Best of Technology 2016
Corneal Inlay
Five surgeons nominated the Raindrop Near Vision Inlay (ReVision Optics) the best technology of 2016. This device expands the new category of corneal inlays and represents a significant advance in the treatment of presbyopia, according to Robert J. Weinstock, MD, chief medical editor of CRST. Ophthalmologists “now have a potential surgical presbyopic solution for patients who are plano presbyopes and are not yet at the point where they are a good candidate for a refractive lens exchange or have developed cataracts,” he explained.
Cathleen M. McCabe, MD, of Sarasota, Florida, reported excellent results thus far in her patients, and she expressed excitement at being able to offer the corneal inlay to frustrated emmetropic patients who are relying on readers. She also appreciates that the device can be removed, if necessary, and noted that her patients find this reassuring.
Along these lines, Mitchell A. Jackson, MD, of Lake Villa, Illinois, said, “The instant gratification of these patients day 1 makes it a LASIK-like procedure in terms of near vision recovery.” He stated that the implant fills a gap in options for treating presbyopia.
Weighing in from Bloomington, Minnesota, Y. Ralph Chu, MD, said watching Stephen G. Slade, MD, and Jeffrey Whitman, MD, implant the first Raindrop devices live on Eyetube.net ushered in “a new era for the treatment of presbyopia for all refractive surgeons. I look forward to seeing this technology develop.”
The optics of and the candidates for the Raindrop and the previously approved Kamra (AcuFocus) differ. Dr. Weinstock stated that the corneal shape modification achieved by the former is novel and important. For his part, CRST Editor Emeritus Dr. Slade welcomes new refractive options for patients and said the Raindrop and small-incision lenticule extraction (SMILE) “have the potential to drive the market for all procedures.”
Laser Refractive Surgery
Segueing from Dr. Slade’s remarks, Los Angeles surgeon Uday Devgan nominated SMILE with the VisuMax laser (Carl Zeiss Meditec), which the FDA approved this year for the treatment of myopia. “This may surpass LASIK for safety and efficacy, particularly since there is no flap,” he remarked. Dr. Devgan expects fewer problems with dry eye disease (DED) with SMILE versus LASIK in addition to the absence of flap-related complications and faster recovery of excellent vision (see Listen up for a podcast on SMILE with CRST Editor Emeritus John Doane, MD).
Intraocular Lenses
Three surgeons nominated the Tecnis Symfony and Tecnis Symfony Toric IOLs (both from Abbott) as the year’s most exciting technology: Daniel Chang, MD, of Bakersfield, California; Jason J. Jones, MD, of Sioux City, Iowa; and George O. Waring IV, MD, of Charleston, South Carolina. As the first extended-range-of-vision IOLs on the US market, the Symfony lenses expand patients’ choices and ophthalmologists’ armamentarium, Dr. Jones stated. “Unlike a multifocal lens, which splits light, or an accommodating IOL, which attempts to change focus, this diffractive-technology lens extends the range of useful focus to provide a seamless range of useful vision while providing excellent quality of vision,” he commented.
Dr. Waring remarked, “The diffractive echelette design allows for both extended depth of focus and enhanced chromatic aberration control, resulting in contrast sensitivity comparable to the Tecnis monofocal IOL [Abbott].” The Symfony lens has expanded the pool of patients to whom Dr. Waring can offer a presbyopia-correcting IOL, and he anticipates growth in the presbyopia-correcting IOL market as a result of these approvals (see Watch It Now for a video from Michael Patterson, DO, on implanting this lens).
LISTEN UP
Gary Wörtz, MD, and John Doane, MD, discuss the safety and efficacy of small-incision lenticule extraction or SMILE and how the procedure compares to LASIK.
From Dublin, Ireland, Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin), voted for the Harmoni Modular IOL (ClarVista Medical), which came to the European market in September but is not yet FDA approved. Having used the earlier design, Mr. Cummings said the latest modifications allow “an even simpler technique, often requiring only one hand for insertion.” He added that the lens demonstrates excellent stability in the eye and that it offers the promise of an upgradeable optic in the future, a concept his patients love. “The Harmoni system is a platform technology featuring a universal base component and a full portfolio of optic components so that vision can be tailored to the patient’s needs,” he said.
