Thanks to continued advances in operating equipment, surgical technique, and IOL technology, cataract surgery is safer and more effective than ever. Although most patients will be relatively straightforward surgical candidates, those with preexisting retinal diseases such as age-related macular degeneration, retinal detachment, and diabetic macular edema may require certain modifications in surgical planning. This article reviews the factors to consider when managing these patients, with a special focus on posterior chamber IOL selection.
SET EXPECTATIONS
Because patient expectations for cataract and refractive surgery are extremely high, it is crucial for those with retinal conditions to understand that their surgical outcomes may not match the outcomes of others, including their family or friends who might have shared with them their positive experiences.
It is advisable to assess patients’ visual potential first, then image the retina with OCT to confirm that no recent changes have occurred. If you have doubts about current retinal status, refer patients back to their retina specialist. In our experience, it is especially helpful for patients to hear about their guarded visual potential twice—first from the retina specialist and again from the anterior segment specialist.
PREOPERATIVE PEARLS
Taking proper steps preoperatively can aid in IOL selection.
IOL power calculations. The same principles of IOL measurement used for routine cataract surgery patients apply to those with retinal conditions. Among them are the following:
- Assess the ocular surface for signs of dry eye disease and epithelial basement membrane dystrophy to ensure accurate calculations;
- Consider performing corneal topography, especially in patients with excellent visual potential who may benefit from a toric IOL;
- Use cataract grade to guide the type of biometry used (see IOL Power Calculation);
- Obtain calculations for a variety of IOLs in case of an unexpected event;
- Perform a preoperative evaluation for phacodonesis in every cataract surgery patient but especially in those with a history of pars plana vitrectomy (because they are more often affected by zonular dehiscence and posterior capsular compromise); and
- Be sure to note a history of refractive surgery so that appropriate IOL formulas are used. This detail can easily get buried in a complicated ocular history.
IOL POWER CALCULATION
Make the Most of Biometry
Optical biometry can be used in most patients; modern swept-source OCT biometers can penetrate even mature cataracts. However, after a pars plana vitrectomy with gas tamponade or lens touch, the cataract can be dense and white, and ultrasound biometry is often necessary. Obtaining an accurate axial length measurement is critical with ultrasound biometry. Asymmetry may be seen in patients with a scleral buckle. Regardless of the type of biometer used, scrutinize the metrics on measurement quality.
You may occasionally encounter a patient whose eye is filled with silicone oil, which will make performing IOL measurements more difficult. Silicone oil induces a hyperopic shift of 3.00 D or more,1,2 so remember to change the setting on the biometry machine to account for the presence of the oil. The choice of IOL power depends on the plan for the silicone oil. If it will be removed soon, select the IOL power as you normally would; if the oil will remain in place for the long term, various software programs such as the Holladay IOL Consultant (Holladay Consulting) can help you to determine the optimal IOL power.
1. Hotta K, Sugitani A. Refractive changes in silicone oil-filled pseudophakic eyes. Retina. 2005;25(2):167-170.
2. Grinbaum A, Treister G, Moisseiev J. Predicted and actual refraction after intraocular lens implantation in eyes with silicone oil. J Cataract Refract Surg. 1996;22(6):726-729.
Refractive target. The refractive target is a decision shared with the patient. For patients with macular degeneration, it may be advantageous to aim for distance vision so that the plus spectacles used for reading boost magnification. For patients who have high myopia, especially those who are young and may not have the contralateral cataract extracted for many years, it is important to consider the potential for significant postoperative anisometropia. Unless they are willing to wear a contact lens or to have the contralateral cataract removed soon, consider aiming for a myopic target that will balance with the visual acuity of the fellow eye.
IOL selection. Hydrophobic acrylic monofocal IOLs are generally the safest bet in retina patients. Toric IOLs are an excellent option for patients with regular astigmatism, and several companies manufacture them on hydrophobic acrylic platforms.
Certain IOLs should be avoided in this population. Patients with significant maculopathy may not tolerate presbyopia-correcting IOLs because of a possible degradation in contrast vision and a 12% to 18% loss of light from diffractive optics. This loss of light can negatively affect visual function, especially in low-luminance settings. Moreover, performing retinal surgery—particularly fine macular work—through presbyopia-correcting IOLs can be challenging. This is an important consideration because these patients may require future retinal surgery procedures.
Silicone IOLs should also be avoided because silicone oil adheres to and opacifies these lenses. Even if silicone oil is not presently in the eye, silicone oil tamponade may be required in the future.
Hydrophilic acrylic IOLs should be avoided for similar reasons: They are prone to calcification if gas tamponade is ever performed, although this phenomenon has also been reported in hydrophobic IOLs.1,2
As a retina surgeon, I (C.Y.W.) do not notice a significant difference between one- and three-piece IOLs in the capsule, but I prefer an optic diameter of at least 6 mm for visualization purposes. Of course, if an IOL is placed in the sulcus because of a ruptured posterior capsule, it must be a three-piece design to avoid sequelae such as uveitis-glaucoma-hyphema syndrome (Figure). If the posterior capsule is violated but the anterior capsulorhexis is intact, sulcus fixation of the IOL with optic capture is a good option. In this situation, an adjustment of IOL power is not necessary, whereas the power should be decreased if the entire IOL is placed in the sulcus; www.doctor-hill.com is a useful reference in this situation.
