In April 2024, millions of people witnessed the Great North American Solar Eclipse. In addition to offering a stunning visual experience in some parts of the country, the event prompted a surge in public inquiries about eye health and solar retinopathy. This ophthalmic condition can lead to photochemical toxicity of the fovea, visual acuity loss, and paracentral scotomas.1-3 Solar retinopathy is a rare condition, but the number of cases typically increases following a solar eclipse4,5 (see Clinical Findings and Management of Solar Retinopathy).
AT A GLANCE
- The Great North American Solar Eclipse elicited a wave of online searches related to potential eye damage.
- The increase in online searches for terms associated with eye damage and symptoms of solar retinopathy suggests a shortfall in educational outreach before the eclipse.
- Through infodemiology (ie, the study of the distribution and determinants of information on the internet), physicians may be better able to understand population-level behavior in real time and anticipate the need for preventative health policies and educational campaigns for future global events.
Clinical Findings and Management of Solar Retinopathy
Solar retinopathy presents as photochemical toxicity of the fovea, with damage to the interface between photoreceptors and the retinal pigment epithelium.1 This central foveal damage can be perceived on macular examination (Figure A). Central pigment clumping surrounding atrophy may be observable with fluorescein angiography (Figure B). OCT findings show mostly discreet areas of well-demarcated subfoveal loss of the hyperreflective layer of photoreceptors (Figures C and D).
Patients experience visual acuity loss, metamorphopsias, and central as well as paracentral scotomas.2-4 Their symptoms can resolve over time, with most of the improvement taking place 1 to 6 months after the initial photic injury. Some individuals, however, experience irreversible vision damage.

Figure. Examples of the diagnostic findings of solar retinopathy. Fundus photograph showing central foveal changes with increased hyperreflectivity (A). Fundus angiography showing central staining of pigment clumping with surrounding atrophy (B). OCT scan showing focal discontinuity of the inner and outer segment junction and underlying retinal pigment epithelium (C and D). These images were originally published in the Retina Image Bank website. A and C: Author Theodore Leng, MD, MS. Photographer N/A. Title: Solar Retinopathy. Retina Image Bank. 2013; Image Number 5041 & 5043. © the American Society of Retina Specialists. B and D: Author Thomas A. Ciulla, MD, MBA. Photographer Thomas Steele. Title: Solar Maculopathy. Retina Image Bank. 2015; Image Number 24826 & 24830. © the American Society of Retina Specialists.
There is no known beneficial treatment for solar retinopathy. Primary prevention is therefore the best form of therapy, and public education about safe eclipse viewing is of the utmost importance.
1. Stock RA, Savaris SL, de Lima Filho EC, Bonamigo EL. Solar retinopathy without abnormal exposure: case report. Arq Bras Oftalmol. 2013;76(2):118-120.
2. Dhir SP, Gupta A, Jain IS. Eclipse retinopathy. Br J Ophthalmol. 1981;65(1):42-45.
3. Michaelides M, Rajendram R, Marshall J, Keightley S. Eclipse retinopathy. Eye (Lond). 2001;15(pt 2):148-151.
4. Bruè C, Mariotti C, De Franco E, Fisher Y, Guidotti JM, Giovannini A. Solar retinopathy: a multimodal analysis. Case Rep Ophthalmol Med. 2013;2013:906920.
As a widely viewed event, the recent solar eclipse presented a unique opportunity to analyze the extent and nature of public concerns through an infodemiology approach. This article shares our findings and their implications for public health.
UNDERSTANDING PUBLIC HEALTH CONCERNS THROUGH ONLINE SEARCHES
Infodemiology
The term infodemiology, meaning information epidemiology, refers to the study of the distribution and determinants of information on the internet. Data such as search queries and social media posts are used to predict disease outbreaks and understand health behaviors.
