation combined with masking of the cone by apical thinning and thickening of the surrounding epithelium. These findings resemble a naturally occurring ectasia as is seen with keratoconus.
The patient underwent CXL after laser abrasion in both eyes. After treatment, his BCVA was +0.75 -3.50 x 85° = 1.25 OD and 0.00 -2.75 x 81° = 1.00 OS. Tomography measurements have been stable for 2 years.
1. Saad A, Gatinel D. Topographic and tomographic properties of forme fruste keratoconus corneas. Invest Ophthalmol Vis Sci. 2010;51(11):5546-5555.
2. Saad A, Guilbert E, Gatinel D. Corneal enantiomorphism in normal and keratoconic eyes. J Refract Surg. 2014;30(8):542-547.
3. Guedj M, Saad A, Audureau E, Gatinel D. Photorefractive keratectomy in patients with suspected keratoconus: five-year follow-up. J Cataract Refract Surg. 2013;39(1):66-73.
4. Saad A, Gatinel D. Validation of a new scoring system for the detection of early forme of keratoconus. Int J Kerat Ect Cor Dis. 2012;1(2):100-108.
5. Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism. Graefes Arch Clin Exp Ophthalmol. 2016;254(2):399-405.
6. Chan C, Ang M, Saad A, et al. Validation of an objective scoring system for forme fruste keratoconus detection and post-LASIK ectasia risk assessment in Asian eyes. Cornea. 2015;34(9):996-1004.
7. Heidari Z, Hashemi H, Mohammadpour M, Amanzadeh K, Fotouhi A. Evaluation of corneal topographic, tomographic and biomechanical indices for detecting clinical and subclinical keratoconus: a comprehensive three-device study. Int J Ophthalmol. 2021;14(2):228-239.
8. Ambrósio R Jr, Machado AP, Leão E, et al. Optimized artificial intelligence for enhanced ectasia detection using Scheimpflug-based corneal tomography and biomechanical data. Am J Ophthalmol. 2023;251:126-142.