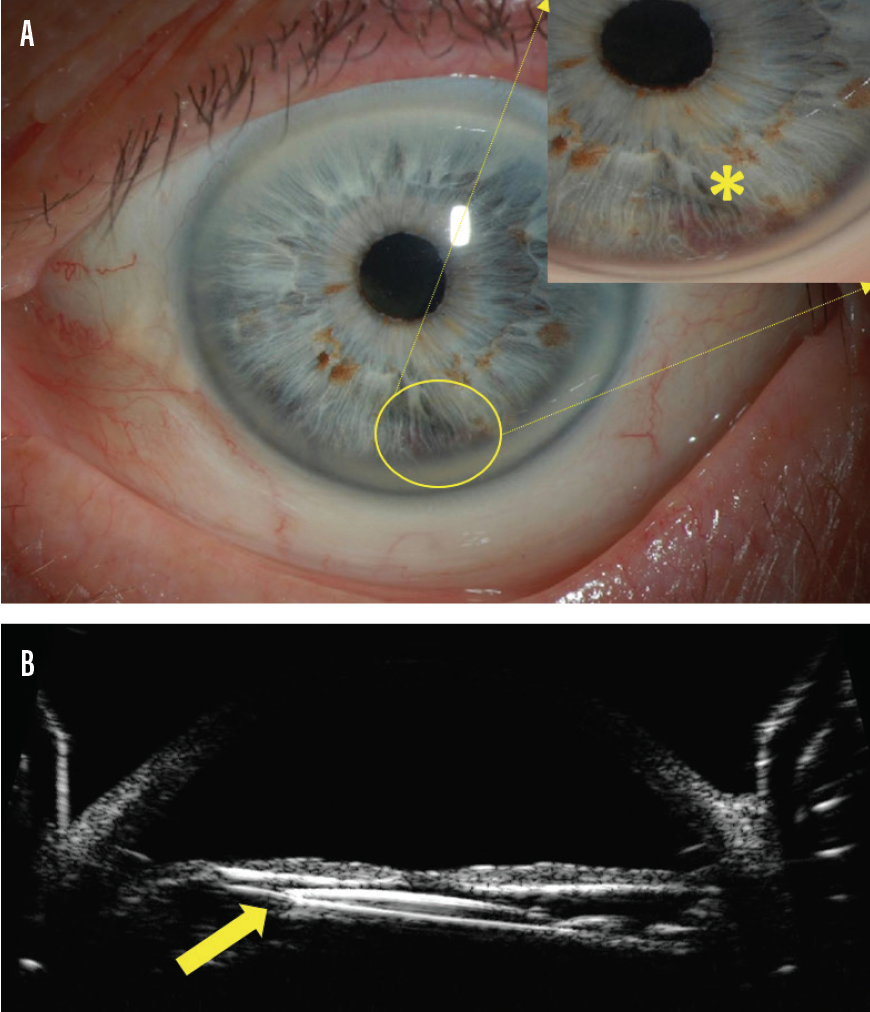
Figure. Uveitis-glaucoma-hyphema (asterisk indicates hyphema) syndrome (A) caused by a one-piece IOL that resides partially in the sulcus (arrow), as confirmed on ultrasound biomicroscopy (B).
When capsular support is inadequate, scleral-fixated IOLs are a popular alternative. The only IOL approved for scleral fixation is the CZ70BD (Alcon), but its placement necessitates a large incision because of the 7-mm optic and nonfoldable PMMA composition. If the Yamane technique is used, the CT Lucia 602 (Carl Zeiss Meditec) is a good choice because of its strong and flexible polyvinylidene fluoride haptics. Remember that leaving the patient aphakic and returning later for secondary IOL placement is always a valid option, especially when unexpected complications occur.
INTRAOPERATIVE, POSTOPERATIVE PEARLS
Likewise, taking proper steps intra- and postoperatively is helpful to ensure good postoperative results.
Intraoperative pearls. The pupils of patients with a history of retinal surgery may not dilate well, so an expansion device may be required. A small capsulorhexis can minimize anterior optic prolapse if gas placement becomes necessary in the future. When performing phacoemulsification, avoid excessive tension on the zonules, which may be weakened from previous pars plana vitrectomy or intravitreal injections. Have capsular tension rings and capsular tension segments on hand in case they are needed. Remove peripheral lens epithelial cells as thoroughly as possible to minimize subsequent secondary opacification.
Postoperative pearls. Ensuring that patients follow up with their retina specialist postoperatively is important for several reasons. First, these patients are prone to developing a posterior vitreous detachment after cataract surgery. Second, patients with certain pathologies such as lattice degeneration require close monitoring. Third, some patients may be due for their regular intravitreal injections, and others require a thorough retinal examination now that the posterior segment is visible again.
CONCLUSION
Cataract surgery dramatically improves visual function in many patients—even those with serious retinal conditions. With appropriate preoperative planning, careful surgical technique, and proper IOL selection, you can maximize outcomes for retina patients.
1. Khurana RN, Werner L. Calcification of a hydrophilic acrylic intraocular lens after pars plana vitrectomy. Retin Cases Brief Rep. 2018;12(3):204-206.
2. Werner L, Wallace JK, Balendiran V, Shumway C, Ellis N, Mamalis N. Surface deposits mimicking calcification on a hydrophobic acrylic intraocular lens. J Cataract Refract Surg. 2019;45(7):1036-1039.