Calculator
The success of an IOL requires selection of the correct power. With that in mind, both Michael E. Snyder, MD, of Cincinnati and Richard Tipperman, MD, of Philadelphia voted for the Hill-RBF calculator (rbfcalculator.com/index.html).
“As IOL technologies continue to expand and improve, our surgical results are still constrained by our ability to target presbyopia,” Dr. Tipperman commented. “Prior to the Hill-RBF Calculator, all IOL power formulas were essentially iterations of the original vergence power formula. The Hill-RBF formula approaches the problem of IOL power [by] targeting an entirely new way [of] using neural networks, artificial intelligence, and a branch of mathematics known as radial basis function.” Dr. Tipperman said that, at this year’s annual meeting of the American Academy of Ophthalmology (AAO), he was told by Warren Hill, MD, that early studies suggest “this formula will be more accurate than even the Barrett Universal Formula.”
Dr. Snyder remarked, “This novel method of IOL calculation is already breaking records for IOL accuracy within a half-diopter in all categories. Due to the artificial intelligence-based backbone of the technology, the Hill-RBF Calculator will continue to ‘learn’ as more data is added.”
Astigmatic Correction
Joining forces in the Sunshine State, William J. Lahners, MD, of Sarasota and P. Dee G. Stephenson, MD, of Venice asserted that the year’s best new technology is an update from Lensar. Dr. Lahners described Streamline II as “an incredible leap forward in technology that nearly automates astigmatic correction during laser cataract surgery. It connects the Cassini corneal analyzer (i-Optics) wirelessly to the Lensar Laser System, recommending and placing the treatment, then uses iris registration to confirm alignment.” These capabilities “along with adjusting for cyclorotation and now marking the steep axis based on total corneal astigmatism from Cassini onto the eye before surgery,” Dr. Stephenson stated, “[allow] for improved technique and outcomes.”
Dr. Lahners commented, “This has completely eliminated the need to mark [the eye] at the slit lamp or in the OR, as it compensates for cyclotorsion and patient positioning issues.” When implanting toric lenses, he uses the IntelliAxis feature of Streamline II to place intracorneal marks. Based on iris registration, these marks are visible in the OR for toric IOL positioning and on the cornea for a couple of weeks postoperatively, he said, allowing him to verify the IOL’s position and adjust it, if necessary. “This has made toric IOL placement a snap, decreased our enhancement rate, and made postoperative confirmation easy,” he added.
Diagnostic Technology
William I. Bond, MD, of Pekin, Illinois, also went with an update. He selected “the Multi-Luminance Flicker Electroretinogram [Diopsys], which is an ultrahigh-speed stimulation protocol that collects information from the retinal cone system. The threshold level of luminance of the new protocol allows you to quantify the level of dysfunction in patients with vascular retinopathies like CRVO [central retinal vein occlusion] and diabetic retinopathy. The flicker [electroretinogram] can also predict the presence of retinal ischemia in patients with CRVO, which is a useful guide in implementing more (or less) aggressive treatment modalities. It also helps one determine whether intravitreal injections of [antivascular endothelial growth factor] are creating retinal function improvement or not. This has practical office use.”
Corneal Collagen Cross-linking
John Berdahl, MD, of Sioux Falls, South Dakota, cast his vote for corneal collagen cross-linking (CXL), and out of the Quad Cities of Illinois, Lisa Brothers Arbisser, MD, agreed. “It’s high time we begin to catch up with the rest of the world in treating progressive keratoconus and post-LASIK ectasia,” she said. Dr. Arbisser added that she is keeping her eye on this area, particularly the PiXL procedure performed with the Mosaic System (Avedro; not FDA approved), “a minimally invasive procedure being developed for low myopia by preferentially cross-linking portions of the cornea to achieve shape change.” (See Listen up for a podcast on CXL with William Trattler, MD.)
