Customized therapeutic keratectomy (SCTK), an evolution of phototherapeutic keratectomy, can reduce or eliminate corneal higher-order aberrations (HOAs). We described the procedure in detail in a related article (click here to read the article). Residual lower-order aberrations can be subsequently corrected by cataract surgery and IOL implantation. Performing SCTK approximately 1 month before cataract surgery can improve the quality of vision and visual acuity in eyes with highly aberrated corneas, as demonstrated in the following case examples.
CASE EXAMPLES
Case No. 1. In January 2021, a 55-year-old man presented for a cataract evaluation in his right eye. The patient’s history was significant for myopic photorefractive correction in 2007.
On examination, myopic regression was evident; his BCVA was 20/32 with a refraction of -2.25 -1.45 x 45º. The patient reported seeing halos around lights at night and experiencing double vision. Tomography, topography, and wavefront aberrometry showed spherical aberration, which was responsible for the reduced contrast sensitivity and halos, and a mildly decentered optical zone, which was responsible for coma and double vision.
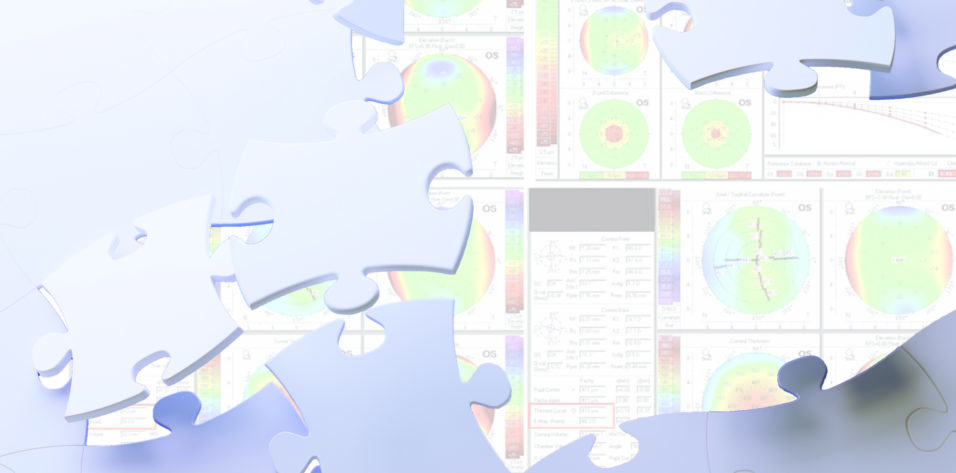
SCTK, phacoemulsification, and IOL implantation were planned. On the day of SCTK, tomography and topography were performed preoperatively (Figures 1 and 2). The patient underwent the corneal wavefront-guided customized transepithelial ablation planned by the surgeon (Figure 3) followed by wet—or smoothing—phototherapeutic keratectomy.
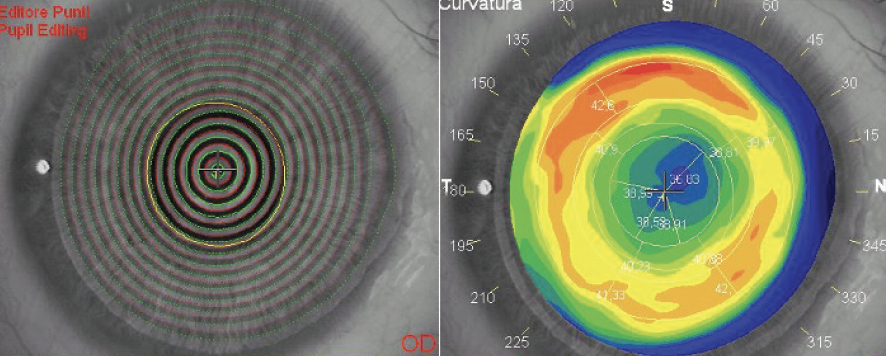
Figure 1. Keratoscopy was checked and edited (left). The tangential map on topography shows the red ring (corresponding to high dioptric values) that typically surrounds a central, slightly decentered, flattened area after myopic correction (right).
