CASE PRESENTATION
A 40-year-old man is referred for a cataract evaluation. In the exam lane, the tall, thin patient is seen wringing his hands and bouncing his feet on the chair. He reports a progressive reduction in vision, glare, halos, and changes in his glasses prescription. He can no longer function normally and says he knows that surgery is necessary but that he has been dreading this day for 10 years.
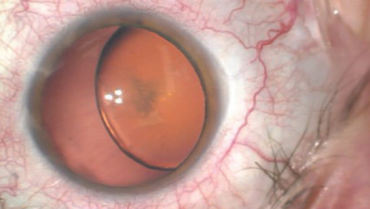
On examination, the patient’s BCVA is 20/70 OU, which improves to 20/30 with pinhole testing. A note attached to the computer in the exam room by a technician reads, “IOP not checked due to anxiety. MD to do.” When a slit-lamp exam and IOP check are subsequently attempted, the patient quickly withdraws from the slit lamp and says, “Sorry, I’m very nervous.” An effort is made to calm him, and an examination is conducted, revealing a well-dilated pupil and a significantly subluxated crystalline lens in each eye (Figure 1). The posterior segment of each eye appears to be healthy with no retinal tears or posterior vitreous detachment (PVD). Biometry and tomography measurements are shown in Figures 2 and 3.

Figure 1. Stretching of the nasal zonules in the left eye is relatively severe, allowing superotemporal subluxation of the crystalline lens. Significant nuclear sclerotic changes to the lens itself are also apparent.
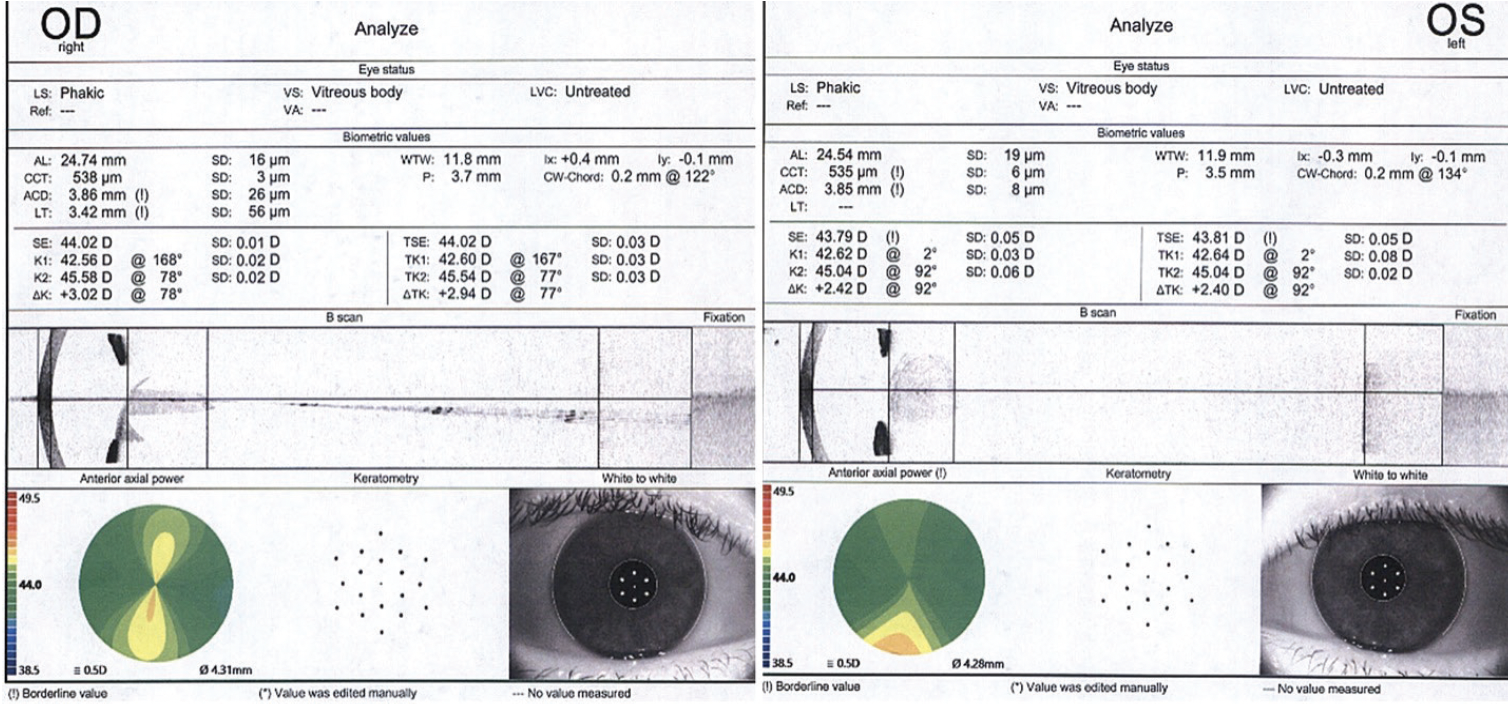
Figure 2. Measurements of the right and left eyes with the IOLMaster 700 (Carl Zeiss Meditec). OCT imaging shows subluxation of the lenses and good fixation. Keratometry reveals moderate with-the-rule (WTR) astigmatism.

