Visually significant astigmatism greater than 0.50 D affects more than 70% of individuals.1 In young people, the resulting distortion and blurring of vision can be corrected with prescription glasses, contact lenses, or refractive surgery. However, many patients who have worn glasses or contacts for astigmatism all their lives are first presented with the tantalizing possibility of seeing well with their naked eyes when they develop cataracts. The ability to solve two problems at once—age-related cataracts and long-standing astigmatism—is often met with enthusiasm by these patients.
To ensure the best possible outcomes, it is important for eye surgeons to be armed with all the options at their disposal. One option that is gaining popularity over other astigmatism-correcting procedures is implantation of a toric IOL during cataract surgery. This lens-based surgical option is discussed in depth in this article, in the context of other pre-, intra-, and postoperative approaches to correcting astigmatic refractive error.
GETTING TO KNOW THE PATIENT
As with any cataract surgery, it is important to ascertain the visual needs and desires of astigmatic patients, to get to know their expectations, and to fully delve into their ocular past to explore the potential possibilities of his or her ocular future. Questions to explore include these:
- What is your occupation, and what are its visual demands?
- What are the three most important activities for you, both for work and hobbies?
- What roles do glasses play in your life?
- What is your past ocular and medical history? Have you had surgeries before?
- Are you comfortable investing in and do you recognize the value of visual freedom?
The role of glasses and the financial implications of surgical astigmatism correction must be clearly delineated to the astigmatic patient. The correction of astigmatism might take the form of a toric IOL or femtosecond arcuate incisions concurrent with cataract surgery; insurance typically does not cover either of these options.
Although cataract surgery is known to be one of the safest and most efficacious of surgeries, the physician must be cognizant of and empathetic to the patient’s concerns and fears: What are the complications? Will the surgery hurt? How difficult is recovery? The fears of some patients are so debilitating that they forgo the potential benefits of surgery and make do with their deteriorating functional vision. Depending on the status of the cornea and the extent and type of astigmatism, additional, albeit smaller, procedures may be required prior to, during, or after the cataract removal itself, making it even more important that the patient be fully informed and comfortable with these steps going forward.
DIAGNOSTICS
In evaluating and measuring the ocular and optical properties of the patient’s eyes to customize the surgical approach and choose a specific IOL, the tests that must be ordered and analyzed after baseline visual acuity and refraction are obtained include:
- For all patients: Anterior and posterior corneal topography, keratometry, tear evaluation (meibography and tear osmolarity) to assess for dry eye conditions that might affect surgical recovery and healing, macular OCT to assess for underlying retinal conditions that might limit potential visual acuity after surgery or require additional surgeries or procedures, and optical biometry for IOL power calculation;
- For patients with a history of glaucoma and glaucoma suspects: Possible visual field testing and retinal nerve fiber layer analysis; and
- For patients with corneal dystrophies: Specular microscopy and endothelial cell count.
To address astigmatism in particular, three data points must be plotted: level of astigmatism in diopters, type of astigmatism, and axis of astigmatism (see Three Data Points for Astigmatic Correction). These points can be collected with topographic evaluation of corneal keratometry. Updated toric IOL calculators and regression formulas can also aid in surgical planning and customization.
THREE DATA POINTS FOR ASTIGMATIC CORRECTION
Level of Astigmatism
Typically, >1.00 D of with-the-rule astigmatism and >0.70 D of against-the-rule astigmatism is considered:
- Visually significant;
- Not correctable with the main phaco incision; and, therefore,
- Warrants consideration of correction during cataract surgery.
Type of Astigmatism
Symmetric, asymmetric, irregular, or skewed
Axis of Astigmatism
With the rule: 60º–120°
Against the rule (more common in the elderly): 150°–210°
Oblique: 30°–60° or 120°–150°
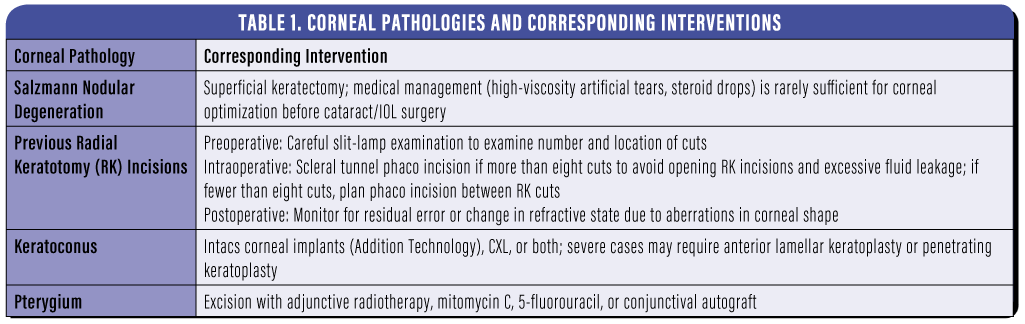
Irregular astigmatism may be caused by previous trauma or surgery, Salzmann nodules, pterygium, corneal scars, corneal melts, or other corneal diseases. These may represent contraindications to toric IOLs or limbal relaxing incisions (LRIs), or it may be possible to treat them first to normalize the corneal contour prior to astigmatic correction.
