CASE PRESENTATION
A 39-year-old woman presents for a cataract evaluation. In 2009, the patient underwent retinal detachment (RD) repair with a scleral buckle and gas tamponade as well as a vitrectomy in the right eye and laser retinopexy for retinal tears in both eyes.
Since undergoing the retinal repairs, she has had intermittent blurry near vision and depth perception issues in the right eye, but these symptoms have worsened progressively during the past several months. The patient reports experiencing a macula-on RD and states that she never lost central vision. She says her visual acuity after the RD repair was 20/20 OD before the recent diagnosis of a cataract.
On examination, the patient’s UCVA is counting fingers at 3 feet OU. Her BSCVA is 20/40-2 OD with a refraction of -10.50 -1.75 x 135º and 20/20 OS with a refraction of -8.50 -0.75 x 40º. With glare testing, her visual acuity is light perception OD and 20/25 OS. During all waking hours, she wears toric soft contact lenses (Acuvue, Johnson & Johnson Vision; OD: -9.00 D, 8.6-mm base curve, 14.5-mm diameter; OS: -8.00 D, 8.4-mm base curve, 14.0-mm diameter). She rarely wears glasses (Figure 1). Her left eye is dominant on testing, but she is unsure if this has always been true.
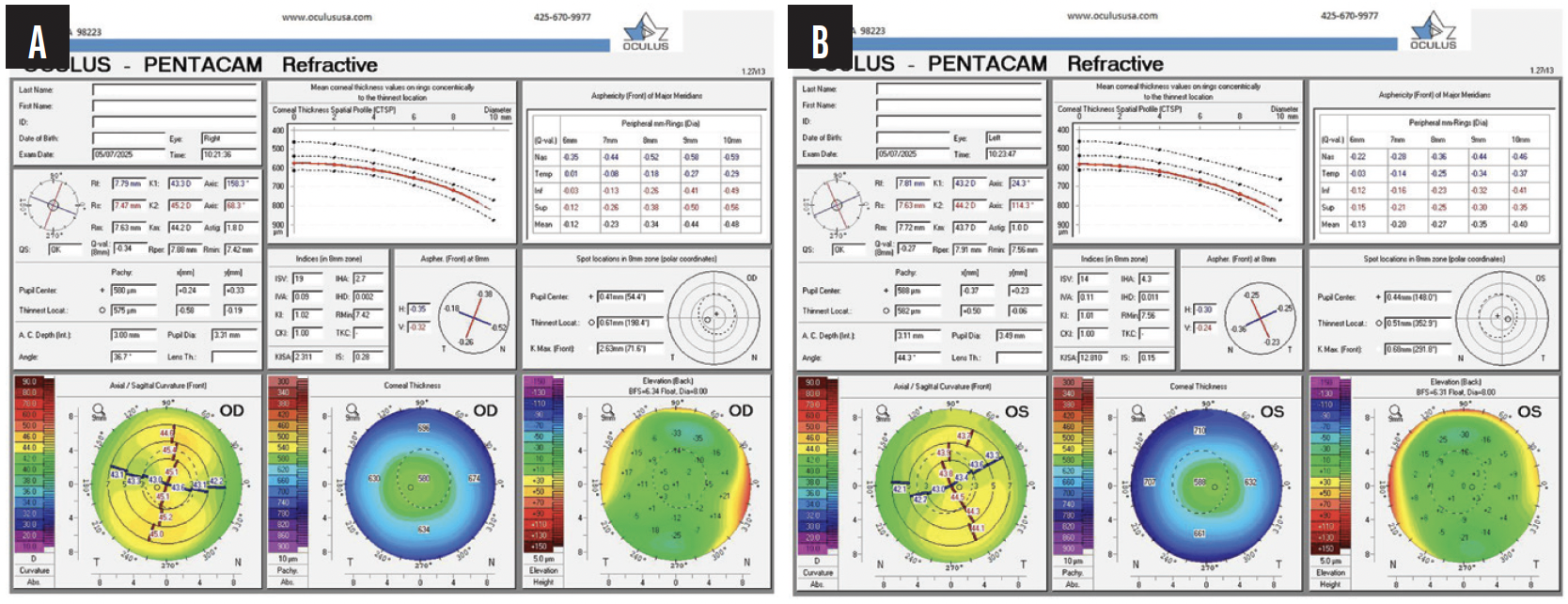
Figure 1. Measurements with the Pentacam (Oculus Optikgeräte) show regular astigmatism, minimal higher-order aberrations, no evidence of keratoconus precluding laser vision correction, and an adequate anterior chamber depth for an EVO ICL.
A slit-lamp examination reveals a 2+ nuclear cataract and 2+ to 3+ posterior subcapsular cataract in the right eye and a trace nuclear cataract in the left eye. A fundus examination finds extensive retinal scarring in the periphery of the right eye status post RD repair and laser retinopexy scars in the left eye (Figure 2). OCT shows a healthy macula and a partial posterior vitreous detachment (PVD) in the left eye and mild irregularity of the macula in the right eye (Figure 3). No PVD is evident in the left eye. Her medical history and examination findings are otherwise unremarkable (Figure 4).

