With the continued progress in anterior segment surgery, the outcomes of both cataract and refractive surgery continue to improve. These advances have raised patients' expectations. Recently, attention has focused on the ocular surface, as ophthalmologists have come to understand its tremendous impact on surgical outcomes and on patients' vision in general. Several diagnostic tests made available during the past few years allow eye care practitioners to evaluate the ocular surface. This article describes three of the diagnostic tests available and discusses how I use them in my practice.
TEAR FILM OSMOLARITY
There are many methods by which to evaluate the tear film but no consensus on which is the best. It can be quite difficult to interpret results and to monitor patients' response to therapy with many of the existing methods. For these reasons, the assessment of tear film osmolarity has assumed a prominent role in the analysis of the ocular surface. An increase in tear film osmolarity is a hallmark of dry eye disease (DED) and is considered to be the predominant mechanism in the development of surface damage from the disease.1,2 In fact, tear film osmolarity has been reported to be the single best marker for DED.1,2
Tear film osmolarity analysis became much easier upon the release of the TearLab Osmolarity System (TearLab; Figure 1). I have multiple units in my office and could not function without them. Whereas many of the other methods of evaluating the tear film are subjective, the TearLab Osmolarity System gives me an objective number with which to grade the tear film. Not only does this feature help me to diagnose DED and assess its severity, but it also gives me a reliable tool with which to monitor patients' response to therapy. I also regularly use this system to evaluate my preoperative patients. Quite often, the tear film is overlooked prior to cataract or refractive surgery, even though its health can affect the final outcome of the procedure. With this device, I can detect tear film abnormalities that need to be treated before proceeding with surgery. A poor ocular surface can render preoperative measurements and IOL calculations inaccurate and lead to postoperative visual aberrations and patients' complaints.
InflammaDry
Ocular surface inflammation is thought to lead to damage in patients with DED. Numerous inflammatory components have been found to be elevated in DED. Among these constituents is matrix metalloproteinase 9 (MMP-9).3 InflammaDry (Rapid Pathogen Screening) detects the presence of MMP-9 in the tear film. A positive test result, indicating inflammation, may suggest the use of anti-inflammatory medications. I prefer not to perform punctal occlusion initially for an eye with significant inflammation. On the other hand, in the absence of inflammation, punctal occlusion may be appropriate treatment for an aqueous-deficient patient.
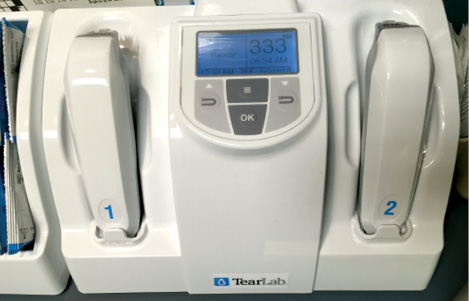
Figure 1. The TearLab Osmolarity System.
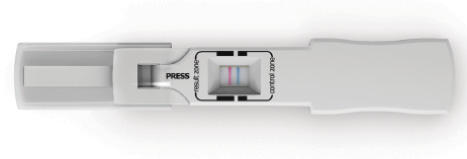
Figure 2. The AdenoPlus diagnostic test.
AdenoPlus
Quite frequently, a patient presents to the office with red, irritated eyes. Although DED is frequently included in the differential diagnosis, infection should also be considered. Conjunctivitis is frequently seen by ophthalmologists, optometrists, and primary care physicians and in urgent care or emergency room settings. Because the type of infection is usually difficult to determine, it is not unusual for patients to receive a prescription for an antibiotic eye drop even though they do not have a bacterial infection. The AdenoPlus device (Rapid Pathogen Screening) is sensitive and specific for detecting the adenovirus as the source of the infection,4 which may significantly alter patients' management (Figure 2).
Just recently, I saw a patient with red, itchy eyes. I initially diagnosed blepharitis and felt that there was probably an allergic component to her symptoms as well. My plan was to prescribe an antibiotic-steroid drop. To my surprise, her AdenoPlus test result was positive for adenovirus. I therefore did not prescribe the fixed-combination drop, because the antibiotic was not necessary. Instead, I gave her lubricants and explained to her the expected course of this type of infection. The test result also alerted my staff to clean the examination room extensively so as not to expose other patients to this highly contagious virus.
CONCLUSION
This article discusses just three currently available devices and my thoughts on how they can be incorporated into the ophthalmology practice. More options are on the way. n
1. Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792-798.
2. International Dry Eye Workshop. The definition and classification of dry eye disease. In: Report of the International Dry Eye Workshop (DEWS). Ocul Surf. 2007;5(2):75-92.
3. Sambursky R, Davitt WF, Latkany R, et al. Sensitivity and specificity of a point-of-care matrix metalloproteinase 9 immunoassay for diagnosing inflammation related to dry eye. JAMA Ophthalmol. 2013;131(1):24-28.
4. Sambursky R, Trattler W, Tauber S, et al. Sensitivity and specificity of the AdenoPlus test for diagnosing adenoviral conjunctivitis. JAMA Ophthalmol. 2013;131(1):17-22.
Kenneth A. Beckman, MD
• clinical assistant professor of ophthalmology at Comprehensive EyeCare of Central Ohio, Ohio State University, Westerville, Ohio
• (614) 890-5692; kenbeckman22@aol.com; Twitter @kab822
• financial disclosure: consultant to TearLab and, since writing this article, investor in Rapid Pathogen Screening