Best Of Research Or Review Article/Presentation
Cataract Surgery
His eye on diagnostics, Dr. Weinstock selected research comparing swept-source optical coherence tomography (OCT) with standard retinal OCT for detecting retinal problems in the cataract population.1 The investigators found that the swept-source OCT of the IOLMaster 700 (Carl Zeiss Meditec) provided useful information about the macula but could not replace a dedicated macular retinal OCT device. Dr. Weinstock elaborated, “This is very important for cataract and refractive surgeons to understand in helping them with recommendations to their patients when they present for cataract surgery. According to this study, the IOLMaster 700 is not adequate to really base decisions on, and we as cataract and refractive surgeons will, for the time being at least, continue to get a retina-dedicated OCT device image to … guide our recommendations for our premium IOL patient population.”
LISTEN UP
William Trattler, MD, describes his experience with corneal collagen cross-linking and the significance of this procedure in a discussion with Gary Wörtz, MD.
With their picks, Karl G. Stonecipher, MD, of Greensboro, North Carolina, and Dr. Bond took opposing sides on laser cataract surgery. Dr. Stonecipher nominated research comparing rates of vitreous loss after phacoemulsification and laser cataract surgery.2 “I believe this article represents a large series of patients from multiple surgeons, and in that environment, the [femtosecond] laser improved safety, which is something we always strive for in our patients,” he said.
In a counterpunch, Dr. Bond voted for what he called a “brilliant” and “convincing” analysis of the safety and efficacy of manual and laser cataract surgery involving 14,567 eyes. The investigators, he said, concluded that there were no significant differences in visual or refractive outcomes between the two groups.3 Dr. Bond commented, “This would seem to confirm a long-held suspicion of mine in a statistically significant manner.” He added that, when acronyms for the laser procedure were being sought, he “suggested femto-assisted refractive cataract extraction, initials/acronym of FARCE.”
For his part, Los Angeles surgeon Robert K. Maloney picked research shared with him by John McAvoy, MD, at the German Eye Surgeons Meeting held in June. Dr. Maloney said the research demonstrates that “the stem cells of the crystalline lens lie along the equator of the lens. This means that we may need to also polish the equator of the bag at the time of cataract surgery to minimize the chance of posterior capsular opacification.”
Dr. Tipperman looked outside the ophthalmic literature to see the future. What he found, he said, “is a landmark article” that is as, “if not more, revolutionary than Harold Ridley’s first use of an IOL.” He elaborated that US and Chinese scientists “describe a new, regenerative medicine approach to remove congenital cataracts in infants, permitting remaining stem cells to regrow functional lenses. In the 12 children treated in this study, all regrew functional lenses from stem cells and obtained improved vision.”4
That outcome is amazing, but Dr. Tipperman said its implications are mind-blowing. “One of the challenges in developing [presbyopia-correcting] IOLs is that, mechanically, it has not been possible to create an artificial lens that performs nearly as well as the healthy phakic human lens,” he explained. “Although it seems like science fiction today, perhaps someday, based on the groundbreaking work in this article, we will actually remove patients’ cataracts and replace them with stem cells [that] will grow into a fully functional and accommodating natural lens!”
Intraocular Lenses
As with his choice of the year’s best technology, Dr. Chang’s vote in this category deals with IOLs. He selected a presentation by Steven C. Schallhorn, MD, that “basically showed that preoperative angle kappa had no bearing on postoperative outcomes” with a multifocal lens implant.5
Los Angeles surgeon Uday Devgan selected research suggesting that “the rate of cataract formation with phakic IOL implantation may be more than we previously thought.”6
Both Dr. Chu and Dr. McCabe expressed excitement about laser technology in development by Perfect Lens. The former nominated an article describing how the femtosecond laser shifts the refractive index inside an IOL.7 “This allows the surgeon in a quick laser-based procedure to not only change the refractive error of a lens but also to reverse multifocality and fine-tune astigmatism,” Dr. Chu explained. “I think this technology is evolving rapidly and may make a significant impact in allowing surgeons to refine patient[s’] outcomes after the lens has stabilized inside the bag.”
