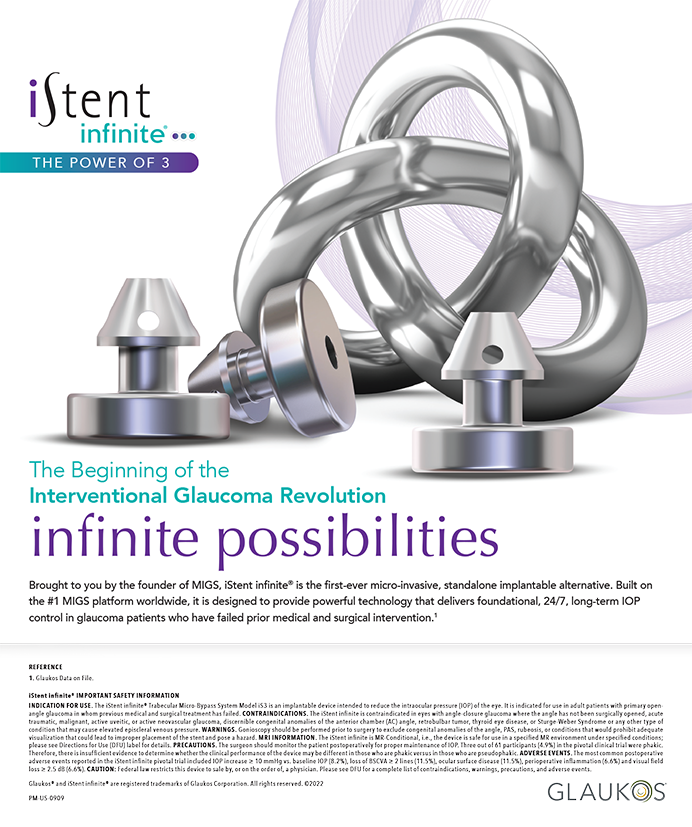
The prevalence of preoperative astigmatism in cataract surgery patients is well described (Figure 1).1 Expressed another way, 60% of cataract patients have at least 0.50 D of astigmatism, and 40% have at least 0.75 D (Figure 2). This is pertinent because the widely accepted threshold for the surgical correction of astigmatism is 0.75 D. The surgical correction of very small amounts of astigmatism (eg, ≤ 0.50 D) generally is not predictable. The same is true of irregular astigmatism. Many factors can interfere, such as dry eye disease and age-related corneal changes.
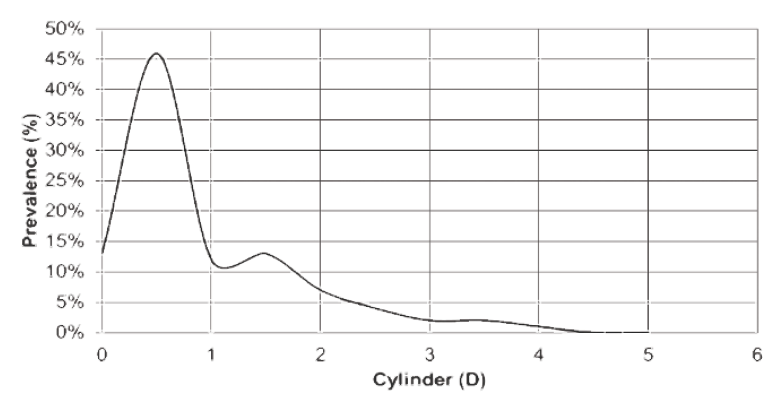
Figure 1. Prevalence of preoperative astigmatism in cataract surgery patients.
Figure 2. Cumulative prevalence of preoperative astigmatism in cataract surgery patients.
