CASE PRESENTATION
A 58-year-old man is referred for cataract surgery on his left eye. The patient reports that he sustained a traumatic eye injury and underwent surgical repair at age 2. He says he had “OK” vision when he was very young but states that, for the past 30 to 40 years, he has had no usable vision in the left eye. He states that his vision recently became unacceptably poor and expresses interest in options to improve it. The patient has been evaluated by two other cataract surgeons, both of whom told him that the risk of surgery is unacceptably high and that he is unlikely to recover usable vision. He is willing to accept the fact that he has a poorly sighted left eye but asks if an improvement is possible.
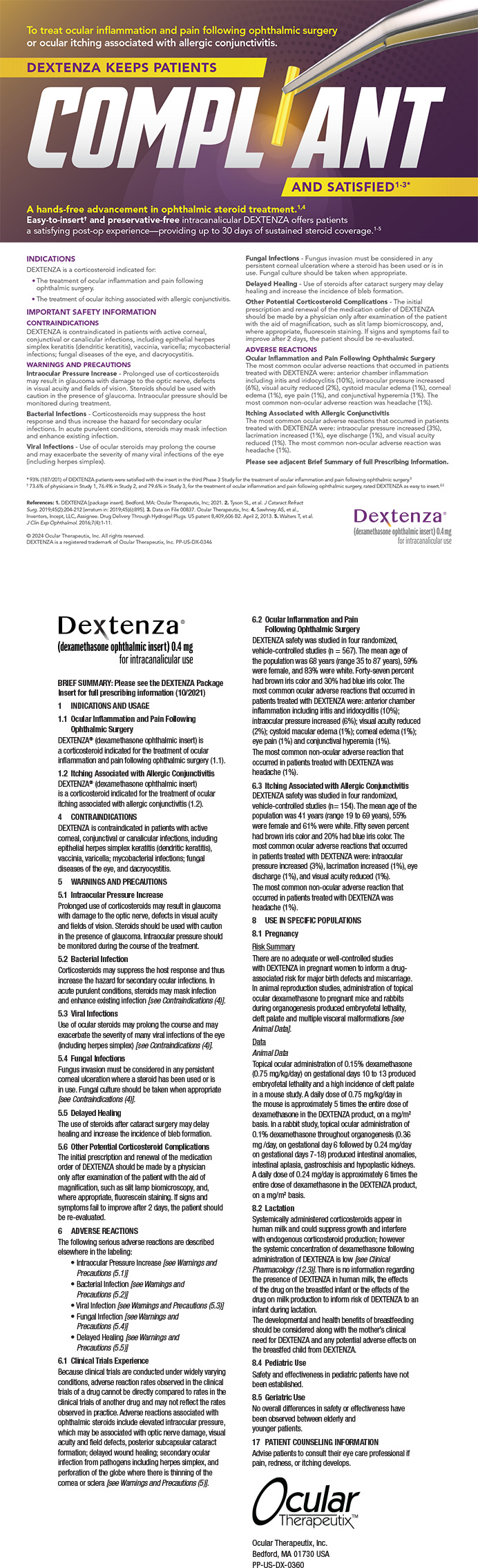
On examination, visual acuity is 20/20 OD and barely hand motion OS. A very mild afferent pupillary defect and an irregular pupil are evident in the left eye. Slit-lamp examination of the right eye is essentially normal. The left eye has normal lids and lashes. The conjunctiva and sclera have a small temporal scar that extends onto the cornea inferior to the visual axis. The anterior chamber is quiet. A large defect is evident in the temporal iris. A mature cataract is present, and the temporal capsular bag has an irregular contour. The loss of zonular support in the temporal meridian is severe
(Figure 1).
Figure 1. The preoperative appearance of the left eye. Note the irregular pupil, hypermature traumatic cataract, and loss of zonular support in the temporal zone. A temporal corneoscleral scar is also evident.
A retinal examination of the right eye is normal. There is no view of the retina in the left eye, but B-scan ultrasound is normal.