Figure 3. Measurements of the right and left eyes with the Pentacam (Oculus Optikgeräte) show WTR astigmatism but otherwise normal tomography.
How would you proceed? Would the patient’s anxiety influence your management strategy?
— Case prepared by Brandon D. Ayres, MD

JOSEPH G. CHRISTENBURY, MD
The patient has a connective tissue disorder, likely Marfan syndrome but possibly Ehlers-Danlos syndrome. He has significantly subluxated native crystalline lenses from zonular insufficiency, a result of the connective tissue disorder. I think cataract surgery is warranted at this stage.
Although the exam found no retinal tears or PVD, I would refer the patient to a retina surgeon for a thorough examination with scleral depression to confirm the absence of peripheral retinal pathology. The cataract procedure may be challenging due to the severe zonulopathy, so the patient may need to see the retina specialist during the postoperative period.
I would plan to perform cataract surgery under general anesthesia owing to the patient’s severe anxiety. Given the biometry and topography measurements, I would choose a monofocal toric IOL targeted for distance to correct his astigmatism and counsel him that he will require reading glasses postoperatively.
After the capsulorhexis, capsular hooks would be placed to pull the lens centrally and stabilize the capsular bag. Hydrodissection and hydrodelineation would be performed to isolate the lens nucleus. After the nucleus has been removed, a capsular tension ring (CTR) and a Morcher Ahmed Segment (FCI Ophthalmics) would be inserted to fixate the capsular bag to the sclera before cortical removal. A temporal peritomy would be made, and the Ahmed Segment would be secured to the temporal sclera with an 8-0 PTFE suture (Gore-Tex, W.L. Gore & Associates). Provided all has gone well to this point, a toric IOL would be implanted in the bag. Triamcinolone acetonide (Kenalog, Bristol-Myers Squibb) would then be injected into the anterior chamber to ensure no vitreous prolapse is present.