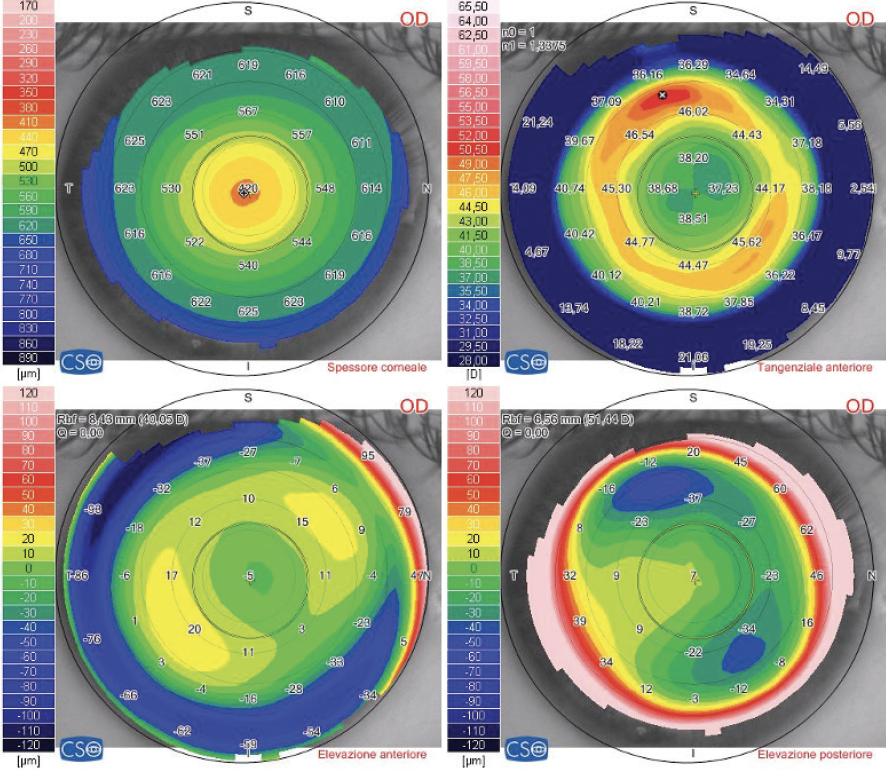
Figure 2. Tomographic maps obtained before SCTK: pachymetry (top left), tangential map (top right), anterior elevation map (bottom left), and posterior elevation map (bottom right).
Figure 3. The transepithelial ablation pattern customized by the surgeon and performed on the eye during SCTK. We described how the surgeon planned this specific ablation pattern in detail and with figures in a related article (scan the QR code on the previous page to read the article). This pattern ablates mainly in the midperiphery (the procedure removes tissue from areas not ablated during prior refractive surgery) and ablates almost nothing at the center of the cornea (where the prior refractive surgery ablated the most, leading to a thinner pachymetry).
After the first ablation step, the patient was asked to stand up and sit in front of the tomographer for new measurements (Figure 4). At this point, the surgeon was satisfied with the results of the first ablation step and halted the SCTK procedure.