Dr. McCabe voted for Dr. Waring’s presentation on the device.8 “This technology could take overall refractive outcomes after cataract surgery to a new level of precision,” she noted.
Glaucoma
Mr. Cummings voted for the published results of the Effectiveness of Early Lens Extraction for the Treatment of Primary Angle-Closure Glaucoma (EAGLE) Study.9 The findings show the value of lens extraction in patients with angle-closure glaucoma, he said. “It’s something that many of us have practiced for years, as it makes so much sense, but now there is a prospective, randomized, multicenter study clearly demonstrating the benefits (and in fact superiority) over peripheral iridotomy,” he explained.
Coming at glaucoma management from another angle, John Berdahl, MD, of Sioux Falls, South Dakota, nominated an article on how poor patients’ adherence is to topical glaucoma therapy.10 He remarked, “The more we learn about drop compliance and adherence, the more we learn that approaches beyond drops like [microinvasive glaucoma surgery] and drug delivery are crucial.”
Endophthalmitis
Drs. Arbisser and Stephenson agreed that the most important research or review was an editorial on intracameral antibiotics and endophthalmitis prevention.11 Javitt wrote the piece based on three articles in Ophthalmology, Dr. Stephenson said. “His review showed that there was a really good reason to use intracameral antibiotics over topical antibiotics, given the average 2.66-fold greater incidence of endophthalmitis with topical versus intracameral antibiotics,” she explained.
According to Dr. Arbisser, the editorial is “a must-read for everyone performing intraocular surgery. … There is no rational reason (but rather only logistical and legal reasons) why every case should not have [an] intracameral antibiotic instilled.”
Cornea
Five panelists’ picks focused on the cornea. Dr. Lahners singled out a presentation on accelerated CXL from Refractive Surgery Subspecialty Day at the 2016 annual meeting of the AAO.12 “This was a very thoughtful and insightful review of the challenges and controversies in the newer accelerated cross-linking protocols,” he explained. “While cross-linking serves only a small percentage of our population with ectatic corneal diseases, its ability to prevent severe visual loss and potential corneal transplantation is profound. Thanks to the approval of CXL in the United States, we now have access to this important treatment modality. It would be great to tell future ophthalmologists, ‘Can you believe that we used to do corneal transplants on keratoconus patients?’”
Both Drs. Snyder and Waring concentrated on specific techniques of corneal surgery. Dr. Snyder favored a presentation by Kashif Baig, MD, MBA, FRCSC, “on a double-punch technique of [Descemet membrane endothelial keratoplasty] tissue, allowing two successful almond-shaped grafts from a single donor eye. This could significantly expand sight-restoring surgery in places where donor tissue is scarce.”13
According to Dr. Waring, the most interesting article of 2016 described a small case series of patients with Fuchs dystrophy who underwent intentional Descemet stripping without endothelial keratoplasty.14 He commented, “Most patients recovered without need for endothelial keratoplasty.” Dr. Waring added that, after a recent conversation with his friend Deepinder Dhaliwal, MD, on her initial positive experience and based on this article, he performed his first cases using this technique.
With practices in the Keystone and Garden States, Cynthia Matossian, MD, nominated an article by Jay Pepose, MD, PhD, on dry eye disease (DED) in CRST’s sister publication Advanced Ocular Care.15 “Since not all patients with DED are symptomatic, it is very important for eye physicians to have objective data for the evaluation of DED,” she said. “The patients also benefit by better understanding their disease process when they are given an objective report or analysis.”