It is crucial to obtain accurate measurements of the presenting astigmatism, but in patients with chronic dry eye disease (DED), narrow palpebral fissures, or deep-set eyes these measurements can be challenging to obtain. And no treatment course, let alone a surgical procedure, should be based on inaccurate measurements. It is therefore important to treat existing ocular surface disease, such as DED, and to optimize the cornea prior to surgical evaluation.
The eye surgeon should carefully consider the location and size of the clear corneal incision in surgical planning for cataract surgery. In eyes with negligible astigmatism, a larger-than-normal incision in the steeper axis of curvature can be made to allow surgical access to the lens and at the same time flatten the corneal curvature.
Other options for astigmatism reduction should be carefully discussed with the patient and evaluated in the context of the patient’s unique visual situation. In addition to the use of toric IOLs, these may include PRK; LASIK; and astigmatic keratotomy (AK) including LRIs, manual midperipheral arcuate incisions, and femtosecond arcuate corneal incisions.
PREOPERATIVE APPROACHES
If a patient with cataract desires visual freedom and concurrently has Salzmann nodules, pterygium, a previous corneal transplant with high astigmatism, or keratoconus, these conditions should be treated prior to cataract surgery (Table 1).
For patients with high astigmatism due to a previous corneal transplant, the astigmatism can be debulked before cataract surgery. Any of the following techniques can be used preoperatively to normalize the corneal contour, debulk the astigmatism to less than 4.00 D, and enable a more predictable and successful choice of toric IOL if necessary:
- Removal of any tight sutures;
- Partial graft dehiscence in areas of steep curvature;
- Intragraft arcuate incisions at a 7-mm optical zone using manual AK blades at the slit lamp or femtosecond laser; and
- Placement of compression sutures on the flat axis using intraoperative keratoscopy.
INTRAOPERATIVE APPROACHES
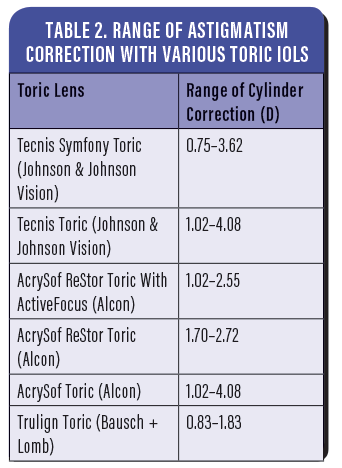
Toric IOLs. The first generation of toric IOLs became available in the United States in 1998, and they have since become a common way to address astigmatism intraoperatively. Intraoperative correction of astigmatism has been reported to improve overall lifetime savings and visual outcomes compared to postoperative vision correction with spectacles.2 Several toric IOL models are now available in the United States (Table 2).
The implantation of a toric IOL is trickier than standard IOL implantation. The axis must be aligned correctly with the plane of astigmatism, and the IOL must be carefully monitored for rotation away from the desired axis, especially in eyes with large capsular bags. If the capsular bag diameter is greater than 25 mm, placement of a capsular tension ring is useful to minimize toric IOL rotation. Other complications can include the need for a second procedure to realign the IOL to the correct axis or lens exchange if the lens has rotated and capsular fixation has already occurred.
Advantages of toric IOLs over LRIs, AK, and photorefractive corneal surgery include the avoidance of incisional complications and the standardization of astigmatism correction.
LRIs and AK. Performed immediately prior to cataract surgery, LRIs can be used to effectively treat 1.00 to 3.00 D of astigmatism. The incisions are made at the limbus circumferentially across the steep axis. The limbal location preserves the cornea’s optical quality; leads to faster recovery of functional vision compared with corneal incisions; and causes fewer incisional complications such as pain, discomfort, and residual refractive error.
AK can be done either manually or with a femtosecond laser; typically, femtosecond laser is reserved for skewed or asymmetric astigmatism or for treatment of astigmatism with use of a multifocal IOL that does not correct astigmatism.
Choosing the best approach. In post-LASIK eyes, it is important to assess central corneal astigmatism based on the total corneal power map from the topographer and to treat with either a toric IOL or with AK to a 400-µm depth at a 7-mm optical zone (ie, within the flap). LRIs are less likely to be effective than AK, as they are made outside the flap.