The ease of use, predictability, and rapid recovery associated with toric IOLs make them preferable to corneal relaxing incisions—even when a femtosecond laser is used—for most patients with clinically significant regular astigmatism.2-5 The AAO’s EyeWiki states that “standard toric IOLs are available in cylinder powers of 1.50 D to 6.00 D. They are usually intended for regular corneal astigmatism in a range from 0.75 D to 4.75 D, and extended series or customized IOLs are available to achieve higher cylindrical power. Toric IOLs are available as monofocal and multifocal lenses.”6
According to the directions for use for one toric IOL, “the clinical study for the Tecnis Toric 1-Piece IOL [Johnson & Johnson Vision] did not show evidence of effectiveness for the treatment of preoperative corneal astigmatism of less than one diopter.”7 There is a role for relaxing incisions for low cylinder powers and for postoperative enhancements. Sometimes, adjustment of the cataract incision alleviates small amounts of astigmatism without the need for relaxing incisions.5
Medicare Regulations
Medicare has applied the deluxe8 concept to presbyopia- and astigmatism-correcting IOLs. This permits providers (ie, hospitals and ambulatory surgery centers) to collect an extra fee from beneficiaries for the noncovered aspect of an otherwise covered IOL. At the same time, CMS also agreed to allow the surgeon to charge the beneficiary for additional, clearly identifiable, and medically appropriate services to manage astigmatism. These may include one or more of the following services:
- Refraction and/or wavefront aberrometry (in-office and/or in the OR) to identify lower- and higher-order aberrations;
- Corneal topography for preexisting regular astigmatism;
- Corneal pachymetry for planning arcuate corneal incisions;
- Scanning computerized ophthalmic diagnostic imaging of the macula to screen for possible disease;
- Marking the axis of astigmatism on the eye at the outset of cataract surgery;
- Use of a femtosecond laser to perform arcuate corneal incisions for the surgical correction of clinically significant, regular astigmatism; and
- Enhancement with refractive keratoplasty to correct residual astigmatism (eg, astigmatic keratotomy, limbal relaxing incision, corneal relaxing incision, PRK, LASIK).
Surgeons need to construct individual protocols for additional refractive services and determine which are medically appropriate on a case-by-case basis. They should establish a reasonable fee for the refractive package that takes into consideration the services included and local market conditions. The hospital outpatient department or ambulatory surgery center will follow a similar approach to establish its noncovered facility fee for the IOL upgrade, additional equipment not used in routine cataract surgery, and enhancements.9,10
Operational Challenges
Important questions about reimbursement are engendered by the surgical correction of astigmatism. Patients cannot be expected to pay extra for additional noncovered items and services associated with refractive cataract surgery unless they have a clear understanding of their financial responsibility. To cover all the bases and avoid allegations of balance billing, providers should educate third-party payers before surgery and get written authorization to bill patients for noncovered items and services. The CMS ruling for astigmatism-correcting IOLs11 and refractive keratoplasty12 makes clear the agency’s policies for Medicare patients; other payers generally, but not always, follow suit.
A number of practice management challenges may arise after the surgical correction of astigmatism:
- Ex post facto patient complaints about the out-of-pocket expense;
- Patient dissatisfaction with outcomes;
- Unexpected reimbursement for refractive surgery by a third-party payer; and
- Postprocedural investigation by payers and state and federal agencies in response to complaints.
From our experience assisting clients, my colleagues and I have learned several important principles to preempt or mitigate these difficulties. First, preoperative screening and diagnostic testing are foundational to the identification of suitable candidates. Second, thorough informed consent is essential to setting realistic expectations. Third, a clear, detailed, written explanation of out-of-pocket fees on appropriate forms is crucial. The coverage plan dictates how to proceed. An Advance Beneficiary Notice of Noncoverage is used for Medicare Part B.13 A Notice of Exclusion from Health Benefits is used for non-Medicare payers.14 The predetermination of benefits process and associated forms from the Medicare Advantage Organization should be used for Part C Medicare.15 Finally, guidance from the AAO, ASCRS,16 CMS,17 and Office of the Inspector General18 for the use of a femtosecond laser and the surgical correction of astigmatism should be followed.
Significantly, CMS guidance on laser cataract surgery issued in November 2012 made clear that the use of a femtosecond laser to perform portions of the cataract procedure, such as the capsulotomy, is covered as part of medically necessary cataract surgery and that the beneficiary is not financially responsible. CMS added that this guidance does not change the longstanding policy on refractive keratoplasty.
