Despite its lack of FDA approval, corneal collagen cross-linking (CXL) continues to be a first-line treatment for patients in the United States with keratoconus, post-LASIK ectasia, and pellucid marginal degeneration. Thankfully, numerous clinical trials are available in virtually every state for patients diagnosed with ectatic corneal conditions. CXL has proven to be effective at stopping the progression of keratoconus and other ectatic corneal conditions, and it also enhances quality of vision and corneal shape, with improvement continuing for years after the procedure. Research is ongoing, however, regarding optimal treatment parameters as well as whether CXL should be performed initially as a stand-alone procedure or in combination with surgical modalities such as Intacs (Addition Technology), topography-guided PRK, and conductive keratoplasty.
LONG-TERM RESULTS
A recent study examining the long-term results (10 years) of epithelium-off (epi-off) CXL confirmed that the improvements in corneal shape and vision seen during the first few years after the procedure continue over a decade.1 Not only did patients’ ectasia stabilize, but their corneal shape and BCVA also improved. This study gives clinicians the confidence to tell patients that a single CXL treatment will, in most cases, result in long-term improvement.
Although the initial treatment parameters of a decade ago were effective, numerous innovations have further improved the results of CXL. For example, surgeons now understand that, although treatment can be centered on the middle of the corneal apex in keratoconic eyes, results are better in eyes with peripheral corneal weakness from pellucid marginal degeneration (PMD) when the ultraviolet (UV) light is centered over the thinner part of the cornea located inferiorly. The one concern with peripheral UV light treatments was the risk of damage to conjunctival goblet cells. A recent paper by Dr. Hafezi, however, has confirmed that the conjunctiva is not damaged by UV light during CXL.2
DATA AND DEBATE
Epi-off CXL is currently being studied by Avedro with hopes of FDA approval either in the near term or within a few years. First developed in 1998 by Theo Seiler, MD, PhD, the procedure was initially designed as a 30-minute treatment. Recent research has suggested, however, that exposure times can be shortened when the UV light energy is proportionally increased.3 Many clinical trials, including a phase 3 multicenter randomized trial sponsored by The American-European Congress of Ophthalmic Surgery and Avedro, are evaluating whether the results of higher-energy UV light treatment of shorter duration are the same, better, or worse than those of the traditional 3-mW treatment for 30 minutes. More data should become available during the next year to help clinicians optimize treatment parameters.
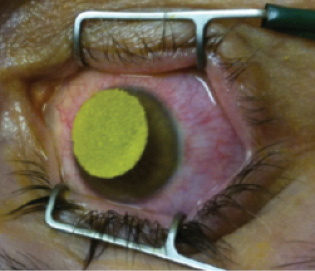
Figure 1. A corneal protector sponge is soaked with riboflavin to help with riboflavin loading during epi-on CXL.

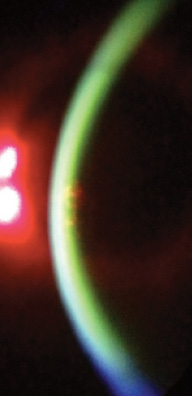
Figure 2. A slit-lamp view confirms sufficient riboflavin in the cornea to proceed with UV light therapy for epi-on CXL.
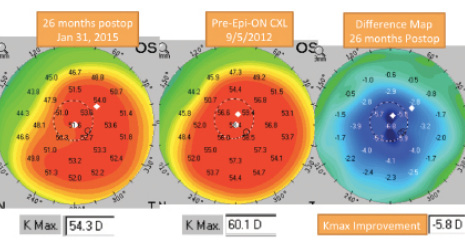
Figure 3. A 35-year-old woman underwent epi-on CXL in 2012. Twenty-six months later, the cornea had flattened significantly.