How would you approach this patient’s mature cataract given the duration and severity of the traumatic injury?
—Case prepared by Brandon D. Ayres, MD

MELISSA B. DALUVOY, MD
An injury sustained at such a young age increases the likelihood of amblyopia, but this patient reports that he had OK vision in his youth. Because he says he has had no useful vision for the past 30 to 40 years, the patient must be counseled that his visual prognosis is guarded, and he must be educated on the risks of surgery.
With regard to surgical approaches, there are a few options: traditional phaco cataract surgery with the placement of a capsular tension ring (CTR) and Ahmed Capsular Tension Segments (CTSs, Morcher) and IOL implantation; a posterior lensectomy, vitrectomy, and scleral fixation of an IOL; and manual small-incision cataract surgery and IOL implantation. My decision would depend on the density of the lens. If it is too dense to remove with phacoemulsification or a fragmatome, manual small-incision cataract surgery is the safest option. This patient is relatively young, however, and although the center of the cataract exhibits some brunescence, the cataract appears to be more cortical and can likely be removed with phacoemulsification.
A retrobulbar or peribulbar block would be my preference because cases such as this one can be unpredictable. I would take a superior approach so that I am not working over the area of zonular loss. The capsule would be stained, and a dispersive OVD would be instilled to cushion the area of zonular loss and keep the vitreous back. After the capsulorhexis, the cataract would be removed gently. I would be prepared to place capsular hooks at any time in response to capsular instability.
Assuming the cataract is removed safely and the capsular bag is intact, I would use a CTR and Ahmed CTS to fixate the capsular bag to the sclera. This can be done by placing a polypropylene suture (Prolene, Ethicon) or a PTFE suture (Gore-Tex, W.L. Gore & Associates) in a scleral pocket or groove. I would choose a three-piece IOL to implant. If the capsular bag has been violated or cannot be adequately stabilized, I would perform a thorough anterior vitrectomy and place a scleral-fixated IOL using the Yamane technique.

MICHAEL D. GREENWOOD, MD
If the patient had usable vision from age 2 to roughly age 18, then it was lost when the traumatic cataract became severe and can likely be restored. My approach to this case would begin with thorough informed consent that includes detailed discussion of the potential need for multiple surgeries and an explanation that the plan may change quickly once the eye has been entered.
After staining the capsule with trypan blue dye, I would perform my normal capsulorhexis. If zonular laxity is severe, it may be necessary to insert capsular hooks before completing the capsulorhexis. A laser capsulotomy would be an excellent alternative here.
If not required during the capsulorhexis, capsular hooks would be placed thereafter, and phacoemulsification would be performed, followed by careful irrigation and aspiration. A CTR and then a CTS would be placed in the area of zonular loss, and a one-piece acrylic IOL would be implanted. Next, an artificial iris (CustomFlex ArtificialIris, HumanOptics) would be implanted to reduce glare and improve cosmesis. Alternatively, if the defect is small enough not to require an iris implant, a pocket can be created with a femtosecond laser, and corneal tattooing can be performed.
In cases similar to this one, I like to have a full toolbox and multiple plans should I need to change direction in the moment.

SOOSAN JACOB, MS, FRCS, DNB
The ocular trauma probably rendered the eye amblyopic. Because the vision in this eye was usable when the patient was very young, reasons for the delayed posttraumatic loss of vision such as secondary glaucoma and vitreoretinal pathology must be considered. The recent reduction in vision in the left eye is likely secondary to the hypermature cataract. Cataract removal may restore vision to the prior low baseline. An additional consideration is that, without surgery, the hypermature cataract may leak or subluxate further and cause complications. Cataract surgery may therefore be attempted. The visual prognosis is poor, so informed consent is essential.