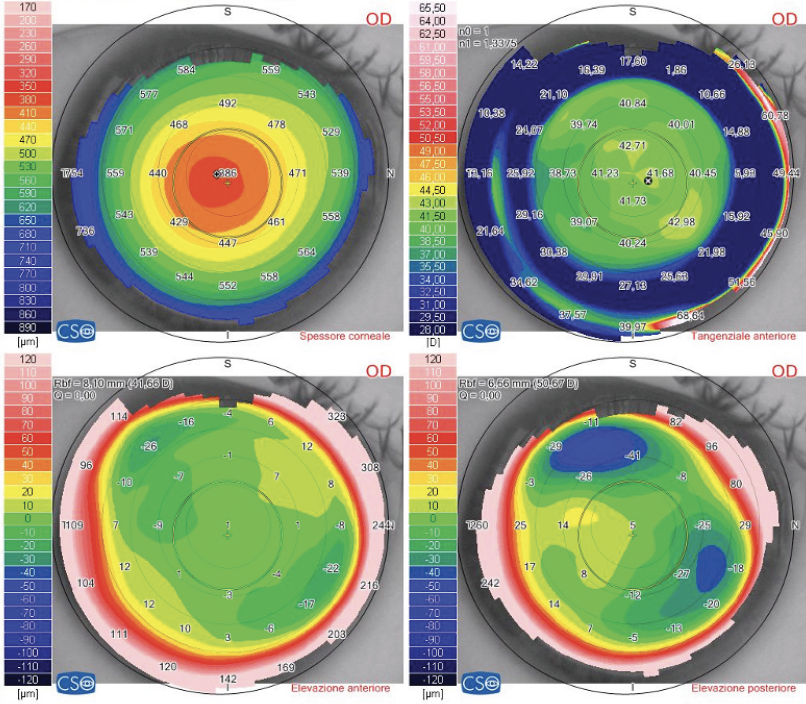
Figure 4. Tomographic maps acquired intraoperatively, after the first laser ablation step of SCTK: pachymetry (top left), tangential map (top right), anterior elevation map (bottom left), and posterior elevation map (bottom right). Epithelial regrowth after SCTK smooths the corneal surface further.
One month after SCTK, his BCVA was 20/25 with a refraction of -5.00 -0.75 x 50º. The patient underwent cataract surgery in February 2021, and his final BCVA was 20/20 with a refraction of -0.75 D of cylinder at 50º. The patient stated that his quality of vision had improved significantly after the SCTK procedure and that the halos and double vision had disappeared.
Case No. 2. A 52-year-old man was referred for an evaluation of his right eye. The patient had undergone PRK 4 years earlier to correct 3.75 D of hyperopia.
His corrected distance visual acuity (CDVA) was approximately 20/63 with a refraction of 1.00 D of sphere. A central corneal opacity and a cataract were visible on slit-lamp examination (Figure 5). Topography, tomography, aberrometry, and anterior segment OCT (Figure 5) were performed.
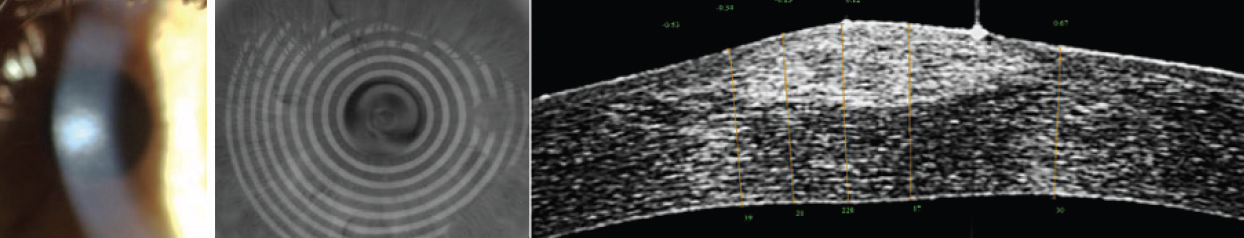
Figure 5. Before SCTK, a central corneal opacity is evident (left), and keratoscopy shows irregularity of the central mires (center). Anterior segment OCT shows an abnormal stromal scar after a hyperopic ablation, with increased corneal thickness and an abnormal corneal profile and appearance (right).
SCTK was planned to reduce HOAs. After SCTK, his CDVA was 20/32 with a refraction of 5.25 D of sphere. Optimal results were evident at the postoperative visit (Figure 6).