Dr. Jackson also had DED on his mind when he selected the best research article of 2016. “I might be biased, but the landmark publication … for the clinical outcomes of lifitegrast 5% [Xiidra; Shire] for treating the signs and symptoms of dry eye from the OPUS-3 clinical trial paves the way for a much ‘dessicated’ market of ocular surface treatment choices for the last decade or so in the United States,” he said.16
Refractive Surgery
Dr. Slade and Steven J. Dell, MD, chief medical editor of CRST, chose an article surveying all LASIK results published between 2008 and 2015 and demonstrating the procedure’s excellence.17 “This comprehensive review article examined 97 relevant articles representing 67,893 eyes undergoing LASIK after 2008 using modern laser platforms,” Dr. Dell elaborated. “The data demonstrated excellent safety, with loss of 2 or more lines of corrected distance visual acuity occurring in 0.61% of patients. Uncorrected distance visual acuity was better than 20/40 in over 99% of patients. In studies reporting patient satisfaction, only 1.2% of patients were dissatisfied with LASIK.”
Dr. Slade remarked, “LASIK has been around for 25 years, and it is amazing to look at the progress from those early days—laser keratomes, eye trackers, advanced ablations, scanning lasers, and more.”
Best Of Surgical Pearls 2016
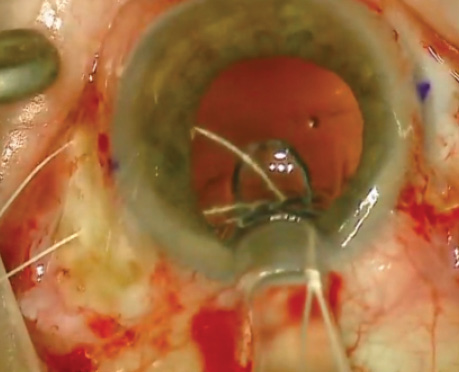
IOL Fixation
“Sometimes, it is the small things that make surgery easier and safer,” Dr. McCabe noted. Both she and Dr. Weinstock voted for a novel technique from Dr. Patterson in which he inserts an Akreos AO60 lens (Bausch + Lomb) with a preloaded Gore-Tex suture (W.L. Gore & Associates; off-label usage) through its haptics for scleral fixation (see Dr. Patterson’s video in Watch It Now). “I have preloaded [a] suture and utilized an inserter in order to insert the lens through a small incision,” Dr. McCabe commented, “but occasionally, the trailing suture would get pinched by the plunger, making the lens very difficult to deliver and increasing the risks of the procedure. Dr. Patterson shows that a pediatric lacrimal probe can be used to push the lens through the cartridge without the inserter, … preventing pinching of the suture during delivery.”
Dr. Devgan chose another variation of this technique shared by Ehsan Rahimy, MD, for the scleral fixation of an Akreos AO MICS Lens (Bausch + Lomb) using a Gore-Tex suture. Dr. Devgan said he has adopted this approach.18
Drs. Dell, Jones, and Stephenson turned to the 2016 annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS). All three nominated the “Transconjunctival Intrascleral IOL Fixation With Double-Needle Technique,” a video for which Shin Yamane, MD, won the grand prize at the ASCRS Film Festival. “This technique permits implantation of a three-piece [posterior chamber] IOL without capsule support while avoiding conjunctival and scleral dissection, scleral suturing, or glue,” Dr. Jones commented.
Dr. Stephenson added that the surgeon externalizes “the haptics through transconjunctival 30-gauge needle tracks in the posterior sulcus plane. The haptics are secured by simply melting the tip of the haptic with a handheld cautery and creating a bulb larger than the needle track. The ends are tucked into the scleral tunnels.” According to Dr. Jones, the technique “is efficient and elegant as well as extremely secure.”
Dr. Bond chose Dr. Maloney’s surgical repositioning of a dislocated IOL through scleral suture fixation of the IOL-capsular bag-capsular tension ring complex.19
IOL Rotation
Mr. Cummings lauded Jorge Alió, MD, PhD, for information shared at the 8th Keratoconus Experts Meeting during the XXXIV Congress of the European Society of Cataract & Refractive Surgery. There, Dr. Alió stated that he uses the Toric Artisan or Toric Artiflex lens (both from Ophtec; neither available in the United States) instead of the Visian TICL (STAAR Surgical; not available in the United States) for patients with keratoconus. “The reason is that the ICL has the tendency to rotate in these keratoconic eyes, as they also have elastic sclera sometimes, and clipping the Artisan/Verisyse [Abbott] onto the iris provides more rotational stability,” Mr. Cummings explained. “I would have some fears about eye rubbing and possibly dislocating the Artisan, but by the time a phakic IOL has been implanted, one would hope that the patient has abandoned the eye rubbing habit.”
