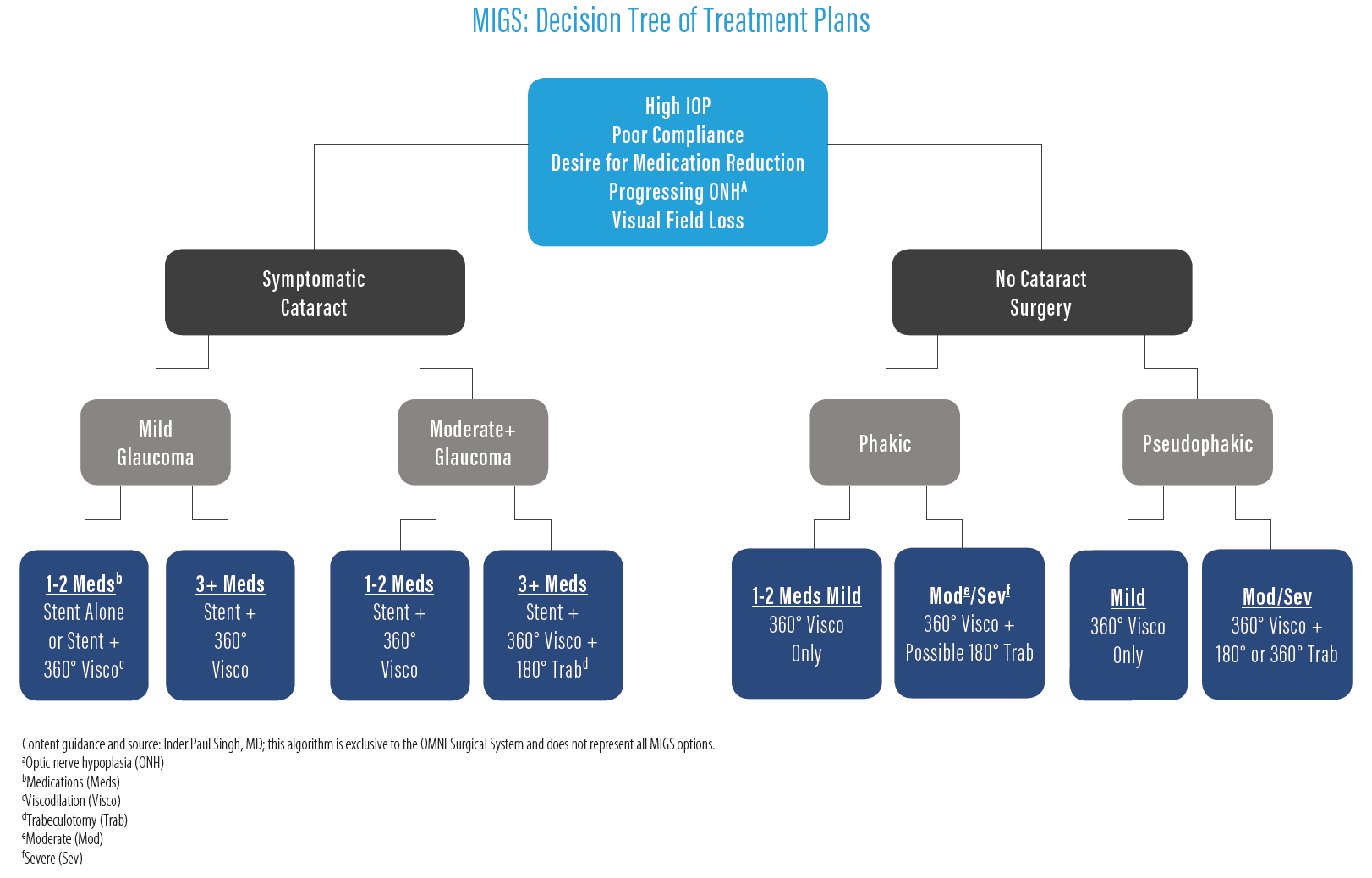
MIGS has created a market of devices that target different pathways with different mechanisms. This provides ophthalmologists today with a multitude of options to consider and creates a decision tree of choices leading to a range of procedures tailored to each patient’s diagnosis and treatment plan. These options force us to determine where in the aqueous outflow pathway we want to address when creating the proper treatment plan. While the dramatic increase in MIGS options may seem complicated, I have developed an algorithm to help me navigate the options.
Options to Target Points of Resistance to Outflow
There are multiple options to address the different segments of the conventional outflow pathway: trabecular meshwork (TM), Schlemm’s canal, and the distal collector channels. The iStent (Glaukos) works primarily by bypassing the TM; the Hydrus Microstent (Ivantis) bypasses the TM and scaffolds Schlemm’s canal (both iStent and Hydrus stents are approved for use only at the time of cataract surgery); goniotomy using a blade such as the Kahook Dual Blade (New World Medical) unroofs Schlemm’s canal by removing a strip of TM; iTrack Surgical Systems (Ellex) uses a lighted tip catheter to break herniations and push viscoelastic into the distal collector channels; and the OMNI Surgical System (Sight Sciences) is designed as a stand-alone application, or in conjunction with cataract surgery, to also break canal herniations and push viscoelastic into the distal collector channels with the added benefit of providing the option of cutting the TM, thereby performing an ab-interno trabeculotomy with the same single-handed device.