Search Term Popularity
The Great North American Solar Eclipse elicited a wave of online searches related to potential eye damage. We extracted data from Google Trends (trends.google.com) to determine the temporal and geographic distribution of public interest in topics related to photic injury from unsafe eclipse viewing across the United States. We analyzed the search volume index (SVI) for terms directly related to eye injuries from the eclipse based on patient education materials; examples include eye damage, solar retinopathy, and eclipse blindness.6
Google Trends quantifies interest by a keyword SVI ranging from 0 to 100, with 100s being peak popularity during the specified time range. We found that the terms reached their peak popularity in the hours immediately following the eclipse (Figure 1) and were used the most in states located within the path of totality (P < .01 for all search terms after independent samples t-test, Figure 2).

Figure 1. Google Trends SVI output of keywords versus time. All values were normalized to the search term with the highest SVI (eye damage).
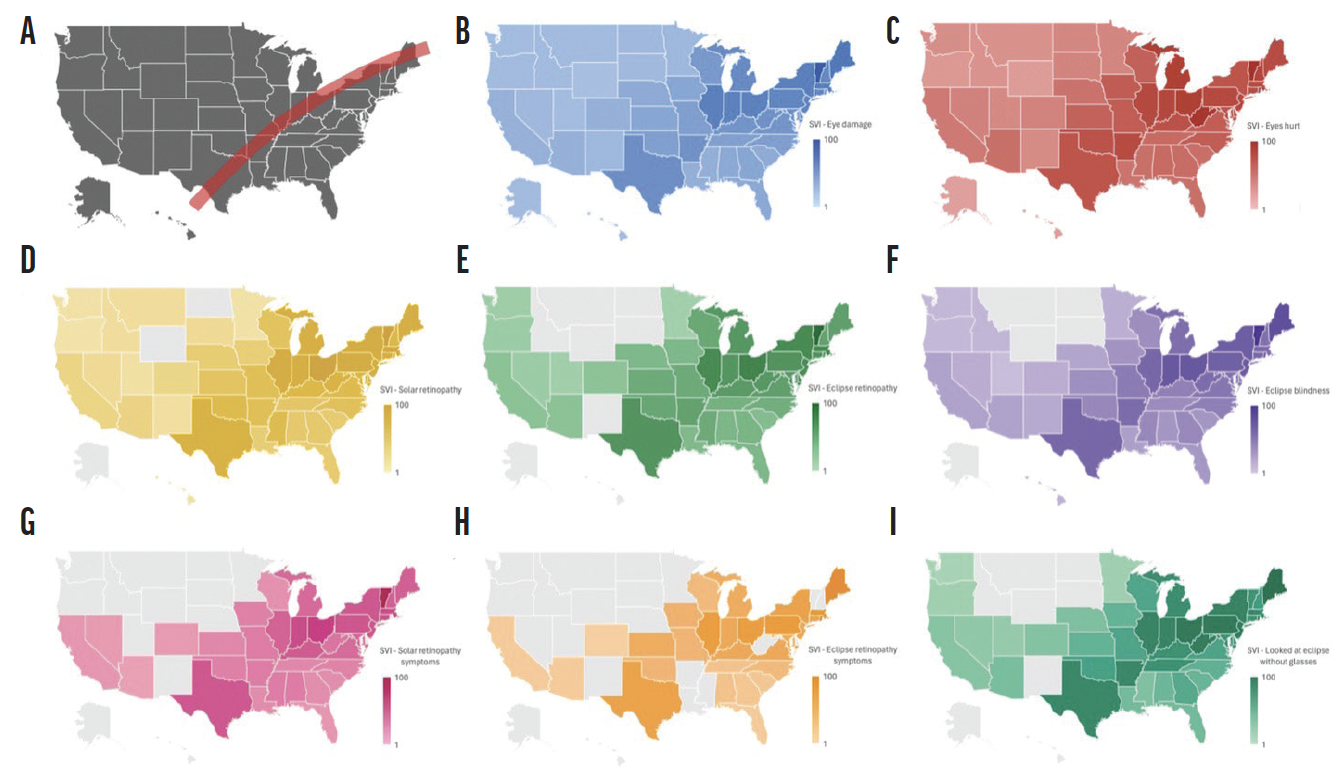
Figure 2. Geographic heat maps of SVI for keywords by state. Solar eclipse path of totality (A). Geographic heat map of search terms: eye damage (B); eye hurts (C); solar retinopathy (D); eclipse retinopathy (E); eclipse blindness (F); solar retinopathy symptoms (G); eclipse retinopathy symptoms (H); and looked at eclipse without glasses (I). States shaded in gray indicate that insufficient online searches were accrued to be documented within the Google Trends database.