WATCH IT NOW
Michael Patterson, DO, shares his innovative technique of using a pediatric Bowman probe to insert a Gore-Tex–fixated IOL.
Dr. Snyder nominated Dr. Hill’s pearl from an interactive symposium on tough cases at the Cataract Surgery: Telling it Like It Is meeting. Dr. Hill described using a notched Henderson Capsular Tension Ring (Morcher; US distributor FCI Ophthalmics) to prevent the rotation of toric IOLs, especially in the capsular bags of highly myopic eyes “with the steep axis at 90º astigmatism,” Dr. Snyder said.
IOL Categorization
Dr. Matossian chose advice from Dr. Chang.20 “The categorization of night vision syndromes into different subsets was very helpful, especially with the diagram for the simulated halo effects for a theoretical monofocal, multifocal, and [extended-depth-of-focus] IOL,” she said.
Cataract Incision
“I never thought that, after 20 years of doing eye surgery, I would say that my favorite pearl of the year was to learn a new technique of making a scleral tunnel!” Dr. Lahners exclaimed. He continued, “A 6-mm PMMA lens can be inserted or removed through a novel wound that has an internal 6-mm diameter but only a 3-mm external wound at the limbus (Figure). This allows us to insert and remove those pesky PMMA lenses without generating the astigmatism of a 6-mm limbal wound. This design can also be used to extend an existing 3-mm wound in tough cases.”21
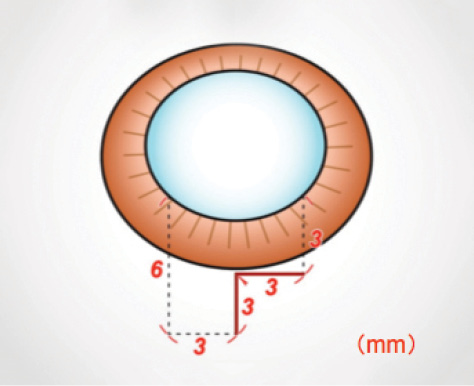
Figure. A 6-mm PMMA IOL can be removed through an L-shaped scleral pocket incision that has an external width of 3 mm.
Laser Cataract Surgery
Dr. Arbisser singled out a tip from Haeussler-Sinangin and colleagues that Berger’s space can be visualized by the onboard OCT of femtosecond laser systems immediately after routine laser cataract surgery.22 “A posterior capsulotomy can be performed (off label) in the majority of cases without puncturing the posterior capsule and instilling [viscoelastic] into Berger’s space,” she commented. “For pediatric cases, adjustment of size for elasticity based on age is needed. [H. Burkhard Dick, MD,] is working on a nomogram.”
WATCH IT NOW
Karl Stonecipher, MD, covers the basics of laser vitreolysis.
Soosan Jacob, MS, FRCS, DNB, demonstrates the presbyopic allogenic refractive lenticule or PEARL technique.
Antibiotic Prophylaxis
Dr. Tipperman voted for a tip on hemorrhagic occlusive vascular retinitis (HORV) from the ASCRS.23 “Ophthalmologists are increasingly recognizing the benefit of intracameral antibiotics at the time of cataract surgery in reducing the risk of endophthalmitis,” he commented. “Prior to this ASCRS clinical alert, vancomycin was the most commonly used intracameral antibiotic in the United States because of its pharmacokinetics and microbial spectrum of action. When the clinical entity of HORV became evident this past year, ASCRS mobilized a task force led by Dr. David Chang to draft an alert regarding the role of vancomycin in HORV to allow surgeons to be well informed regarding this issue and make the best clinical decisions for their patients.”