NICOLE FRAM, MD
The patient has ectopia lentis and physical characteristics consistent with Marfan syndrome. Characteristic findings with this condition include a tall, lean body habitus, a disproportionate arm-to-height ratio, arachnodactyly due to relatively long fingers and toes, and a high, arched palate.1 Bilateral superotemporal lens displacement, as shown in Figure 1, is common among patients with Marfan syndrome.2 Before surgical intervention is considered, the cardiovascular risk factors of aortic root dissection, aortic aneurysm, and/or mitral valve abnormality should be evaluated and ruled out.3
In addition to the obvious challenge presented by the zonulopathy due to the fibrillin-1 gene mutation located on chromosome 15, the patient has significant anxiety. Surgery under general anesthesia is often preferred for young, anxious men, but the patient may have comorbid conditions that will disallow it. At a minimum, a retrobulbar or sub-Tenon block would be performed, and verbal anesthesia would be employed.
Biometry and corneal tomography reveal significant WTR astigmatism. Plan A could involve the placement of a sutured CTR or a CTR with a sutured Ahmed Segment in the bag and the implantation of a toric IOL, also in the bag. If neither of these strategies is feasible owing to severe zonulopathy, then the scleral fixation of an enVista Toric IOL (model MX60T, Bausch + Lomb) with a PTFE suture (off-label indication) would be an excellent plan B (Figures 4 and 5).
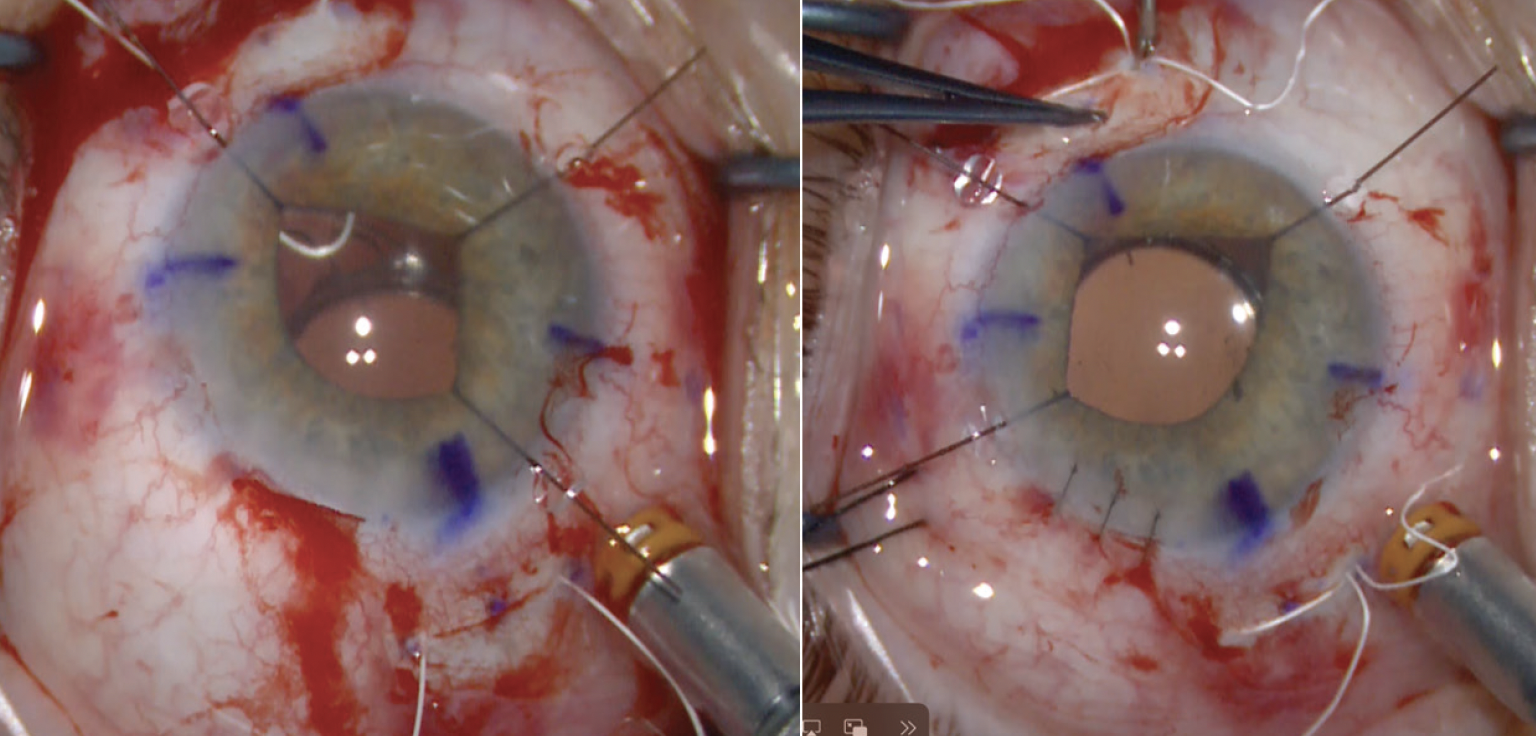
Figure 4. An MX60ET lens is horizontally fixated to the sclera with a PTFE suture. Note: The suture knot and ends should be fully buried in the sclerotomy.

