Keratoconjunctivitis sicca remains a widespread yet difficult problem for the cataract and refractive surgeon. According to the International Dry Eye WorkShop, dry eye disease (DED) affects approximately 5 million Americans who are over 50 years old,1 with a prevalence as high as 17% of women and 11.1% of men.2 The preoperative recognition and management of DED are essential to optimize the outcomes of cataract and refractive surgery. A systematic and stepwise approach to treatment depends on a physician's understanding of the underlying etiology and potential exacerbating conditions. Examining the contribution of systemic medications is imperative, because any agent that disturbs one of the components of the tear film (ie, lipid, aqueous, or mucin) has the potential to aggravate dry eye symptoms (Table). After the initiation of a systemic medication that decreases tear production, asymptomatic patients may become symptomatic, and patients with existing DED can experience worsening symptoms. Because basal tear production decreases with age and the use of multiple systemic medications increases, it is essential that clinicians recognize which drugs carry the potential for causing or exacerbating DED.
ANTICHOLINERGIC AGENTS
Mechanism of Action
The great majority of medications that contribute to DED do so through their anticholinergic effects.3 Mechanistically, systemic anticholinergic agents compete with acetylcholine at the postsynaptic muscarinic receptors in the central and peripheral nervous system, blocking the signaling action of acetylcholine. DED occurs because both aqueous and mucin production decrease when anticholinergic medications block the G-protein-coupled signaling from the parasympathetic nerves in the lacrimal gland acini and the conjunctival mucus-producing cells.
The Offenders
Many diverse classes of systemic medications have anticholinergic effects that can cause or worsen DED. Antidepressant medications block norepinephrine and serotonin reuptake and thereby increase amine-dependent synaptic transmission, but the drugs' anticholinergic effect on muscarinic receptors contributes to DED. Because these same agents are also used to treat anxiety, obsessive-compulsive disorders, and even chronic pain, ophthalmologists will frequently encounter patients taking antidepressant medications. There is currently no published evidence by which to stratify antidepressants based on the amount of DED they induce. Based on other anticholinergic side effects (eg, dry mouth), however, tricyclic and heterocyclic antidepressants (eg, amitriptyline, imipramine, nortriptyline, bupropion, venlafaxine) likely induce more ocular dryness than selective serotonin reuptake inhibitors (eg, fluoxetine, sertraline, paroxetine).
Similarly, both first- and second-generation antipsychotic drugs used to treat schizophrenia, behavioral disturbances in patients with dementia, and bipolar mania can induce DED through anticholinergic effects. Based on other systemic anticholinergic side effects, both generations of medication likely cause similar levels of DED. The management of DED in patients with behavioral disturbances can be particularly challenging, because an accurate history can be difficult to obtain and there may be issues with treatment compliance.
Levodopa and pramipexole, used to treat Parkinson disease, have anticholinergic effects that can contribute to DED. Additionally, patients with Parkinson disease have a low blink rate and may concurrently be on antidepressants and antipsychotics, further worsening their ocular surface disease. Treatment challenges arise because this movement disorder can make it difficult for patients to instill eye drops .
H1-antihistamines used to treat allergic rhinitis have varying degrees of anticholinergic properties. Decongestants are often used concurrently and may decrease blood flow to the lacrimal glands by vasoconstriction. Fortunately, the second-generation H1-antihistamines (eg, loratadine, cetirizine, fexofenadine) have a lower affinity for the muscarinic receptors and therefore induce fewer central and peripheral anticholinergic side effects such as DED compared to the first generation (ie, diphenhydramine). Even the intranasal use of antihistamines and decongestants can cause ocular side effects, because high intranasal vascularity leads to high systemic absorption. Topical antihistamines for allergic conjunctivitis induce fewer dry eye symptoms than oral antihistamines, because less medication reaches the lacrimal glands.
Anticholinergic medications used to manage overactive bladder (eg, oxybutynin, tolterodine, fesoterodine) can exacerbate symptomatic complaints of ocular burning, foreign body sensation, and dryness. Extended-release formulations may carry less risk of inducing DED.