In post-RK eyes, the »Trulign Toric IOL (Bausch + Lomb) offers a nice approach, correcting astigmatism and offering assistance with presbyopia. Monofocal toric IOLs do not address presbyopia, and the optics of diffractive multifocal toric IOLs might conflict with the RK incisions.
Some studies indicate that final visual outcomes with LRIs and toric IOL implantation are comparable.1,2 However, especially in myopic astigmatism, toric IOL implantation is reported to be more predictable and reliable in reducing the astigmatism; toric IOLs resulted in greater change in cylindrical error than LRIs alone or combined with a toric IOL. Variability in LRI outcomes can be due to technique and other subjective factors: the quality of the blade, the surgeon’s skill, the calibration and positioning of the blade, limbal versus far peripheral placement of incisions, and correct identification of the steep corneal meridian on keratometry.3,4
The surgeon can also utilize the first step of cataract surgery, the clear corneal incision, as an unofficial LRI, so to speak. Making a slightly larger incision across the steepest corneal meridian according to the topography map adds a bit of astigmatic correction.
POSTOPERATIVE APPROACHES
Residual astigmatism after cataract surgery is most likely to occur in eyes that are extremely hyperopic or extremely myopic. This can occur due to changes in effective power of the toric IOL in a long or short eye. Modern toric IOL power calculators such as the Barrett calculator take this into account.
Capsular fibrosis or small amounts of retained OVD can cause toric IOL rotation. It is important to ensure that the toric IOL has not rotated out of correct orientation. Variable healing of corneal incisions can also lead to residual astigmatism.
LASIK, PRK, and postoperative LRIs at the slit lamp can be performed to address residual astigmatism. Laser vision correction delivers more predictable outcomes, but LRIs are also becoming more precise with refined corneal measurement technologies and by limiting the variables in play; depth and location of the incisions are based on patient demographics and specific ocular properties such as IOP, corneal thickness, and corneal rigidity. If PRK is done in a patient older than 65 years, care must be taken to ensure good corneal healing: Glycemic control, vitamin C supplementation, and avoidance of sunlight without sunglasses for 3 to 4 months postoperative are important factors.
Lens exchange or lens replacement surgery is a last resort if residual refraction is too great to be countered by these other methods.
LENS-BASED OR CORNEA-BASED?
Lens-based surgical correction of refractive error, including astigmatism, has been gaining popularity over other keratorefractive procedures, especially with the revolution of IOL technologies and the rapid expansion of lenses on the market. Lens surgery can correct a broader range of refractive errors with greater accuracy and predictability in final functional vision than corneal refractive surgery. It can provide more reliable reduction in ametropia without the high rates of spherical aberration induced by corneal reshaping procedures. Keratorefractive procedures are limited anatomically by the amount of cornea that can be reshaped or ablated and functionally by the size of the pupil and of the treatment zone. All of these factors make lens-based correction a more efficacious choice, especially in eyes on the severe ends of the refractive spectrum, with high degrees of myopia or hyperopia.
Astigmatism is a fairly common condition that can be treated concomitantly with cataract. Young patients may prefer noninvasive methods to treat their astigmatism. In older patients with cataract, astigmatism can be managed surgically at the time of cataract surgery, combining the processes of evaluation and treatment for both conditions.
Cataract surgery is refractive surgery. There are myriad lens options at the surgeon’s disposal, depending on the circumstances and goals of the patient. Lens-based correction of astigmatism with a toric IOL is an increasingly popular choice for management by surgeons and patients alike, due to the efficacy of the approach, the ability to manage astigmatism along with cataract extraction, the relatively low complication rate, greater accuracy and postoperative predictability, permanent refractive stability, and a larger range of functional and anatomic visual correction compared with keratorefractive procedures.
1. Satterfield DS. Prevalence and variation of astigmatism in a military population.
J Am Optom Assoc. 1989;60(1):14-18.
2. Anderson DF, Dhariwal M, Bouchet C, Keith MS. Global prevalence and economic and humanistic burden of astigmatism in cataract patients: a systematic literature review. Clin Ophthalmol. 2018;12:439-452.
3. Lee J, Lee H, Kang DS, Choi JY, Kim EK, Kim TI. Comparison of toric foldable iris-fixated phakic intraocular lens implantation and limbal relaxing incisions for moderate-to-high myopic astigmatism. Yonsei Med J. 2016;57(6):1475-1481.
4. Ouchi M. High-cylinder toric intraocular lens implantation versus combined surgery of low-cylinder intraocular lens implantation and limbal relaxing incision for high-astigmatism eyes. Clin Ophthalmol. 2014;8:661-667.