Whether epithelium-on (epi-on, also known as transepithelial CXL) can be as effective as epi-off has been the subject of controversy. A number of studies have compared the two approaches with mixed outcomes. Some have demonstrated reduced efficacy with epi-on, whereas others have found an equal effect.4,5 Because each study used different formulations of riboflavin and methods, differences in efficacy could be related to the methods rather than to epi-on treatment as a whole. Some keys to improving the efficacy of epi-on therapy are using a riboflavin formula without dextran, placing a corneal protector sponge to maximize riboflavin exposure (Figure 1), and evaluating the cornea at the slit lamp to confirm that sufficient riboflavin is present prior to initiating UV light treatment (Figure 2).
For the past 5 years, the prospective, nonrandomized, multicenter CXL-USA study has enrolled patients with keratoconus, PMD, post-LASIK ectasia, post-RK fluctuations in vision, and Terrien marginal degeneration. In this study, epi-on has proven to be effective, with less than 1% of eyes needing a second treatment.6 In addition, patients have often experienced an improvement in corneal shape and in UCVA and/or BCVA, which can continue for many years (Figure 3).6
ADDITIONAL TREATMENT
After CXL, patients have a variety of choices. Most choose to continue using their current methods of vision correction, either glasses or contact lenses. Many wearing contact lenses switch to scleral designs, which can provide excellent visual acuity and are very friendly to the ocular surface. A small percentage of patients may choose to undergo additional surgery such as topography-guided PRK (available outside the United States) or the placement of Intacs. These procedures can be performed from 6 months to many years after CXL.
An area of intensive research concerns whether combining CXL with other surgical procedures is a more effective approach than performing CXL alone. Outside the United States, a popular combination is topography-guided PRK with CXL, and the results have been very good.7 Another possible pairing is Intacs with CXL.8 Performing CXL 1 day after conductive keratoplasty appears to hold promise (S. Shetty, MD, and R. Rubinfeld, MD, unpublished data, 2015). Although these combined procedures may quicken improvement in corneal shape and visual acuity compared to CXL alone, they potentially carry a higher level of risk, because multiple procedures are being performed.
FUTURE DIRECTIONS
The future of CXL is promising, with the hope of FDA approval in the near term. Innovations continue, including adjustments to the time and energy parameters of UV light exposure, optimization of the location where light is delivered to the cornea, and combinations of CXL with other procedures. n
1. Raiskup F. Corneal collagen crosslinking with riboflavin and ultraviolet-A light in progressive keratoconus: ten-year results. J Cataract Refract Surg. 2015;41(1):41-46.
2. Hafezi F, Mrochen M, Koller T, Seiler T. Current state of CXL (corneal collagen cross-linking): controversies and recommendations. Instructional course presented at: XXXI Congress of the ESCRS; October 7, 2013; Amsterdam, The Netherlands.
3. Mazzotta C, Traversi C, Pardiso A, et al. Pulsed light accelerated crosslinking versus continuous light accelerated crosslinking: one-year results. J Ophthalmol. 2014;2014:604731.
4. Leccisotti A, Islam T. Transepithelial corneal collagen cross-linking in keratoconus. J Refract Surg.
2010;25:1-7.
5. Filippello M, Stagni E, Buccoliero D, et al. Transepithelial cross-linking in keratoconus patients: confocal analysis. Optom Vis Sci. 2012;89(10):e1-7.
6. Trattler W, Rubinfeld R, Correa R, et al. Evaluation of epi-on corneal collagen cross-linking (CXL) at 6 months and 1 year follow-up in patients diagnosed with keratoconus and post-LASIK ectasia. E-poster presented at: XXXII Congress of the ESCRS; September 13-17, 2014; London, England.
7. Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009;25(9):S812-S818.
8. Vicente LL, Boxer Wachler BS. Factors that correlate with improvement in vision after combined Intacs and trans-epithelial corneal crosslinking. Br J Ophthalmol. 2010;94(12):1597-1601.
William B. Trattler, MD
• director of cornea at the Center for Excellence in Eye Care in Miami
• (305) 598-2020; wtrattler@earthlink.net; Twitter @wtrattler
• financial disclosure: holds a financial interest in CXLO