CASE PRESENTATION
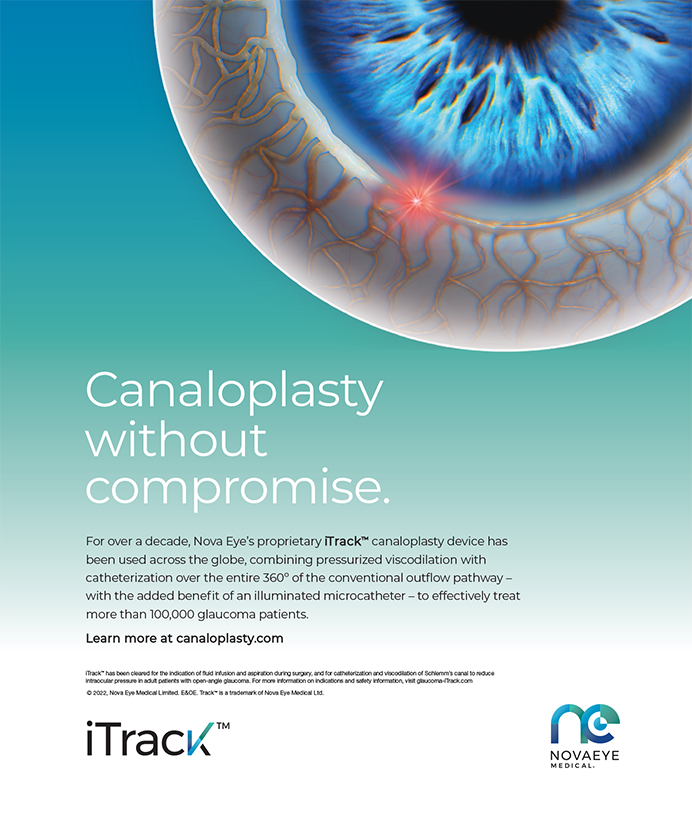
A 73-year-old man with cataracts is very interested in spec- tacle independence. His BCVA is 20/50 OD and 20/25- OS with a minimal refractive error. He has no significant corneal astigmatism. The examination is consistent with a 2+ nuclear sclerotic cataract in the right eye and a 1+ to 2+ nuclear sclerotic cataract in the left eye. A retinal examination reveals a mild macular sheen in the right eye. Macular optical coherence tomography (OCT) reveals an epiretinal membrane (ERM) in the right eye (Figure).
How would you approach this case? How do you normally handle a combined ERM and cataract and why?
—Case prepared by Tal Raviv, MD.
STEVEN DEWEY, MD
As I discuss “spectacle independence” with patients, I strongly redirect them to the phrase “reduced spectacle dependence.” I want them to understand that I am working to achieve the same goal but that I cannot foresee all of their visual needs.
The available options are multifocal IOLs, accommodating IOLs, and monovision. Without a suitable trial of monovision through contact lenses, a patient with a minimal refractive error will typically find the imbalance unacceptable. A suitable approach might be to use the Crystalens (Bausch + Lomb) in a mini-monovision scenario. With the dominant eye corrected for distance, the nondominant eye can be targeted for -1.00 D. Satisfaction with this arrangement will have a lot to do with the patient’s personality and habits in addition to his stature and arm length.
Many ophthalmologists consider multifocal IOLs to be the most reliable option for spectacle independence, and OCT does not preclude the strategy in this case. When a patient receiving a monofocal IOL has an ERM, I will test his or her potential vision extensively—particularly his or her near acuity. If it is J2 or better, I expect a strong improvement in acuity after uncomplicated cataract surgery despite the ERM. Of course, with an aspheric monofocal, the surgeon may not have obtained an OCT scan.
