
I recently participated as a clinical investigator at one of 15 sites in the US clinical trial of the Tecnis Symfony IOL (ZXR00; Abbott), the first in the new category of extended-range-of-vision IOLs. The lens is different from a traditional multifocal IOL in that it does not split light between near and distant focal points. Rather, a diffractive echelette design feature extends the range of vision, while achromatic technology reduces chromatic aberration to increase contrast sensitivity and enhance quality of vision. This article shares pivotal FDA trial data on visual outcomes that I presented at the 2016 meeting of the American Society of Cataract and Refractive Surgery.1
In the prospective, randomized, subject- and evaluator-masked study, 148 subjects received the Symfony lens bilaterally and 150 the ZCB00 Tecnis monofocal lens (Abbott). Mean age and sex were similar in both groups.
STUDY RESULTS
Figure 1 shows patients’ uncorrected binocular visual acuity results at 6 months. Monocular and binocular distance visual acuities for the Symfony group were clinically comparable to those of the monofocal control lens group. Monocular intermediate visual acuity with the Symfony lens was 1.7 lines (uncorrected) to 2.4 lines (distance corrected) better than in the control group. Mean binocular UCVA at intermediate distance (66 cm) was 20/20 (0.002 LogMAR) at 6 months, and mean binocular UCVA at near (40 cm) was between 20/25 and 20/32 (0.146 LogMAR).
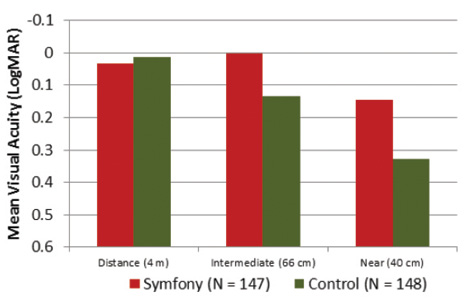
Figure 1. Based on 6-month results from the US clinical trial, patients who receive the Symfony IOL can expect uncorrected binocular results for distance and intermediate of approximately 20/20 and near results between 20/25 and 20/32.
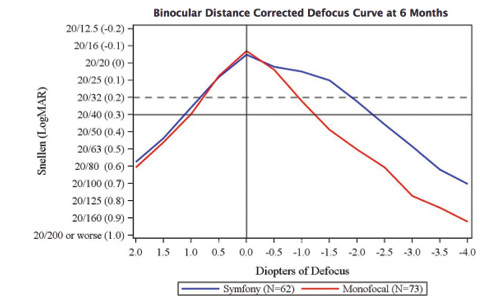
Figure 2. In the US clinical trial, mean binocular visual acuities remained above 20/32 for the Symfony group through intermediate defocus values of 1.50 D (66 cm) while maintaining a 1- to 2-line acuity difference over the monofocal group through 4.00 D of defocus.
My colleagues and I performed robust defocus testing on a subset of the patients in this study; we deliberately defocused them and tested their vision from +2.00 to -4.00 D of defocus. I was encouraged to see that the resulting defocus curve (Figure 2) is almost identical to what was predicted by the optical bench testing of this lens as well as to defocus testing done in other studies.
REDUCED SPECTACLE USE
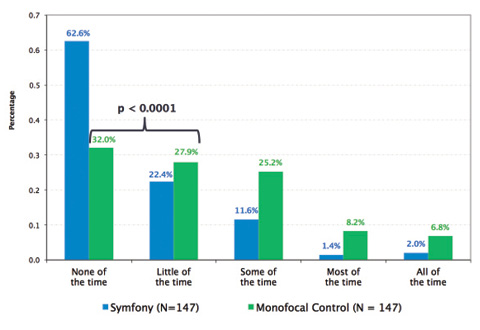
Figure 3. In the US clinical trial, a statistically significantly (P < .001) greater proportion of Symfony subjects compared to controls reported wearing glasses “none/a little of the time.”
A secondary effectiveness endpoint in the clinical trial was a reduction in spectacle wear. The study data show that 85% of Symfony subjects reported wearing glasses “none” or “a little bit” of the time (Figure 3). The majority (63%) reported never wearing glasses, which was nearly twice as many as in the monofocal control group. Still masked to which lens they received and without the benefit of any enhancements to correct residual refractive error, 92% of Symfony patients said they would choose the same IOL again.
I have to admit that I was impressed by how well my patients were able to function without glasses for near activities when they were targeted for distance. Of my 21 study patients, 10 received bilateral Symfony lenses. Most of my patients reported using reading glasses only once or twice per week or even less, so this lens provides fairly robust uncorrected acuity at all distances, something I had not expected to see without some mini-monovision.
NIGHT VISION SYMPTOMS
The Symfony lens spreads light over an extended range instead of directing it to two distinct focal points. This means there is no second focal point that must be suppressed by the brain, as was reflected by the low rate of visual symptoms in the US clinical trial.
On a nondirected symptom questionnaire, the vast majority of subjects in the US clinical trial reported mild or no halos (90%), glare (98%), or starbursts (95%). Of those who did report symptoms, most experienced a moderate rather than a severe level.
I would expect the incidence of unwanted visual phenomena to be even lower outside the clinical trial, when enhancements can be performed, because residual refractive error is the greatest source of glare and halos. I think it is still important to inform patients about the potential for halo formation, but the symptoms my patients described seemed to be less intense than what I have observed in the past with multifocal IOLs; patients deemed symptoms acceptable when they noted them at all.
WHERE THE LENS FITS INTO THE ARMAMENTARIUM
I think the Symfony IOL is going to be a solid performer for patients who desire presbyopic correction. Although my patients were quite satisfied with the degree of spectacle independence, I might also consider targeting the nondominant eye for micromonovision, or I might place a Symfony lens in the dominant eye and a low-add multifocal lens in the nondominant eye to get even more reliable near vision. At the 2016 meeting of the American Society of Cataract and Refractive Surgery, Black reported on intentional micromonovision with the Symfony IOL in both eyes but a -0.50 D target in one eye. This approach provided just a bit more near vision without detracting from distance acuity.2 Although more studies are needed, I think surgeons will have effective options for refractive targeting or mixing and matching within the Tecnis family of lenses to provide patients with seamless blended vision.
I also think the excellent distance vision that the Symfony IOL provides—equivalent to that of a monofocal IOL—opens up the possibility of using this lens in patients in whom I might hesitate to implant a multifocal IOL such as those with mild corneal aberrations or retinal issues. Based on my experience, the Symfony IOL represents an excellent option for improving near and intermediate vision on a very stable lens platform that is no different to implant or monitor than a monofocal IOL. The robust quality of vision and ability to tolerate certain aberrations may also make the Symfony lens a desirable option for post-LASIK eyes in my practice.
1. Jones J. Visual Outcomes of a New Extended Range of Vision IOL. Paper presented at: ASCRS/ASOA Symposium & Congress; May 8, 2016; New Orleans, LA.
2. Black D. Evaluation of reading speed using an extended range of vision presbyopia-correcting IOL. Paper presented at: ASCRS/ASOA Symposium & Congress; May 7, 2016; New Orleans, LA.
Jason J. Jones, MD
• medical director, Jones Eye Clinic, Sioux City, Iowa
• (712) 239-3937; jasonjonesmd@mac.com
• financial disclosure: consultant to Abbott and paid investigator for the FDA clinical trial of the Tecnis Symfony IOL