Vitreous Floaters
Dr. Chu highlighted a tip from Inder Paul Singh, MD, to use the Nd:YAG laser to remove vitreous floaters (see Dr. Stonecipher’s video in Watch It Now). Shared at an Ellex breakfast symposium during the AAO’s annual meeting, the advice was based on Dr. Singh’s 4 years of experience with laser vitreolysis, said Dr. Chu. “Dr. Singh describes great success with this technique with minimal side effects and complications for patients,” Dr. Chu remarked. He added, “We have been traditionally taught that there is nothing we can do for vitreous floaters and that they typically don’t bother patients much and to ignore their significance. We are finding more and more that patients are significantly bothered by floaters and there may be a less invasive way to reduce these symptoms for them.”
Refractive Surgery
Dr. Slade singled out John Doane, MD, for his “flapulorhexis.” The surgeon makes a small entry beneath a flap and opens it with forceps much like a capsulorhexis. “The technique leaves a beautiful[ly] cut epithelial edge and dramatically reduces epithelial ingrowth,” Dr. Slade said. “This is important to me, as I truly disliked doing PRK over LASIK flaps. While primary PRK is an effective procedure, haze rates and imprecision go up dramatically with PRK over a LASIK flap.” Dr. Slade has used the technique “on flaps up to 23 years old. Works every time!”
LISTEN UP
George O. Waring IV, MD, talks with Gary Wörtz, MD, about today’s management of presbyopia.
R. Bruce Wallace III, MD, of Alexandria, Louisiana, highlighted an article of Dr. Waring’s published in CRST this year on how to present what he terms dysfunctional lens syndrome (DLS) to patients.24 “Describing presbyopia and other accompanying refractive errors as a dysfunction that can be remedied can provide the surgeon with a more understandable explanation for their patients and an easier avenue [by which] to list the various options for correcting the different stages of DLS,” Dr. Wallace said. He continued, “If our colleagues embrace DLS as common terminology in the literature, at meetings, and in patient discussions, we may be better able to advance in our quest to help our patients who are troubled with such a common dysfunction.” (See Listen up for a podcast on the today’s management of presbyopia with Dr. Waring.)
Dr. Waring himself made a play on words with his nomination. “The most intriguing surgical pearl is, in fact, the PEARL technique for presbyopia shared with me by my friend and respected colleague Dr. Soosan Jacob from Chennai, India,” he said. “PEARL stands for presbyopic allogenic refractive lenticule inlay. Dr. Jacob described implantation of an allogenic SMILE lenticule into a femtosecond [laser-]enabled stromal pocket for the treatment of presbyopia. The space-occupying allogenic lenticule results in a hyperprolate corneal shape and improved uncorrected reading vision.” Dr. Dell also nominated Dr. Jacob’s PEARL technique. “This intriguing technology has the potential to sidestep the biocompatibility issues that have been problematic for some synthetic inlay patients,” he stated. (See Dr. Jacob’s video in Watch It Now.)
Corneal Surgery
“More and more people are using amniotic membranes,” Dr. Stonecipher remarked. He voted for a technique that Edward Holland, MD, shared. “[Dr. Holland] uses a punch to leave a hole in the middle of the graft so the patient can see through the graft while [he or she is] healing,” Dr. Stonecipher said. “I have recently started cutting them in half, because I don’t have punches, but it’s a great idea.”
1. Hirnschall N, Leisser C, Radda S, et al. Macular disease detection with a swept-source optical coherence tomography-based biometry device in patients scheduled for cataract surgery. J Cataract Refract Surg. 2016;42(4):530-536.
2. Scott WJ, Tauber S, Gessler JA, et al. Comparison of vitreous loss rates between manual phacoemulsification and femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2016;42(7):1003-1008.
3. Popovic M, Campos-Möller X, Schlenker MB, Ahmed II. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14,567 eyes. Ophthalmology. 2016;123(10):2113-2126.
4. Lin H, Ouyang H, Zhu J, et al. Lens regeneration using endogenous stem cells with gain of visual function. Nature. 2016;531(7594):323-328.