Figure 5. An MX60ET lens is radially fixated with a flanged 7-0 polypropylene suture. Note: The flanges are buried in the sclera in a Z configuration.
Figures 4 and 5 courtesy of Nicole Fram, MD


BHARAT GURNANI, MBBS, DNB, FCRS, FICO, FAICO CORNEA, FAICO REFRACTIVE SURGERY, MRCSED, MNAMS, AND KIRANDEEP KAUR, MBBS, DNB, FPOS, FICO, FAICO PEDIATRIC OPHTHALMOLOGY, MRCSED, MNAMS
The significant superotemporal lens subluxation and the patient’s anxiety present a unique management challenge. Figure 1 hints at a differential diagnosis of Marfan syndrome. A decision to intervene surgically requires weighing its risk factors and associated complications against the patient’s BCVA. The possibility of aortic dissection/aneurysms makes the situation potentially life-threatening. The risk of retinal detachment due to associated myopia and retinal thinning and chance of dislocation of the crystalline lens could make the situation sight-threatening. Patients who have mild lens subluxation and BCVA better than 20/45 can be managed conservatively with spectacles or contact lenses. A lensectomy should be planned if the patient’s visual acuity is reduced by a greater amount of myopic astigmatism and gross lens subluxation. Vision correction with a scleral-fixated IOL, spectacles, or contact lenses can be planned. An important consideration is that, following lensectomy, the incidence of retinal detachment is lower if the patient is left aphakic.4
In the current situation, treatment must be approached with sensitivity and consideration for the patient’s mental well-being. It would be important to explain to the patient both the conservative and surgical options so he can make a well-informed decision. If surgery is pursued, his anxiety could influence its outcome, so we would recommend a consultation with a psychologist or psychiatrist before proceeding. An evaluation by a cardiologist to rule out cardiac associations would also be important.
The patient and his relatives would be counseled in detail on the importance of conservative management. Because his vision is correctable to 20/30, he could do very well with spectacles or contact lenses, and this would be our preferred approach.
If surgery is elected, the patient would be informed of the guarded visual prognosis. Our preference would be to perform surgery under sedation through an anterior route. Ideally, scleral fixation of the capsular bag through the eyelet of a CTR would be completed before any of the hydrosteps. A retina surgeon would be on call in the event the nucleus drops and a pars plana vitrectomy (PPV) is required.

DETLEF HOLLAND, MD
The combination of a tall, thin, young patient with dislocated crystalline lenses is suggestive of Marfan syndrome, an autosomal dominant connective tissue disorder associated with cardiovascular, ocular, and skeletal abnormalities. Approximately 25% of individuals with Marfan syndrome have a spontaneous genetic mutation.
The occurrence of aortic aneurysms and heart failure, if not diagnosed and treated, often results in the death of patients with Marfan syndrome. It would therefore be important to inform this patient of the possible risks and refer him for cardiology and genetic examinations.
The crystalline lenses have dislocated severely owing to loose zonules. Because the patient’s visual acuity has decreased, the lenses may drop into the vitreous or dislocate into the anterior chamber with subsequent complications. Surgical treatment must be performed on the right eye, and the left eye requires frequent monitoring.
The capsulotomy is the most difficult step of cataract surgery in an eye with a dislocated crystalline lens. A capsulotomy exerts stress on the zonules, which may lead to intraoperative damage. For this reason, I transitioned in 2013 to a laser capsulotomy in eyes with dislocated lenses (Figures 6 and 7). The capsulotomy would be tailored to the patient’s ocular anatomy and centered on the lens apex. The capsular bag would be stabilized with iris hooks during phacoemulsification. If possible, scleral fixation of a CTR would be performed. Otherwise, iris or scleral fixation of the IOL with the Yamane technique5 would be performed.