Axial length measurement should be performed using immersion ultrasound. Because of the corneal scar, topography would be useful to determine the presence of irregular astigmatism. The scar is quite peripheral, so it is likely that the central cornea is reasonably regular. Repeat keratometry (K) measurements using different machines would be helpful. An average K value may be taken, or the other eye’s K values may be used. A limited view of the optic disc and the macula may be possible through the aphakic temporal portion of the pupil. Given the mild afferent pupillary defect, the accuracy of the patient’s light projection should be ascertained. A visual evoked potential may also be useful to assess visual potential.
Because the dialysis seems to extend for almost 180º, conventional cataract surgery with only a CTR would be difficult. Two options can be employed. The first is scleral fixation of the bag with a device such as a Cionni CTR (Morcher) or Ahmed CTS. My preference, however, would be to use either a Jacob glued capsular hook technique (off-label use)1 or a Jacob paperclip capsule stabilizer (Morcher; www.youtube.com/watch?v=kD3zIa-SkVc) together with a CTR. The phacoemulsification of a hypermature, subluxated cataract will be difficult with any form of scleral fixation, capsular hooks, or a CTR because of the dense nucleus, the difficulty of chopping, the lack of a protective epinuclear cushion, a lax and flimsy capsular bag, and the probable weakness of the entire zonular apparatus. The risk of extending the zonulodialysis and the tear in the posterior capsule is high.
A second option is to remove the cataract in toto with its capsule, perform an anterior vitrectomy, and then secondarily fixate an IOL. In this scenario, the glued IOL technique would be my preference, especially because the large iris defect will make iris fixation more difficult. Whichever option is chosen, I would perform a pupilloplasty to repair the iris defect.
If the eye has high irregular astigmatism, a third option is to use pinhole optics, achieved with a pinhole IOL or a pinhole pupilloplasty.
Regardless of the approach, secondary pathology, if present, should be treated as well.

ZACHARY LANDIS, MD
At least 4 clock hours of zonular dialysis and iridodialysis are present. It is unknown if the anterior or posterior capsule has been violated. Preoperatively, I would have an extended discussion with the patient regarding his increased risk of nuclear loss and a ruptured posterior capsule and the uncertain visual prognosis given the injury that occurred in his youth.
Intraoperatively, I would look for vitreous prolapse with triamcinolone acetonide and perform an anterior vitrectomy if necessary. A dispersive OVD would be injected, and the anterior capsule would be painted conservatively with trypan blue dye to prevent the dye from traveling posteriorly. After careful completion of the capsulorhexis, four capsule retractors would be placed, and hydrodelineation would be performed.
Phacoemulsification using a stop-and-chop technique would be performed. After the removal of the nucleus and cortex, the capsule retractors would be withdrawn, and the stability of the capsular bag would be assessed. A CTR is inadequate to address the amount of zonular loss in this eye. A CTS would be placed temporally with a PTFE suture if the remaining zonular support is adequate. Ideally, a monofocal one-piece IOL would be implanted in the capsular bag if there is sufficient support with a CTS. If zonular weakness is diffuse, two CTSs may be placed. In this situation, however, I would opt to remove the capsular bag remnants, perform an additional anterior vitrectomy, and perform intrascleral haptic fixation of a three-piece IOL, either the CT Lucia 602 (Carl Zeiss Meditec) or the Tecnis (model ZA9003, Johnson & Johnson Vision).
The large iris defect is likely affecting the patient’s quality of vision, so a pupilloplasty using a modified Siepser knot would be performed at the conclusion of the case.

WHAT I DID: BRANDON D. AYRES, MD
After a discussion of the risks and benefits of cataract surgery and the unique challenges posed by the mature cataract, the lack of zonular support, the iris defect, and the probable amblyopia, the patient elected to undergo surgery. The surgical plan was to remove the cataract, potentially perform an anterior vitrectomy, and repair the iris if possible.
After standard cataract incisions were made, additional lidocaine followed by an OVD were instilled into the anterior chamber. The anterior capsule of the lens was then painted with trypan blue dye in an attempt to avoid staining the anterior vitreous. The capsulorhexis was carefully performed, and two capsular retractors were placed to act as temporary zonules. Once the lens was supported, hydrodissection was performed, and the nuclear portion of the lens was carefully removed. The cortical material was removed with bimanual irrigation and aspiration. After full inflation of the capsular bag with an OVD, a CTR was placed. At this point, it was deemed safe to place an IOL in the capsular bag.