The Decision Tree
How do we start down the path of making the right decisions for our patients (see MIGS: Decision Tree of Treatment Plans)? The first thing I do is decide on a target IOP range and identify the severity of the level of disease. Different MIGS devices can be used to address specific patient pathophysiology and target IOP. To achieve this, I examine visual fields and the optic nerve to gauge the severity of glaucoma and the rate of progression. Most of the mild to moderate patients require a target IOP in the middle teens. The other factor is determining the severity of resistance of outflow. Traditionally, we categorize the severity of glaucoma by examining the extent of visual field loss, which sets the target IOP, but the resistance of outflow needs to be considered as well to help determine the best way to achieve that target IOP. In almost all cases, I want to hedge my bets and address possible resistance to outflow through distal pathways as well. Becoming familiar with all available MIGS procedures helps a surgeon’s journey through the decision tree towards obtaining that established targeted pressure. The challenge is that there is no preoperative test to determine where the outflow resistance exists. In practice, I use 1) number of medications, 2) degree of IOP, and even 3) history of response to laser trabeculoplasty to raise suspicion for resistance behind the TM. Since not all the resistance to outflow is in the TM, we often need to target the entire conventional outflow pathway to reduce IOP, from TM to canal all the way to the distal channels. Viscodilating devices like the OMNI can provide the ability to tackle multiple points of resistance and even combine with a stent procedure in an efficient and safe manner.
MIGS Is not just for your Cataract Patients
Another key for deciding the right procedure is the lens status. For example, do they have a cataract that needs to be addressed now, or will they require cataract surgery in the future? Some MIGS devices and procedures are only approved for use at the time of cataract surgery, like the iStent or Hydrus Microstent. If a patient is ready for cataract surgery, I will often perform the cataract with a stent procedure and perform a viscodilating procedure at the same time to further address the resistance in the canal and distal channels. With the OMNI device, I can efficiently choose to perform a 180° or 360° viscodilation, or even add 180° trabeculotomy depending on the patient’s potential outflow resistance location. Regardless of disease severity, if the patient is using multiple glaucoma drops, and/or if the IOP is high, I assume the resistance is not localized solely in the TM, but also likely in the canal and beyond. I therefore perform concomitant viscodilation to offer the chance to address the entire outflow system along with the stent in hopes of providing the best chance of reducing IOP and medication burden.
For glaucoma patients not needing cataract surgery, there is a different pathway. Approved stand-alone MIGS treatments are viscodilation, cutting/stripping, endoscopic cyclophotocoagulation, or subconjunctival bypass. In mild phakic patients, I perform a viscodilation/canaloplasty procedure leaving the TM untouched and allowing opportunities for secondary surgery, if needed, such as a stent in the future. For moderate to severe glaucoma, I combine viscodilation with a cutting procedure, especially if the patient is pseudophakic. For these patients, we decide on 180° or 360° cutting depending on the amount of medications they are taking and severity of disease.
The ability to efficiently titrate the amount of viscodilation and cutting, as well as combine procedures with different mechanisms, is another example of how we can now tailor our procedures to the individual patient. This has been the most exciting aspect of the new interventional glaucoma mindset.
Conclusion
What new surgeons need to understand when faced with a myriad of decisions and situations is that there is no perfect procedure. Each surgeon needs to first identify their comfort level in performing the available procedure options. From there, the surgeon needs to identify the targeted outcomes, disease severity, angle anatomy, and postoperative course. These decisions will guide you through the decision tree of available options to reach the targeted endpoint.
IMPORTANT SAFETY INFORMATION
INDICATIONS FOR USE: The OMNI® Surgical System is a manually operated device for the delivery of small amounts of viscoelastic fluid, for example Healon or HealonGV* from Abbott Medical Optics (AMO), Amvisc* from Bausch & Lomb, or PROVISC* from Alcon, during ophthalmic surgery. It is also indicated to cut trabecular meshwork tissue during trabeculotomy procedures.
DISCLAIMER: The OMNI® Surgical System is cleared (indicated) by FDA for the uses set forth above. While the OMNI® Surgical System is not specifically cleared for transluminal canal dilation, there is support for its use in transluminal canal dilation in the literature and medical textbooks, and ab interno trabeculotomy, for which it is FDA-cleared, is referred to as a MIGS procedure in the literature and medical textbooks and dictionaries. A current list of references/publications is available through Sight Sciences, Inc.
*Trademarks are property of their respective owners.
For important safety information including contraindications, warnings, precautions and adverse events, please visit omnisurgical.com.
© 2020 Sight Sciences, Inc. 5/20 OM-1009-US.v1