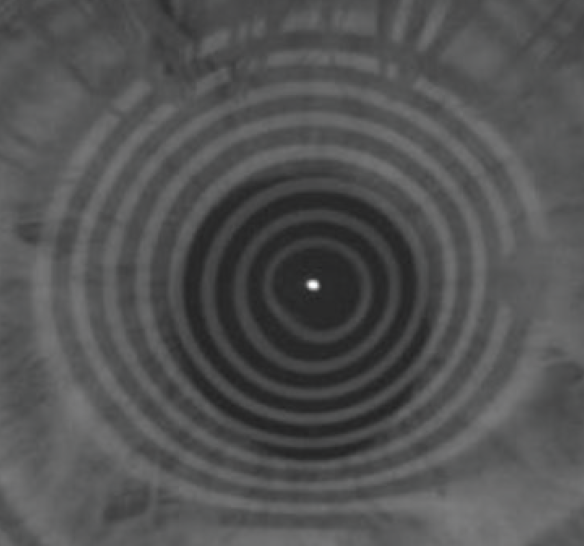
Figure 6. After SCTK, keratoscopy shows a dramatic improvement in terms of the regularity of the central mires.
Two months after SCTK, cataract surgery was performed, and a monofocal IOL was implanted with a desired final refractive target of -0.75 D of sphere to reduce the patient’s dependence on glasses. His final BCVA was 20/20 with a refraction -0.75 D of sphere, demonstrating achievement of the planned refractive target (Figure 7).
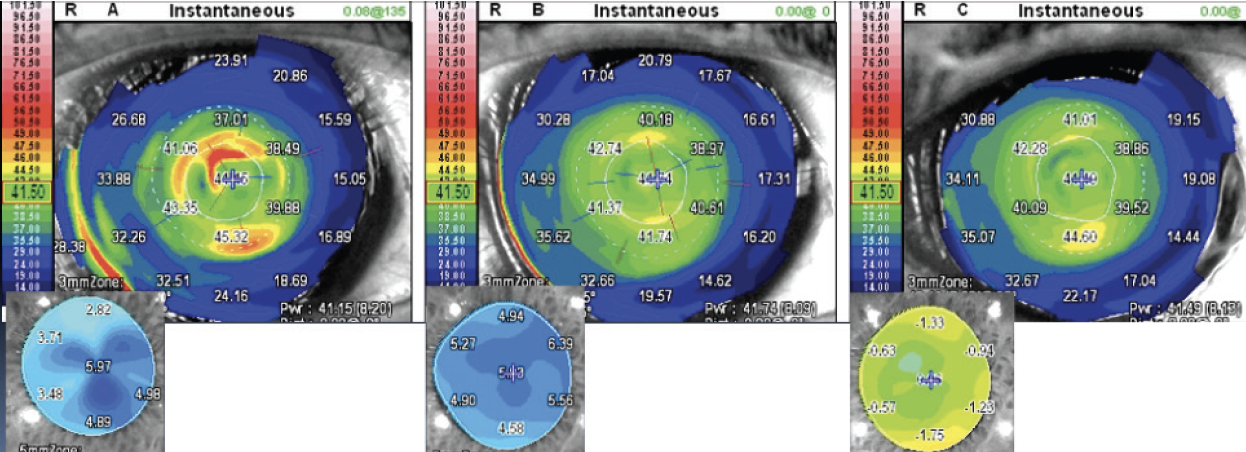
Figure 7. Tangential and OPD-Scan (Nidek) maps acquired immediately after SCTK (left), 2 months after SCTK and complete regrowth of the epithelial layer (center), and after cataract surgery (right).
Case No. 3. A man presented to our clinic in 2019 with a complaint of halos and decreased vision in his left eye. His history was significant for PRK in 1992 to correct -7.00 D of sphere in his left eye.
His BCVA was 20/40 with a refraction of -4.25 -0.50 x 160º. A cataract and annular corneal haze were visible on examination (Figure 8). SCTK was performed to eliminate HOAs. His postoperative CDVA was 20/32 with a refraction of -9.50 -0.50 x 160º.