Figure 2. Fundus photography shows extensive chorioretinal scarring status post RD repair with some changes encroaching on the macula in the right eye (A) and peripheral laser retinopexy scars and myopic changes nasally in the macula in the left eye (B).

Figure 3. OCT of the right eye shows minimal disruption to the foveal architecture and no significant edema or epiretinal membrane.

Figure 4. Biometry with the Argos finds high axial myopia and astigmatism, both greater in the right eye than the left.
The patient is a stay-at-home mother who homeschools her children and runs a nonprofit organization for homeschooled children. Her hobbies include digital art and laser cutting. She desires the best range of vision possible. Specifically, she wants to see clearly at distance without correction and to minimize her dependence on reading glasses if possible. She has not tried monovision or multifocal contact lenses. She realizes during the consultation that her blurry near vision heralds the onset of presbyopia.
How would you proceed? The patient has reasonable expectations and is willing to trust your recommendations. Is she a candidate for a diffractive multifocal lens or a Light Adjustable Lens (LAL; RxSight) in her right eye? If not, which type of IOL and what refractive target would you recommend? She has no visual complaints regarding contact lens correction in her left eye. Would you recommend surgical intervention? How would the plan for the left eye affect IOL selection and the refractive target for the right eye?
— Case prepared by Neda Nikpoor, MD

ASHLEY CRANE, MD
Cataract surgery planning can be particularly challenging when the patient has a history of RD in the fellow eye. A nuanced approach is required to minimize risk. As a retina surgeon who frequently manages such patients, I often collaborate with cataract surgeons to guide surgical timing and optimize long-term outcomes. In this situation, I would recommend exercising caution before proceeding with cataract surgery on the patient’s left eye.
A critical first step would be to determine whether a PVD is present. Performing cataract surgery on an eye without a PVD significantly increases the risk of retinal tears and subsequent detachment, and the risk is even higher in patients who have already experienced an RD in the contralateral eye. I would recommend obtaining a high-resolution OCT scan of the macula to assess the status of the posterior hyaloid face. If its status is still unclear, I would obtain OCT of the retinal nerve fiber layer to provide additional insight into whether the hyaloid is attached.
If the posterior hyaloid remains adherent, I would advise deferring cataract surgery and continuing contact lens wear. Delaying intervention until a spontaneous PVD occurs would meaningfully reduce the risk of postoperative retinal complications. Another consideration is that, should an RD occur that requires repair with a scleral buckle, prior cataract surgery could result in an unfavorable refractive outcome—typically significant myopia. Delaying surgery until the eye’s risk profile improves would best protect both its retinal integrity and refractive stability.

CHASE A. LUDWIG, MD, MS
The patient presents with a favorable retinal profile despite her history of RD repair. OCT imaging demonstrates an intact subfoveal ellipsoid zone, corroborating her report of a macula-on detachment and excellent postoperative visual acuity before cataract progression. Her decline in vision is consistent with lens opacity and buckle-induced axial elongation rather than recurrent retinal pathology.
My colleagues and I recently evaluated the risk of recurrent RD after cataract surgery in eyes with a history of repair. Our large claims-based analysis (not yet published) found that repeat detachment occurred in 8.8% of cases overall, with the highest incidence in patients 18 to 35 years of age. Although myopia showed only a nonsignificant trend toward increased risk, particularly in patients with high or pathologic myopia beyond 1 year, this 39-year-old patient with high myopia and a history of bilateral retinal tears requires vigilant postoperative monitoring.
I would avoid diffractive multifocal IOLs because they can reduce contrast sensitivity and cause dysphotopsias, which is a concern in an eye already compromised by prior retinal surgery. An LAL holds some appeal for its ability to fine-tune outcomes, particularly in the setting of buckle-related refractive unpredictability, but its limited adjustment range and the need for multiple light treatments make it less practical in this situation.
I would favor a monofocal or toric monofocal IOL with a refractive target of modest myopia (-1.50 D) in the right eye. This approach would respect the dominance of the left eye, preserve the patient’s functional near vision, and maintain refractive flexibility should the fellow eye require intervention in the future. Given her occupational demands and visual goals, this conservative strategy would optimize both safety and functional outcomes while minimizing presbyopic dependence.
Again, close retinal surveillance would be essential given her risk profile and bilateral involvement.