The next step was to repair the temporal iris defect. The iris was carefully tested for elasticity with microforceps, and adhesions were lysed. Multiple 10-0 polypropylene interrupted sutures were placed in the temporal iris, allowing excellent reapproximation of the iris defect but causing a temporal decentration of the pupil. Microscissors were used to create small sphincterotomies in the nasal pupillary border, and intraocular diathermy was carefully performed to round out and nasally displace the pupil, achieving an acceptable surgical repair (Figure 2).
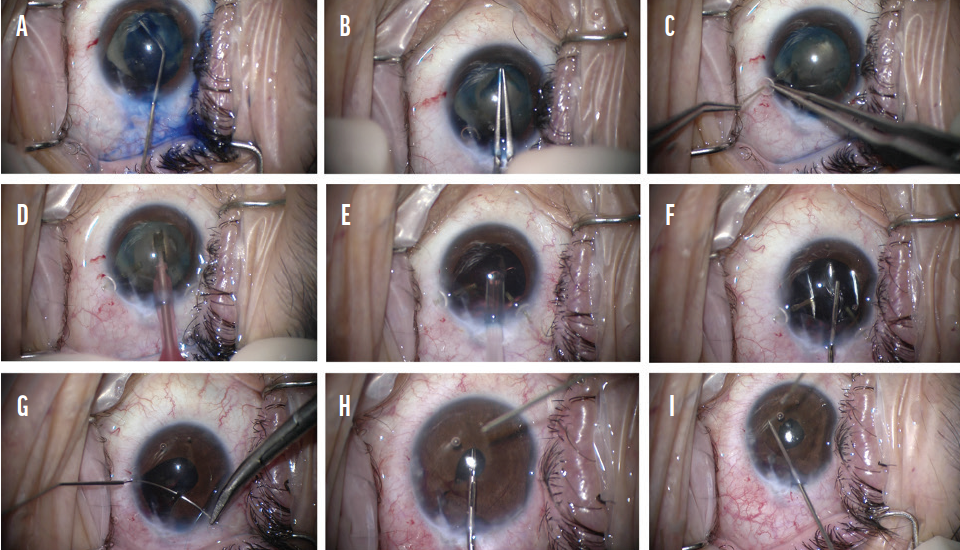
Figure 2. Trypan blue dye is used to stain the anterior capsule (A). A continuous curvilinear capsulorhexis is created (B). Capsular support hooks are placed to help support the capsular bag (C). Phacoemulsification is used to remove the lens (D). A CTR is used to increase support to the capsular bag (E), and a one-piece acrylic IOL is placed in the capsular bag (F). Interrupted polypropylene sutures are used to reapproximate the iris defect (G). Sphincterotomies are created using microscissors (H). Intraocular diathermy is performed to reshape the pupil (I).
One day after surgery, UCVA was 20/400 OS. A slit-lamp examination showed corneal stromal edema and endothelial folds. The anterior chamber was deep with a mixture of inflammatory cells and red blood cells, but no hyphema was noted. The iridoplasty sutures were intact, and the pupil was acceptably centered. IOP was 21 mm Hg, and a Seidel test of all wounds was negative. The patient was excited to notice an improvement in visual acuity, color, and visual field.
Topical steroids and antibiotics were continued for the first week after surgery. At the 1-week visit, the cornea was clear with only rare cell in the anterior chamber. UCVA was 20/80 OS. The patient was thrilled with the overall improvement in vision and the cosmetic result of surgery.
1. Jacob S, Agarwal A, Agarwal A, et al. Glued capsular hook: technique for fibrin glue-assisted sutureless transscleral fixation of the capsular bag in subluxated cataracts and intraocular lenses. J Cataract Refract Surg. 2014;40(12):1958-1965.