Conclusion
Cataract surgery is an immensely successful procedure. Improving on that success is difficult. Minimizing residual refractive error, particularly astigmatism, is one way. Outcomes with toric IOLs are very good, usually better than with corneal relaxing incisions created with or without a laser. Nevertheless, there remains a place for keratotomy for low cylinder powers and postoperative enhancements. Despite reduced Medicare payment rates for cataract surgery, surgeons are seeing growing numbers of patients with cataracts. About 40% of them have 0.75 D or more of clinically significant, regular astigmatism and could benefit from and pay out of pocket for its surgical correction.
1. Ferrer-Blasco T, Montes-Mico R, Peixoto-de-Matos SC, et al. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70-75.
2. Mingo-Botin D, Munoz-Negrete, FJ, et al. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36(10):1700-1708.
3. Leon P, Pastore MR, Zanei A, et al. Correction of low corneal astigmatism in cataract surgery. Int J Ophthalmol. 2015;8(4):719-724.
4. Nunez, MX, Henriquez MA, Escaf LJ, et al. Consensus on the management of astigmatism in cataract surgery. Clin Ophthalmol. 2019;13:311-324.
5. Brennan K. Astigmatism: How low can you go? Review of Ophthalmology. October 14, 2018. Accessed January 10, 2021. https://www.reviewofophthalmology.com/article/astigmatism-how-low-can-you-go
6. Naranjo, A, Patel, AS. Toric IOLs. AAO EyeWiki. August 26, 2019. Accessed January 10, 2021. https://eyewiki.aao.org/Toric_IOLs#:~:text=Standard%20toric%20IOLs%20are%20available,as%20monofocal%20and%20multifocal%20lenses
7. The TECNIS Toric IOL patient information brochure. FDA. Accessed January 10, 2021. https://www.accessdata.fda.gov/cdrh_docs/pdf/P980040S039c.pdf
8. Medicare claims processing manual chapter 20 – durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS). CMS. Accessed January 10, 2021. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c20.pdf
9. Corcoran KJ. Compliance and patient-shared billing. Paper presented at the 2020 ASCRS Virtual Annual Meeting. October 10, 2020.
10. Medicare reimbursement for Tecnis Symfony IOLs.Corcoran Consulting Group. January 2017. Accessed January 10, 2021. https://www.corcoranccg.com/digital_files/monographs/Symfony%20AMO_012617.pdf
11. CMS ruling No. CMS-1536-R, January 22, 2007. CMS. Accessed January 10, 2021. https://www.cms.gov/Regulations-and-Guidance/Guidance/Rulings/downloads/CMS1536R.pdf
12. CMS national coverage determination §80.7 refractive keratoplasty. CMS. Accessed January 10, 2021. https://www.cms.gov/medicare-coverage-database/details/ncd-details.aspx?NCDId=72&ncdver=1&bc=BAAAEAAAAAAA&
13. CMS form instructions advance beneficiary notice of non-coverage (ABN), CMS-R-131 (Expires 06/2023). CMS. Accessed January 10, 2021. https://www.cms.gov/Medicare/Medicare-General-Information/BNI/ABN
14. Forms. Corcoran Consulting Group. Accessed January 10, 2021. www.corcoranccg.com/products/forms
15. Medicare claims processing manual, chapter 30, §50.3 ABN Scope. CMS. Accessed January 10, 2021. https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c30.pdf
16. AAO, ASCRS guidance RE medicare billing, laser cataract surgery. AAO. January 30, 2012. Accessed January 10, 2021. https://www.aao.org/newsroom/news-releases/detail/aao-ascrs-guidance-re-medicare-billing-laser-catar
17. Laser-assisted cataract surgery and CMS ruling 05-01 and 1536-R. CMS. November 16, 2012. Accessed January 10, 2021.
https://www.cms.gov/medicare/medicare-fee-for-service-payment/ascpayment/downloads/cms-pc-ac-iol-laser-guidance.pdf Accessed 01/10/21
18. OIG Advisory Opinion No. 11-14. Accessed January 10, 2021. https://oig.hhs.gov/fraud/docs/advisoryopinions/2011/advopn11-14.pdf