BRIAN SHAFER, MD
Given the patient’s history of pathologic myopia, RD, and subtle macular irregularities, I do not think a diffractive multifocal lens would be a good choice. Although these lenses can offer excellent near vision, they split incoming light between multiple focal points, which reduces the total light available for each image. In someone with her retinal history, I would want to ensure that as much light as possible reaches the retina to support her quality of vision, both at present and in the event of future retinal changes.
In this situation, I believe the value of an extended range of vision would outweigh the benefit of adjustable monofocality. If the patient experiences a repeat RD in the future that requires silicone oil, moreover, an LAL would be contraindicated. Although the risk of a recurrent RD decreased after the vitrectomy and subsequent stabilization, it would still factor into my decision-making.
For the right eye, I would recommend a Clareon Vivity Toric lens (Alcon) with a refractive target of plano. This lens should provide the patient with excellent uncorrected distance visual acuity (UDVA) and a functional intermediate range for daily activities such as digital art and laser cutting and preserve maximum light delivery to the retina compared to diffractive designs. The axis and magnitude of astigmatism are consistent between tomography and biometry, giving me confidence that an accurate toric outcome can be achieved.
I would monitor the patient’s tolerance of any postoperative anisometropia. If she remains comfortable in her current contact lens, no further intervention would be required. If anisometropia becomes bothersome, I would consider implanting an EVO ICL (STAAR Surgical), given her high myopia and clear crystalline lens. Before committing to surgery, a contact lens trial of a mild undercorrection in her left eye would be conducted to determine if this strategy preserves a little near function and can delay full presbyopic symptoms.
I would expect this plan to maximize the visual potential in the patient’s right eye, ensure the greatest possible light utilization for a retina with preexisting vulnerabilities, and leave the left eye flexible for whatever path is determined to be most beneficial postoperatively.

WHAT I DID: NEDA NIKPOOR, MD
Cataract surgery was planned for the right eye. I explained to the patient that a multifocal IOL was not ideal because of the eye’s unclear visual potential after RD and the phakic status of the fellow eye. The most conservative option was a monofocal IOL, and because her right eye was nondominant and she was starting to experience presbyopia symptoms, the decision was between a distance or near target. Given her high axial myopia and the challenge posed by effective lens position, we also discussed an LAL. Owing to the risk of recurrent RD, which would pose a problem if silicone oil were necessary for repair, however, a fixed-power monofocal IOL was selected.
Because she had adapted to the poor vision in her right eye, the patient thought she could tolerate monovision well. A monofocal toric IOL with a refractive target of -1.50 D was chosen. A greater amount of monovision was elected than she currently needed to allow her to enjoy the benefit of monovision for decades to come. We discussed the options of contact lens wear, a LASIK enhancement, or a piggyback LAL if her brain did not adapt to monovision and she desired a change in target. Given her retinal status, a Tecnis Eyhance toric IOL (Johnson & Johnson Vision) was implanted to extend depth of focus somewhat without degrading visual quality.
We discussed continued contact lens wear versus refractive surgery for the left eye. The patient desired surgery. I advised against cataract surgery owing to high risk of RD in a young myopic patient who has not yet had a PVD (https://medisch.fyeo.nl/retinal-detachment/retinal-detachment-calculator). Given her refractive error, the patient elected an EVO ICL with a refractive target of plano.
After a discussion of the risks, the patient opted for immediately sequential bilateral surgery for convenience.
One day postoperatively, she reported trouble with depth perception in the right eye due to pupillary dilation, but she said the vision in her left eye was sharp, “better than glasses or contact lenses.” Her UDVA was 20/60 OD and 20/15 OS. Her uncorrected near visual acuity (UNVA) was J5 OD and J1+ OS.
At 1 week, the patient was struggling to adapt to monovision and reported feeling dizzy and disoriented when looking up immediately after viewing her phone, computer, or anything up close. Her UDVA was 20/200+1 OD and 20/15 OS. Her UNVA was J1+ OD and J1+ OS.
One month after surgery, the patient had fully adapted to monovision and was highly satisfied with her vision. Her UDVA was 20/80-2 OD, 20/20 OS, and 20/15 OU. Her UNVA was J1 OD, J1+ OS, and J1+ OU. Her BCVA was 20/15 and J1 with a manifest refraction of -1.00 -1.00 x 0.15º OD and 20/15 and J1 with a manifest refraction of +0.00 -0.25 x 180º OS.