The question here is whether the OCT finding is simply that, a finding, or if it signifies pathology. Frequently, an ERM represents a vitreomacular adhesion that may or may not require treatment. If a monofocal IOL is planned, I would discuss the finding with the patient and recommend an ERM peel if, after cataract surgery, his vision were still limited. I would administer intravitreal triamcinolone at the time of surgery to reduce the risk of cystoid macular edema, and I would incorporate a prolonged postoperative course of topical nonsteroidal anti-inflammatory drugs. In my experience, few patients like this one will need further intervention and, thus, a combined vitreoretinal/cataract procedure.
With regard to the anticipated use of a multifocal IOL, I would have a low threshold for obtaining a retinal consultation for this patient. The referral would both better identify the extent of the problem and help the patient understand the limitations of the technology in his situation. The results of that evaluation would outline the best options to present to the patient to achieve his goals.
RICHARD J. MACKOOL, MD
This patient appears to have an ERM that is mainly perimacular, so he may still have excellent foveal function. Nevertheless, the macular findings make him less than an ideal candidate for a presbyopia-correcting IOL—diffractive multifocal, refractive multifocal, or accommodating. All of these lenses have a low modulation transfer function, and they are generally best reserved for patients with no current or impending disease of the macula, optic nerve, or cornea. Furthermore, unless bilateral cataract surgery is planned, monocular implantation of a multifocal IOL is generally to be avoided, because many patients will be uncomfortable with a multifocal lens in one eye while the other is phakic.
An ERM often causes permanent and progressive retinal damage, and it can do so within months. In an eye that has a cataractous lens, it can be difficult or impossible to determine how much of the acuity loss is secondary to the lenticular opacity and how much is attributable to the ERM. Cataract extraction, of course, permits determination of how much acuity loss, if any, is being caused by the ERM. The surgeon can then decide whether or not to remove the ERM based upon its known impact on the patient’s visual acuity, the progression of acuity loss, etc. The implantation of a multifocal IOL could muddy the waters: if the patient has a poor result, then the relative contribution of the IOL and the ERM could be difficult to determine.
This patient should undergo cataract extraction and implantation of a monofocal lens in his right eye. The impact of the ERM and the advisability of vitrectomy/ ERM removal can then be readily determined. If and when the patient subsequently undergoes cataract extraction in his left eye, the surgeon can determine the target refraction after considering the refractive and acuity results of the right eye. If they are excellent (eg, near plano refraction, excellent acuity, and no distortion, as they are likely to be), targeting myopia of -0.50 to -1.00 D in the patient’s left eye would be reasonable.
TOBIAS H. NEUHANN, MD
The patient’s interest in spectacle independence is understandable. Nevertheless, 100% spectacle independence is not currently available, even with the trifocal IOLs from PhysIOL or Carl Zeiss Meditec (products not approved by the FDA). Patients will always have a situation in which they require glasses for near vision or for excellent distance vision in dim light. For that reason, it would be important to assess this patient’s expectations and how the available options might perform. (Corneal refractive surgery is not a good choice in this case and will therefore not be discussed.)
One alternative here is monovision. For this strategy, I would implant a monofocal, aspheric, blue-light–filtering IOL targeting distance vision after ERM surgery on the patient’s right eye. I would implant a monofocal, aspheric, blue-light–filtering IOL targeting near vision (-1.50 D) in his left eye. Vice versa I would not recommend.
The second and third alternatives are mono-multivision. One strategy would be to implant a monofocal, aspheric, blue-light–filtering IOL targeting distance vision after ERM surgery on the patient’s right eye. His left eye would receive a trifocal, aspheric, blue-light–filtering IOL (Finevision; PhysIOL; not available in the United States). Alternatively, a monofocal, aspheric, blue-light–filtering IOL targeting distance vision could be implanted after ERM surgery on his right eye. The patient’s left eye would receive a monofocal, aspheric, blue-light–filtering IOL correcting for distance vision. If he were unhappy with reading glasses and wanted a better solution, a possibility outside the United States would be a super thin, add-on multifocal IOL (Rayner Intraocular Lenses or 1stQ).
The fourth alternative is light myopia. The patient would receive a monofocal, aspheric, blue-light–filtering IOL in both eyes with a target of -1.00 D. He would not achieve spectacle independence, but the outcome might be satisfactory, depending on his expectations.