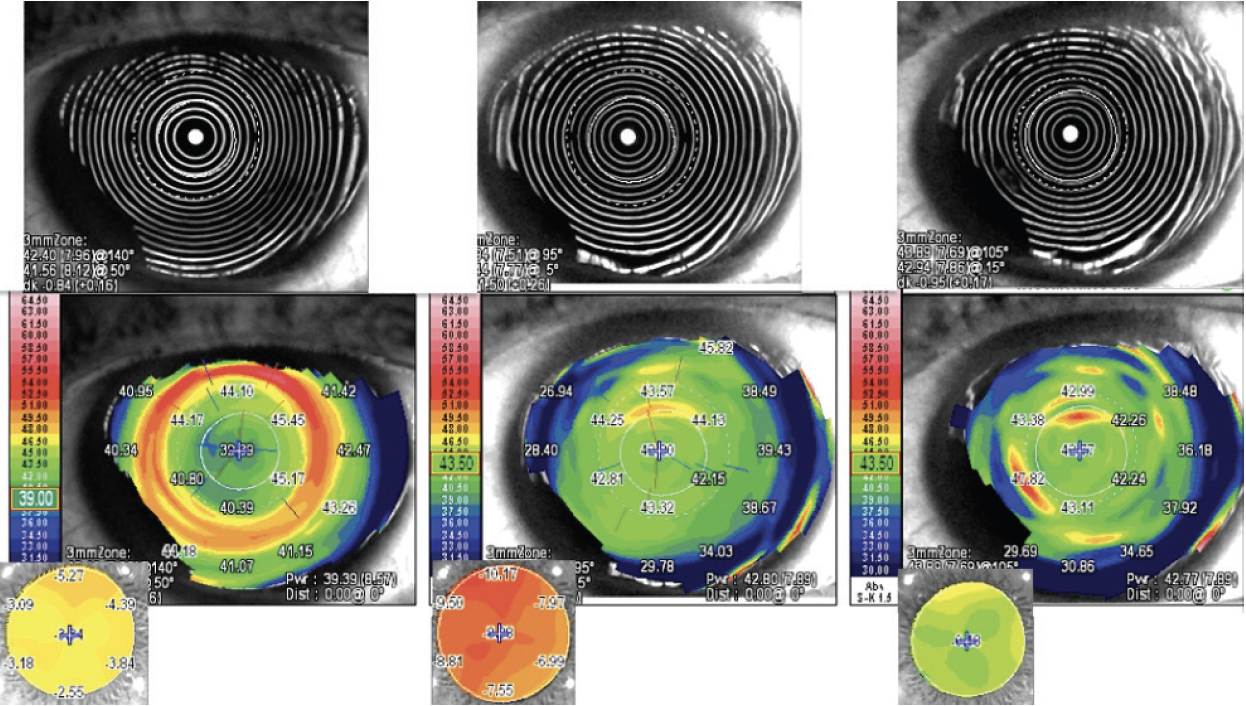
Figure 8. Keratoscopy, tangential, and OPD maps before SCTK (left), after SCTK (center), and after cataract surgery (right).
The refractive error increased after SCTK. The tangential map, however, showed the correction of the spherical aberration that was the main HOA component and that reduced contrast sensitivity. Moreover, a more prolate corneal shape was achieved (Figure 8).
A precise IOL power calculation also became possible. After cataract surgery, his CDVA was 20/20 with a refraction of -0.50 -0.50 x 20º, as planned. A mildly myopic target has demonstrated better intermediate visual acuity compared with emmetropia, with a minimal cost in terms of uncorrected distance visual acuity.1
In this case, SCTK eliminated the patient’s HOAs, which consisted mostly of spherical aberration. Cataract surgery and IOL implantation corrected the myopia induced by SCTK. In the end, quality of vision and visual acuity were optimal.
