
Laser treatments for glaucoma provide nonincisional options for reducing IOP. These procedures target either aqueous outflow via treatment of the trabecular meshwork or aqueous inflow via treatment of the ciliary processes. Laser trabeculoplasty (LTP), involving the application of laser energy to the trabecular meshwork, provides an alternative to medication for treating open-angle glaucoma. In contrast, transscleral cyclophotocoagulation (TSCPC), involving ablation of the ciliary processes, has traditionally been reserved for eyes with advanced glaucoma or refractory cases typically having failed medical and surgical management.
AT A GLANCE
- Laser treatments for glaucoma provide nonincisional options for reducing IOP.
- These procedures target either aqueous outflow via treatment of the trabecular meshwork or aqueous inflow via treatment of the ciliary processes.
- Recently, a new laser modality became available that offers unique versions of both laser trabeculoplasty and cyclophotocoagulation. Because of the pulsed laser delivery, treatment is considered to be less inflammatory than traditional continuous-wave laser therapy and to have a more favorable safety profile.
Recently, a new laser modality became available that offers unique versions of both LTP and cyclophotocoagulation. MicroPulse technology (Iridex) delivers pulsed energy over a designated duty cycle, allowing both “on” time for treatment as well as “off” time for tissue cooling. Because the laser is not designed to ablate or cause any thermal change to tissue, treatment is considered to be gentler than traditional laser therapies. Micropulse cyclophotocoagulation (MP-CPC) and micropulse laser trabeculoplasty (MLT) have still been shown to be effective in achieving IOP reduction, with less inflammation and a superior safety profile compared to its traditional counterparts.1-4

Figure 1. The 532-nm micropulse laser console.
SELECTIVE LASER TRABECULOPLASTY
