Performing cataract surgery in an eye with a small pupil can be technically challenging. A reduction in pupil diameter exponentially decreases the surgeon’s ability to see and perform surgery without risk of complications. A pupil diameter less than 6.0 mm is associated with increased risk of complications (eg, posterior capsular tears, retained lens fragments, and vitreous loss, along with difficulty in toric IOL alignment).1 If an 8.0-mm pupil comes down to 5.5 mm, it reduces the operative field by over 50%, and if a 6.0-mm pupil comes down to 3.5 mm, it reduces the operative field by 66%. Both scenarios increase complication rates. The risk of intraocular miosis increases with ocular comorbidities and other characteristics, including intraoperative floppy iris syndrome or history of alpha-blocker use, pseudoexfoliation, diabetes mellitus, history of uveitis, longer duration of surgery, history of trauma, and use of femtosecond laser during surgery.1 Surgery also releases prostaglandins, which stimulate the iris sphincter muscle and cause miosis. Ophthalmic viscosurgical devices (OVDs) have a transient effect. Use of compounded products and use of other drugs pose risks and availability can be limited and unpredictable. Pupil expansion devices are very useful in these cases.
Not all pupil expansion devices are created equal. In my view, a pupil expansion device should allow the surgeon to perform surgery as though there is no device in place—that is, without compromising technique or requiring the use of specialized instruments or maneuvers. It should be fairly simple to learn how to use, while also extremely stable to support the iris without causing iris sphincter damage. Overall, the use of a pupil expansion device should help the surgeon achieve the same thing every cataract patient wants: a safe, complication-free surgery and an accurate refractive outcome.
Using the APX 200
The APX 200 (FCI Ophthalmics; Figure 1) is a straightforward pupil expansion device that fits nicely into my surgical routine—precisely because I do not have to alter my technique in any way to use it. It provides ample visualization and, if the surgeon desires, its placement can be adjusted to provide extra space for instruments. In my experience, there is a minimal learning curve, and, perhaps most importantly to me, there is minimal risk of damaging the iris or inducing astigmatism.
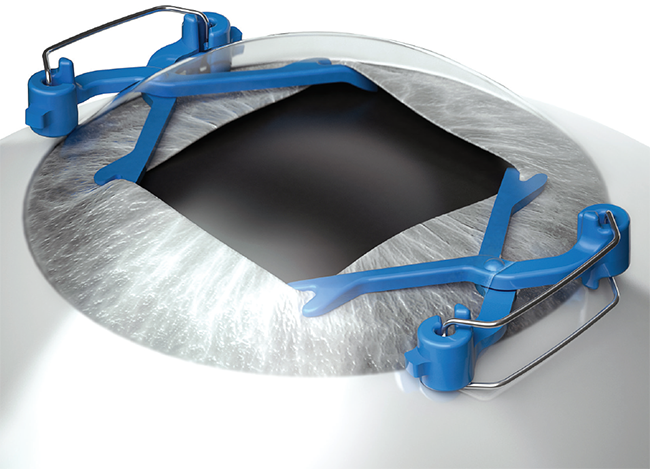
Figure 1. The APX 200 pupil expansion device.
The design of the APX 200 is intuitive (Figure 2). The device is supplied in a disposable blister pack with two expanders, each shaped like a pair of scissors, and two disposable forceps. To prepare the device for use, the forceps are used to grasp the outer segment of the APX 200, which are pinched to close the distal end, and then locked in place until they are used. One of the nice features of the APX 200 is the design of the tip at the distal end: a set of hooks gently engages the wall of the iris, and a slight forward bias in the tip means that the surgeon never has to bend the device forward (Figure 3). This latter feature makes all the more sense in regard to how the device is introduced to the eye.
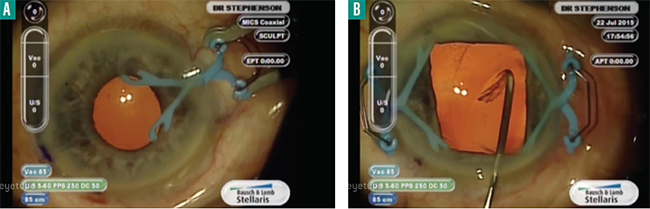
Figure 2. The APX 200 is a scissor-like device with a spring action that helps mechanically dilate the pupil (A). When properly inserted in the eye, the APX 200 provides ample working space and visualization of the surgical field (B).

Figure 3. The tip of the APX 200 is bent slightly downward allowing the shaft to remain parallel to the iris plane.
The APX 200 is introduced through 19-gauge sideport stab incisions that are exactly opposite to each other and that are parallel to the iris plane—I use either a 0.8-mm slit knife or an MVR blade for this step. I have found the incisions to be self-sealing and astigmatically neutral. In fact, because the incision is astigmatically neutral, I can use the APX 200 with ORA System with VerifEYE+ Technology (Alcon), which has advantages. For example, alignment of the IOL is often complicated in the eye with a small pupil; using ORA helps eliminate that concern.
The fact that I am able to use ORA demonstrates some nice features of the APX 200: it requires no special instruments to use, and it does not restrict the use of any tool the surgeon prefers. In my practice, I prefer to perform cataract surgery while sitting at the head of the patient, and thus, I place the APX 200 incisions at 9:00 and 3:00 o’clock. (Surgeons who perform cataract surgery temporally can use the device with incisions at 12:00 and 6:00 o’clock.) In past attempts to use a Malyugin ring while sitting at the head of the patient, I have found it necessary to create a larger superior wound to introduce the device, which may induce astigmatism. Even when using a Malyugin ring through a temporal incision, there is potential to ding the iris or expand the primary incision. With the APX 200, on the other hand, there is no need to adjust my preferred technique, and there is no risk of damaging the iris or wound architecture.
Tips for Success With the APX 200
As with any device used during surgery, there are some crucial steps to ensure success. I would suggest that any surgeon considering adding the APX 200 to his or her armamentarium to practice with the forceps outside the eye to get a feel for the spring action and how to release it slowly and gently.
After creating the two stab sideport incisions, the eye should be filled with a cohesive OVD to fill the chamber and raise the pupil before the APX 200 is introduced. The device should be removed before removing the OVD—although the device is used away from the endothelium, there is a risk of it falling posteriorly and damaging the capsule. To remove the device, the insertion procedure is done in reverse: the forceps grasp the outer edge of the device to close the scissor-like action and it is simply reversed along the same plane so as not to violate the capsule or scratch the implant.
I have found that the rectangular opening created when using the APX 200 is more than sufficient to view the surgical field. However, it may be possible to offset the placement of the devices to create a trapezoidal opening with a wider base facing the surgeon. Ehud I. Assia, MD, described this technique in an Eyetube video (eyetu.be/odigu); according to Dr. Assia, the trapezoidal opening allows even more space for use of surgical instruments.
Conclusion
In my hands, the APX 200 is an easy-to-use device with a minimal learning curve. It is astigmatically neutral and does not affect iris architecture. It is used with two incisions, whereas iris hooks require four incisions. A Malyugin ring can be used through the primary incision, but I find it hard to introduce via a superior wound—and this highlights perhaps the best feature of the APX 200: the surgeon does not have to adjust his or her technique to use the device.
1. Greenberg PB, Tseng VL, Wu WC, et al. Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology. 2011;118:507–514.