Other medications with anticholinergic properties that can cause or worsen DED include the benzodiazepines used as anxiolytics (eg, diazepam, alprazolam), H2 receptor antagonists used for gastroprotection (eg, cimetidine, ranitidine, famotidine), and gastric motility agents (eg, pirenzepine, telenzepine).
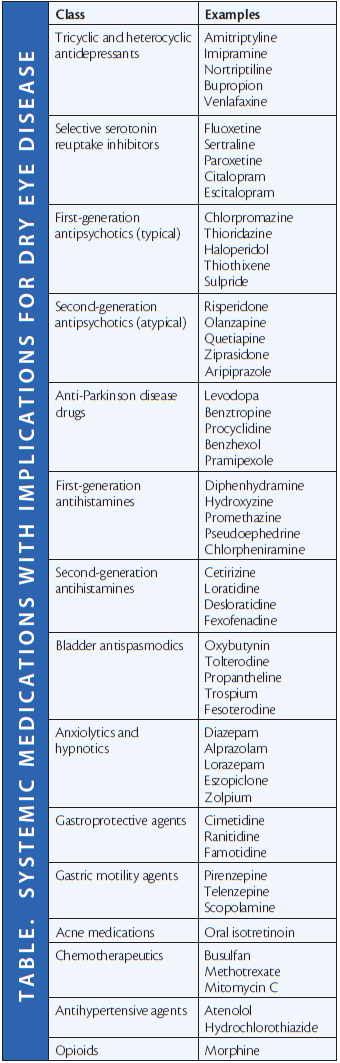
ADDITIONAL AGENTS
Although anticholinergics are the main systemic offenders that induce DED, other medications are also potential contributors. In the younger population being treated for severe acne, oral isotretinoin has been suggested to affect tear stability in a dose-related fashion by inducing atrophy of the meibomian glands and a reduction in basal tear secretion.4,5 Although more rare, chemotherapeutics such as busulfan, methotrexate, and mitomycin C have been reported to alter the tear film and decrease reflex tear secretion.6 Antihypertensive medications such as ß-blockers and diuretics have also been associated with symptomatic complaints of dry eyes, although the mechanism is not clear. Opioids such as morphine and antithyroid hormones may also have the potential to induce symptomatic exacerbation.
AWARENESS
Polypharmacy rises with age. Clinicians must therefore maintain a current list of medications for each patient and update it at every visit. An open line of communication with the prescribing physicians is necessary, because they may not be aware of the ocular drying effect of systemic medications. Reducing or discontinuing a systemic agent implicated in DED should be done in consultation with the prescribing provider after balancing risks, benefits, and symptom severity. Alternatively, a different class of medication or even another drug in the same class could be considered. A thorough understanding of the contribution of systemic medications to DED arms the ophthalmologist with another tool for the complex evaluation and treatment of this multifaceted eye disease. n
1. The epidemiology of dry eye disease: report of the epidemiology subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:93-107.
2. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000;118:1264-1268.
3. Wong J, Lan W, Ong LM, Tong L. Non-hormonal systemic medications and dry eye. Ocul Surf. 2011;9(4):212-226.
4. Fraunfelder FT, LaBraico JM, Mayer SM. Adverse ocular reactions possibly associated with isotretinoin. Am J Ophthalmol. 1985;100:534-537.
5. Aragona P, Cannavo SP, Borgia F, Guarneri F. Utility of studying the ocular surface in patients with acne vulgaris treated with oral isotretinoin: a randomized controlled trial. Br J Ophthalmol. 2005;152:576-578.
6. Maino DM, Tran S, Mehta F. Side effects of chemotherapeutic oculo-toxic agents: a review. Clin Eye Vis Care. 2000;12:113-117.
Sejal R. Amin, MD
• clinical lecturer, Department of Ophthalmology and Visual Sciences, University of Michigan, Ann Arbor, Michigan
Christopher T. Hood, MD
• assistant professor, Department of Ophthalmology and Visual Sciences, University of Michigan, Ann Arbor, Michigan
• (734) 764-5106; hoodc@med.umich.edu