Latina and colleagues first described Q-switched 532-nm Nd:YAG LTP or selective laser trabeculoplasty (SLT) in 1998.5 Using a goniolens, the surgeon visualizes the pigmented trabecular meshwork and applies laser energy to this tissue. SLT is thought to lower IOP by increasing outflow through the trabecular meshwork.6 Up to 360º of trabecular meshwork can be treated with the following settings: 0.6- to 1-mJ power, 400-mm spot size, and 3-nanosecond duration. Power is titrated until bubble formation in observed.
SLT has been shown to be as effective as one IOP-lowering medication, and it can be used as an initial treatment for open-angle glaucoma or ocular hypertension.7 The procedure’s success when repeated has also been demonstrated.8-10 Complications include infrequent IOP elevation and iritis and, rarely, corneal edema.
Micropulse Laser Trabeculoplasty
MLT targets the trabecular meshwork in a fashion similar to SLT. Laser energy is delivered in a pulsed fashion, however, and is therefore not considered to cause any tissue damage. Treatment is applied confluently across 360º of trabecular meshwork for a target of 120 spots with the following laser parameters: 1,000-mW power, 300-mm spot size, 300-nanosecond duration, and a 15% duty cycle.1 Because of the micropulse modality, no tissue reaction is seen during treatment, which can make the confirmation of proper treatment challenging initially. Like SLT, MLT is also repeatable. The procedure has been performed with 532- and 577-nm laser wavelengths.
In one study using the 577-nm laser, 360º MLT achieved an average IOP reduction of 19.5% in over 70% of cases, with a safety profile comparable to that of SLT.1 Another prospective study comparing MLT to SLT found an equivalent IOP reduction between groups, with greater comfort reported for patients in the MLT group.2
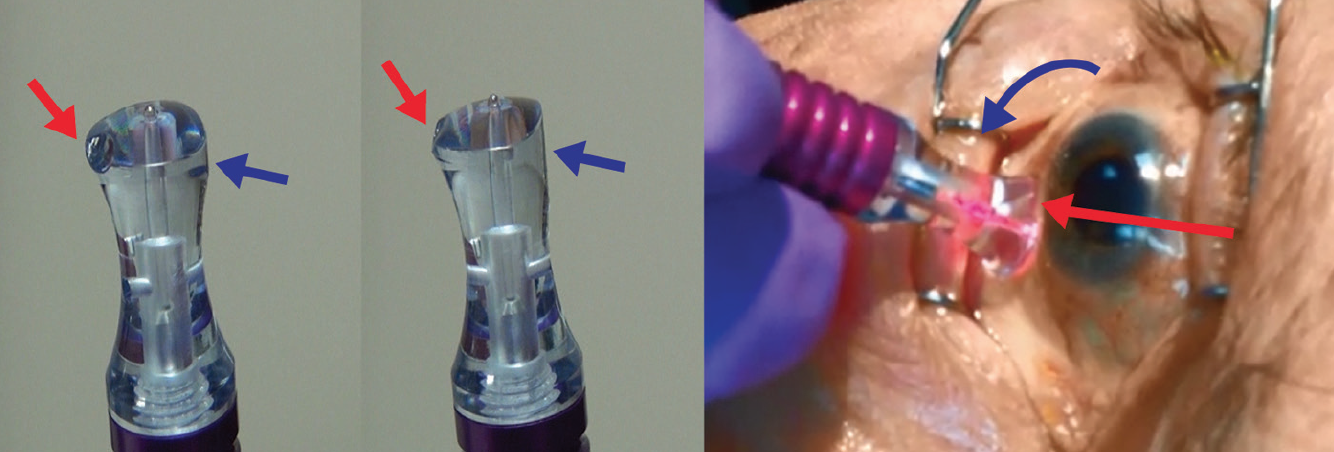
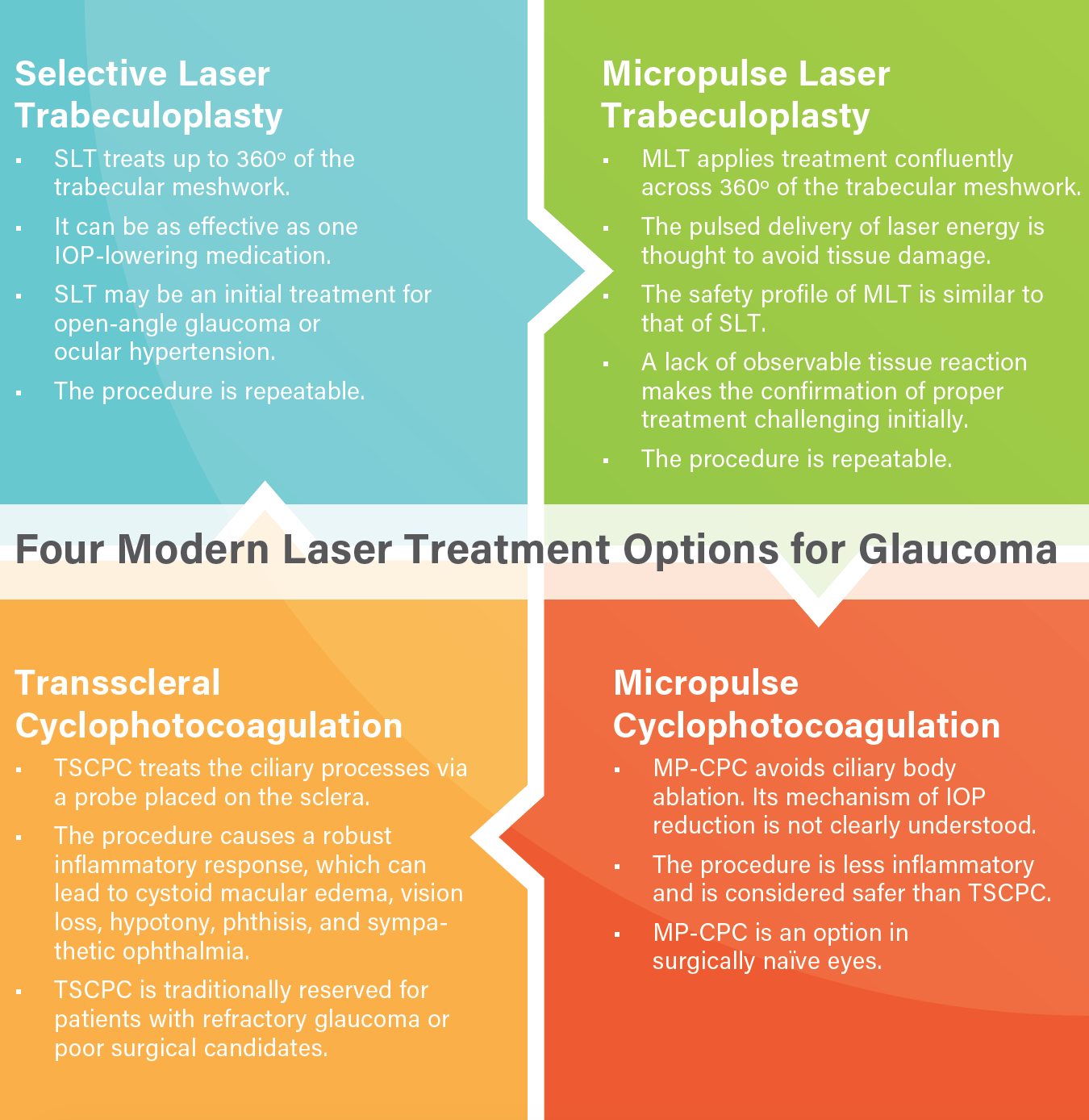
Figure 2. The MicroPulse P3 Glaucoma Device on the Cyclo G6 Glaucoma Laser System. Arrows indicate proper positioning: flat side toward the eyelid and notched side toward limbus.