5. Schallhorn SC. Large series analysis of the relationship of angle kappa and quality of vision after multifocal IOL implantation. Paper presented at: ASCRS Congress & Symposium; May 6-10, 2016; New Orleans, LA.
6. Guber I, Mouvet V, Bergin C, et al. Clinical outcomes and cataract formation rates in eyes 10 years after posterior phakic lens implantation for myopia [published online ahead of print March 3, 2016]. JAMA Ophthalmol. doi:10.1001/jamaophthalmol.2016.0078.
7. Sahler R, Bille JF, Enright S, et al. Creation of a refractive lens within an existing intraocular lens using a femtosecond laser. J Cataract Refract Surg. 2016;42:1207-1215.
8. Waring GO IV. In vivo refractive index modification of an intraocular lens with a femtosecond laser—Perfect Lens. Paper presented at: AECOS Summer Symposium; July 17, 2016; Deer Valley, UT.
9. Azuara-Blanco A, Burr J, Ramsay C, et al, for the EAGLE study group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016;388:1389-1397.
10. Newman-Casey PA, Blachley T, Lee PP, et al. Patterns of glaucoma medication adherence over four years of follow-up. Ophthalmology. 2015;122(10):2010-2021.
11. Javitt JC. Intracameral antibiotics reduce the risk of endophthalmitis after cataract surgery: does the preponderance of the evidence mandate a global change in practice? Ophthalmology. 2016;123(22):226-231.
12. Kohnen T. Accelerated crosslinking. Paper presented at: AAO Annual Meeting; October 14, 2016; Chicago, IL.
13. Baig K. DMEK from D to K: a step-by-step approach to Descemet’s membrane endothelial keratoplasty. Instructional Course: XXXIV Congress of the ESCRS; September 12, 2016; Copenhagen, Denmark.
14. Borkar DS, Veldman P, Colby KA. Treatment of Fuchs endothelial dystrophy by Descemet stripping without endothelial keratoplasty. Cornea. 2016;35(10):1267-1273.
15. Pepose J. The value of objective data in evaluating DED. Advanced Ocular Care. May/June 2016. http://bit.ly/2fjGP4r. Accessed October 27, 2016.
16. Holland EJ, Luchs J, Karpecki PM, et al. Lifitegrast for the treatment of dry eye disease: results of a phase III, randomized, double-masked, placebo-controlled trial (OPUS-3). Ophthalmology. In press. http://bit.ly/2f9WqRk. Accessed November 1, 2016.
17. Sandoval HP, Donnenfeld ED, Kohnen T, et al. Modern laser in situ keratomileusis outcomes. J Cataract Refract Surg. 2016;42(8):1224-1234.
18. Rahimy E, Khan MA, Gupta OP, Hsu J. Gore-Tex sutured intraocular lens. Retinal Physician. May 1, 2016. http://bit.ly/2eKxWx3. Accessed October 27, 2016.
19. Guttman Krader C. Managing dislocated IOLs with scleral suture fixation. Ophthalmology Times. January 19, 2016. http://bit.ly/1lSXgmI. Accessed October 27, 2016.
20. Chang DH. Night vision and presbyopia-correcting IOLs. CRST. August 2016:16(8);25-26. http://bit.ly/2frEt4v. Accessed October 28, 2016.
21. Beiko G. Smaller is better: 3-mm l-shaped scleral tunnel incision. Paper presented at: AAO Annual Meeting; October 14, 2016; Chicago, IL.
22. Haeussler-Sinangin Y, Schultz T, Holtmann E, Dick HB. Primary posterior capsulotomy in femtosecond laser-assisted cataract surgery: in vivo spectral-domain optical coherence tomography study. J Cataract Refract Surg. 2016;42(9):1339-1344.
23. Clinical alert: HORV association with intraocular vancomycin. ASCRS website. http://www.ascrs.org/node/26101. Accessed October 28, 2016.
24. Waring GO IV. How to present refractive lens exchange to patients. CRST. July 2016;16(7):53-54.