Health Literacy
We used a health literacy data map to assess the geographic distribution of public inquiries and their correlation with regional health literacy rates.7 We then used a machine learning algorithm from the scikit-learn library (version 1.0.2) to generate k-means clusters of higher and lower levels of health literacy, with independent samples t-tests performed to compare SVI between the two groups.8
We found that high volumes of searches occurred regardless of the states’ health literacy levels. Although health literacy can be a predictor of health behavior and outcomes, the Great North American Solar Eclipse triggered widespread interest and concern across individuals with various health literacy levels.
THE LIMITATIONS OF ONLINE SEARCH QUERY DATA
Our study had several limitations. First, the use of Google Trends data presented inherent challenges. SVI provided by Google Trends is a relative measure of interest, not absolute search volumes. These search data are also anonymous, limiting insights regarding demographic analysis.
Second, our analyses of eight key search terms might not have fully captured the range of queries people used to seek information about eye damage after eclipse viewing. This would have limited our understanding of public interest and concern.
Third, search queries alone cannot provide sufficient evidence for the true epidemiologic extent of photic injury. The number of searches might not have correlated with the prevalence of photic injury, and individuals with true photic injury symptoms might have foregone medical attention. The lack of direct clinical data on confirmed cases of solar retinopathy prevented a more comprehensive understanding of the true epidemiologic impact of the eclipse.
THE ROLE OF INFODEMIOLOGY
Despite its limitations, our study confirmed a significant surge in public concern regarding eye health and solar retinopathy following the Great North American Eclipse of 2024. The marked increase in searches for terms associated with eye damage and symptoms of solar retinopathy underscores a possible shortfall in educational outreach before the eclipse.
In an increasingly digital world, infodemiology could help ophthalmologists learn more about patients, whether it be public concern about photic injury after an eclipse, perception of a specific procedure or technology, or disease awareness. By leveraging data-driven approaches such as search engine queries, physicians can better understand population-level behavior in real time and anticipate the need for preventative health policies and educational campaigns for future global events. The next total solar eclipse will span Europe in 2026; the next eclipse crossing the continental United States will occur in 2044.
1. Dhir SP, Gupta A, Jain IS. Eclipse retinopathy. Br J Ophthalmol. 1981;65(1):42-45.
2. Michaelides M, Rajendram R, Marshall J, Keightley S. Eclipse retinopathy. Eye (Lond). 2001;15(pt 2):148-151.
3. Bruè C, Mariotti C, De Franco E, Fisher Y, Guidotti JM, Giovannini A. Solar retinopathy: a multimodal analysis. Case Rep Ophthalmol Med. 2013;2013:906920.
4. Codenotti M, Patelli F, Brancato R. OCT findings in patients with retinopathy after watching a solar eclipse. Ophthalmologica. 2002;216(6):463-466.
5. Wong SC, Eke T, Ziakas NG. Eclipse burns: a prospective study of solar retinopathy following the 1999 solar eclipse. Lancet. 2001;357(9251):199-200.
6. Solar retinopathy. Cleveland Clinic. Accessed April 12, 2024. https://my.clevelandclinic.org/health/diseases/solar-retinopathy
7. Health literacy data map. The University of North Carolina at Chapel Hill. Accessed April 13, 2024. http://healthliteracymap.unc.edu
8. Ikotun AM, Ezugwu AE, Abualigah L, Abuhaija B, Heming J. K-means clustering algorithms: a comprehensive review, variants analysis, and advances in the era of big data. Information Sciences. 2023;622:178-210.