Case No. 4. A 64-year-old man who underwent bilateral LASIK in 2011 was referred by his ophthalmologist for a consultation. The patient reported experiencing postoperative diplopia and epithelial ingrowth in his right eye, which he stated was amblyopic. He also reported undergoing retreatments and relifting of the LASIK flap 11 times to peel the epithelial ingrowth.
On presentation, his BCVA was 20/100 with a refraction of +3.00 -4.00 x 60º. The patient underwent a complete ophthalmic examination that confirmed epithelial ingrowth in the LASIK flap (Figure 9). A cataract was also visible on examination.
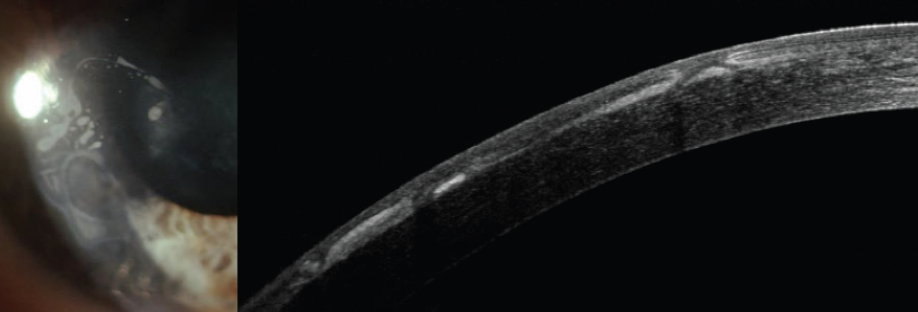
Figure 9. Photograph of the anterior segment (left) and anterior segment OCT (right) at presentation show epithelial ingrowth in the LASIK flap.
SCTK eliminated the HOAs, in this case composed mostly of coma (Figures 10–12). Postoperatively, the patient’s BCVA was 20/40 with a refraction of +2.00 -1.00 x 10º. After cataract surgery, his BCVA was 20/25 with the desired refractive target (-0.50 D of sphere) in his amblyopic eye.1
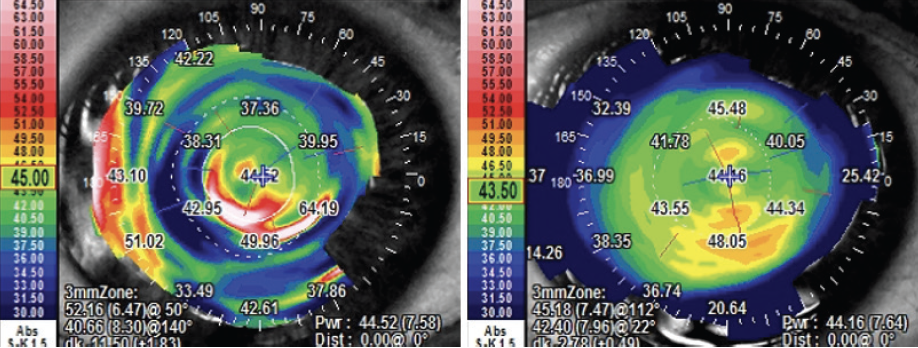
Figure 10. Preoperative (left) and postoperative (right) tangential maps.
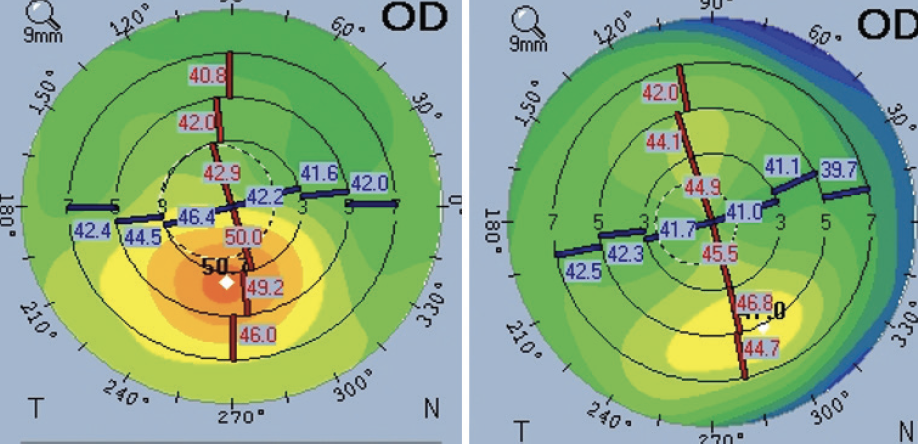
Figure 11. Preoperative (left) and postoperative (right) sagittal maps.