Transscleral Cyclophotocoagulation
TSCPC involves the indirect application of an 810-nm diode laser to the ciliary processes via a probe placed on the sclera. The procedure often causes a robust inflammatory response, which can lead to cystoid macular edema, vision loss, hypotony, and—rarely—phthisis and sympathetic ophthalmia. For this reason, physicians traditionally reserve TSCPC for patients with refractory glaucoma or poor surgical candidates.
The Cyclo G6 Glaucoma Laser System (Iridex) is designed to deliver micropulse treatment to the ciliary processes. With a traditional transscleral laser, the surgeon performs discrete applications of laser energy via the G6 probe. MP-CPC, in contrast, is applied via slow sweeps along the limbus with the MicroPulse P3 Glaucoma Device (Iridex). The standard parameters are sweeps over each hemisphere for a range of 100 to 240 seconds at a power of 2,000 mW with 31.3% duty cycle.
The mechanism of IOP reduction via the Cyclo G6 is not clearly understood, because micropulse delivery avoids ciliary body ablation, but MP-CPC is thought to stimulate aqueous outflow.11 Because of the micropulse laser format, treatment is less inflammatory than traditional TSCPC and is considered to have a more favorable safety profile. MP-CPC is therefore considered to be an option for IOP reduction in surgically naïve eyes.
Kuchar and colleagues found MP-CPC to lower IOP by 20% to 30% in more than 70% of treated eyes, and they reported a better safety profile compared to traditional TSCPC.3 In a randomized study comparing MP-CPC and TSCPC, Aquino et al found the procedures to be equally effective at lowering IOP, but they reported a higher success rate and lower incidence of complications with MP-CPC.4 A histologic analysis of cadaveric eyes treated with TSCPC and MP-CPC revealed less ciliary body tissue disruption with the latter procedure.12
CONCLUSION
Laser treatments are valuable nonincisional options for glaucoma management. Micropulse technology offers a novel means of laser delivery that has been shown to be safe and effective.
1. Lee JW, Yau GS, Yick DW, Yuen CY. Micropulse laser trabeculoplasty for the treatment of open-angle glaucoma. Medicine (Baltimore). 2015;94(49):e2075.
2. Chadha N, Belyea D, Lamba T, et al. A randomized, prospective comparison of 360 degree selective laser trabeculoplasty (SLT) vs. 577 nm micropulse laser trabeculoplasty (MLT) in eyes with open-angle glaucoma. Poster presented at: American Glaucoma Society Annual Meeting; February 26-March 1, 2015; Coronado, CA.
3. Kuchar S, Moster M, Reamer CB, Waisbourd M. Treatment outcomes of micropulse transscleral cyclophotcoagulation in advanced glaucoma. Lasers Med Sci. 2016;31(2):393-396.
4. Aquino MC, Barton K, Tan AM, et al. Micropulse versus continuous wave transscleral diode cyclophotocoagulation in refractory glaucoma: a randomized exploratory study. Clin Exp Ophthamol. 2015;43(1):40-46.
5. Latina MA, Sibayan SA, Shin DH, et al. Q-switched 532-nm Nd-YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter, pilot, clinical study. Ophthalmology. 1998;105(11):2082-2088.
6. Gulati V, Fan S, Gardner BJ, et al. Mechanism of action of selective laser trabeculoplasty and predictors of response. Invest Ophthalmol Vis Sci. 2017;58(3):1462-1468.
7. Katz LJ, Steinmann WC, Kabir A, et al; SLT/Med Study Group. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012;21(7):460-468.
8. Francis BA, Loewen N, Hong B, et al. Repeatability of selective laser trabeculoplasty for open-angle glaucoma. BMC Ophthalmol. 2016;16:128.
9. Johnstone M, Wang R, Padilla S, et al. Transscleral laser induces aqueous outflow pathway motion and reorganization. Poster presented at: American Glaucoma Society Annual Meeting; March 2-5, 2017; Coronado, CA.
10. Polat J, Grantham L, Mitchell K, Realini T. Repeatability of selective laser trabeculoplasty. Br J Ophthalmol. 2016;100(10):1437-1441.
11. Khouri AS, Lari HB, Berezina TL, et al. Long term efficacy of repeat selective laser trabeculoplasty. J Ophthalmic Vis Res. 2014;9(4):444-448.
12. Maslin J, Noecker R. Micropulse trans-scleral cyclophotocoagulation for the treatment of glaucoma. Poster presented at: American Glaucoma Society Annual Meeting; March 3-6, 2016; Fort Lauderdale, FL.