In most cases like this one, I recommend the first alternative. I have found that, years later, an ERM develops in the second eye of patients such as this one. The performance of a multi- or trifocal IOL is then really poor, whereas a monofocal IOL still provides the best possible visual acuity.
STEVEN G. SAFRAN, MD
The three main questions raised by this case are as follows:
-
What effect is the ERM having on the patient’s current visual function?
-
What is the risk that the membrane will progress and affect visual function after cataract surgery?
-
What is the risk that the patient will need vitreoretinal surgery to remove the ERM? How would that affect decisions on staging and the type of IOL? What impact might vitreoretinal surgery have on the support and function of the IOL, and how will the IOL affect the retina surgeon’s efforts?
It can be impossible to tell on examination how much an ERM is affecting vision. Some clues on spectral domain OCT can help surgeons determine what is going on. Although the OCT scan provided does not seem to be of particularly high definition, it appears that the central fovea (the foveola) has been spared, that there is no tenting distortion or thickening, and that the inner segment-outer segment junction of the photoreceptors (commonly referred to as the ellipsoid zone) is continuous and normal. Based on this OCT scan, I do not believe that the ERM is affecting visual function to a great degree at this time. The fact that the membrane appears discontinuous over the foveola is also encouraging in terms of the patient’s prognosis.
There is some risk that the ERM will progress in time and affect vision, but in my experience, patients who have an ERM that looks like this on OCT tend to do quite well. I would be comfortable offering this patient a Crystalens or even a multifocal IOL if this were the second eye and the patient were already satisfied with a multifocal lens in his first eye. In general, however, I prefer to avoid multifocal IOLs if an ERM is detected. Even if the membrane is not currently affecting visual function, the patient may be at increased risk of cystoid macular edema or progression of the membrane over time, which could be a “deal breaker” with a multifocal IOL.
I would offer this patient cataract surgery with a Crystalens. I would advise him that, although the IOL would improve his uncorrected distance and intermediate vision, he should still expect to need some help reading fine print. I would place a capsular tension ring at the time of cataract surgery to help stabilize the bag in case the patient requires a pars plana vitrectomy for the ERM in the future. Before proceeding with surgery, I would try to clearly explain the patient’s situation to him and ensure that he grasped the complexity of the issues. I would be quick to select a standard monofocal implant or even defer surgery if I felt either were indicated by the patient’s response to this discussion.
Section Editor Lisa Brothers Arbisser, MD, holds an emeritus position at Eye Surgeons Associates, located in the Iowa and Illinois Quad Cities. She is also an adjunct associate professor at the John A. Moran Eye Center of the University of Utah in Salt Lake City.
Section Editor Tal Raviv, MD, is founder and director of the Eye Center of New York and a clinical associate professor of ophthalmology at the New York Eye and Ear Infirmary of Mount Sinai. Dr. Raviv may be reached at (212) 889-3550; talraviv@eyecenterofny.com.
Section Editor Audrey R. Talley Rostov, MD, is in private practice with Northwest Eye Surgeons in Seattle.
Steven Dewey, MD, is in private practice with Colorado Springs Health Partners in Colorado Springs, Colorado. He acknowledged no financial interest in the product or company he mentioned. Dr. Dewey may be reached at sdewey@cshp.net.
Richard J. Mackool, MD, is the director of the Mackool Eye Institute and Laser Center in Astoria, New York. Dr. Mackool may be reached at (718) 728-3400, ext 256; mackooleye@aol.com.
Tobias H. Neuhann, MD, is the medical director of AaM Augenklinik am Marienplatz in Munich, Germany. He acknowledged no financial interest in the products or companies he mentioned. Dr. Neuhann may be reached at +4989 230 8890; sekretariat@a-a-m.de.
Steven G. Safran, MD, is in private practice in Lawrenceville, New Jersey. He is a speaker for Bausch + Lomb. Dr. Safran may be reached at (609) 896-3931; safran12@comcast.net.