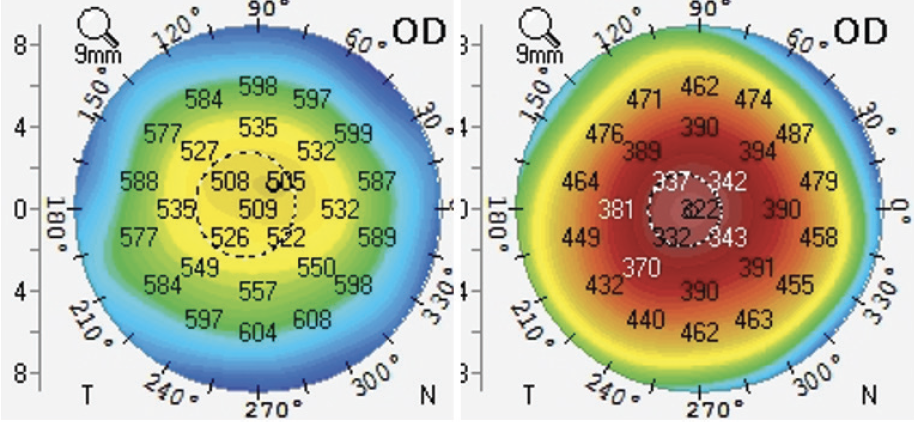
Figure 12. Preoperative (left) and postoperative (right) pachymetry.
This case highlights the importance of performing SCTK before cataract surgery to increase the precision of the IOL calculation. The biometric formula requires the input of the steepest and flattest meridians (K1 and K2) to predict the correct IOL power. The influence of K1 and K2 on IOL selection is greater even than axial length.
Looking at the preoperative tangential map, it is possible to understand how difficult—sometimes impossible—it can be to accurately determine K1 and K2 when the cornea is highly aberrated. If those measurements are unreliable, it may not be possible to correct residual refractive error after cataract surgery with an excimer laser procedure, and an IOL exchange or a piggyback IOL may be required.
Case No. 5. In July 2020, a woman presented with decreased vision in her left eye. The patient reported that she had undergone photorefractive treatment in 2002 to correct -8.00 D of myopia.
Myopic regression and a cataract were evident on examination. Topography revealed a slightly decentered treatment, which had induced HOAs—mainly coma and spherical aberration (Figure 13). Her BCVA was 20/32 with a refraction of -1.00 -0.75 x 150º. SCTK, phacoemulsification and IOL implantation were planned.
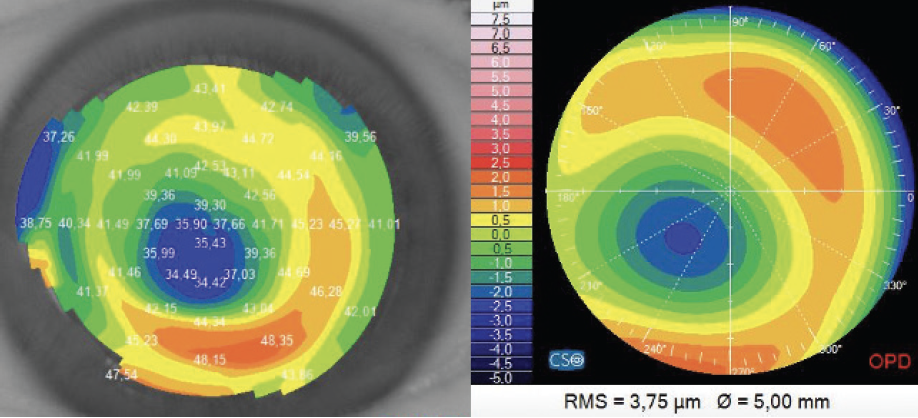
Figure 13. Topography (tangential map) shows a cornea that has undergone a decentered myopic photorefractive treatment (left). Measurements with the OPD-Scan shows corneal aberrations composed mainly of coma and spherical aberration (right).
SCTK was performed at the end of July 2020. Corneal HOAs were reduced with minimal stromal ablation (Figure 14). One month later, the patient’s BCVA was 20/25 with a refraction of -6.25 -0.75 x 155º (Figure 15).
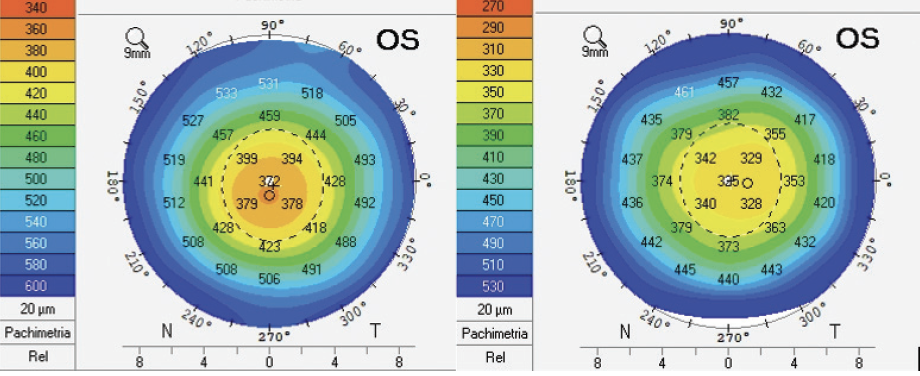
Figure 14. Pachymetry before (left) and 1 month after SCTK (right). Central stromal ablation was minimal.
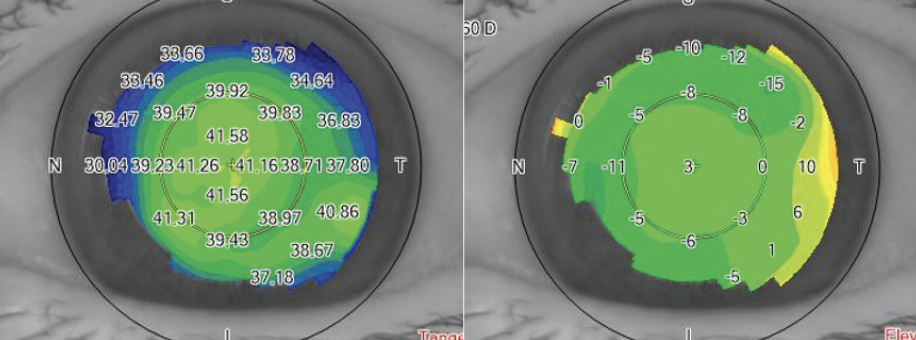
Figure 15. The topographic tangential power map (left) and the altitudinal map (right) were acquired 1 month after SCTK.
Cataract surgery was performed in September 2020. Her final BCVA was 20/20 with a refraction of -0.75 D of cylinder at 155º.
CONCLUSION
In eyes with highly aberrated corneas, performing SCTK before cataract surgery can dramatically improve the patient’s quality of vision and visual acuity after cataract surgery and IOL implantation.
1. Vinciguerra P, Holladay JT, Pagano L, et al. Comparison of visual performance and satisfaction with a bilateral emmetropic vs a bilateral mild myopic target using a spherical monofocal intraocular lens. J Cataract Refract Surg. 2020;46(6):839-843.