Figure 6. Scheimpflug image of a dislocated lens obtained with the Lensar Laser System.

Figure 7. A laser capsulotomy performed in different eyes with subluxated lenses in patients who have Marfan syndrome.
Figures 6 and 7 courtesy of Detlef Holland, MD

WHAT I DID: BRANDON D. AYRES, MD
I performed as detailed an examination as possible and then had a long discussion with the patient that focused on how Marfan syndrome can complicate cataract surgery. I emphasized the importance of topical therapy and the possibility that sutures would have to be placed during surgery and removed several weeks later. In addition to describing the risks and benefits of surgery calmly and at length, I explained that, given the severity of the lens subluxation, a full PPV would likely be required for safety. The patient agreed to undergo surgery under general anesthesia on the left eye first. He was given a sample of artificial tears so that he could practice instilling eye drops and was referred to a retina specialist so that a combined procedure could be scheduled.
On the day of surgery, the patient received general anesthesia. Several paracentesis incisions were made, and the anterior chamber was filled with an OVD. Centration marks were placed at the limbus at the 3 and 9 clock positions with a gentian violet marker in the event that suture fixation of an IOL proved necessary. Conjunctival peritomies were created at these clock positions for the same reason.
A 4-mm near-clear temporal incision was started with a guarded diamond blade and extended into the cornea with a crescent blade. The anterior chamber was then entered with a 2.4-mm keratome. During the capsulorhexis, capsular support hooks were inserted to hold the crystalline lens in place (Figure 8). The nuclear portion of the lens and most of the cortical material were carefully removed via phacoemulsification. At this point, vitreous was observed to have broken through the zonules, and it became clear that zonular support was inadequate. A decision was made to perform a full vitrectomy and suture fixate the IOL for the patient’s safety.

Figure 8. Limbal marks highlight the 3 and 9 clock positions. A capsulorhexis is performed after the placement of a capsular support hook. Note the zonular laxity as the lens is pulled into position.
To facilitate the PPV, nasal and temporal peritomies were created, and marks for sclerotomies were made 3 mm posterior to the limbus and 4 mm apart. The marks were centered on the 3 and 9 clock positions (Figure 9). At the more superior of these locations, 23-gauge trocars were placed. The positions of the scleral incisions were selected for the comfort of the retina surgeon, who operated from the top of the patient’s head, and to allow IOL implantation from a temporal approach.

Figure 9. The nuclear portion of the lens is removed, and scleral incisions are made with 23-gauge instrumentation in preparation for a PPV and removal of the remaining lens and capsular bag. Although difficult to see here, vitreous is coming through the zonular apparatus, necessitating a vitrectomy.
The retina specialist then performed the PPV and removed the residual capsular bag. Once all vitreous had been cleared from the eye and a PVD had been created, the retina surgeon turned the case back over to me.
Two additional sclerotomies were created with a 23-gauge lancet in the locations previously marked on the sclera. A PTFE CV-8 suture was introduced into the anterior chamber with microforceps. A second pair of microforceps was then introduced through a nasal sclerotomy, and the suture was grasped in the anterior chamber and externalized with a handshake technique. The end of the suture protruding through the temporal wound was subsequently laced through an MX60E lens in a way that did not tilt the IOL (Figure 10). The suture was then externalized through the second nasal sclerotomy using a handshake technique. Next, a second strand of a PTFE suture was laced around the opposing haptic. The IOL was subsequently placed in the posterior segment, and the temporal sutures were externalized through the temporal scleral wounds. Again, care was taken to avoid torque on the IOL.
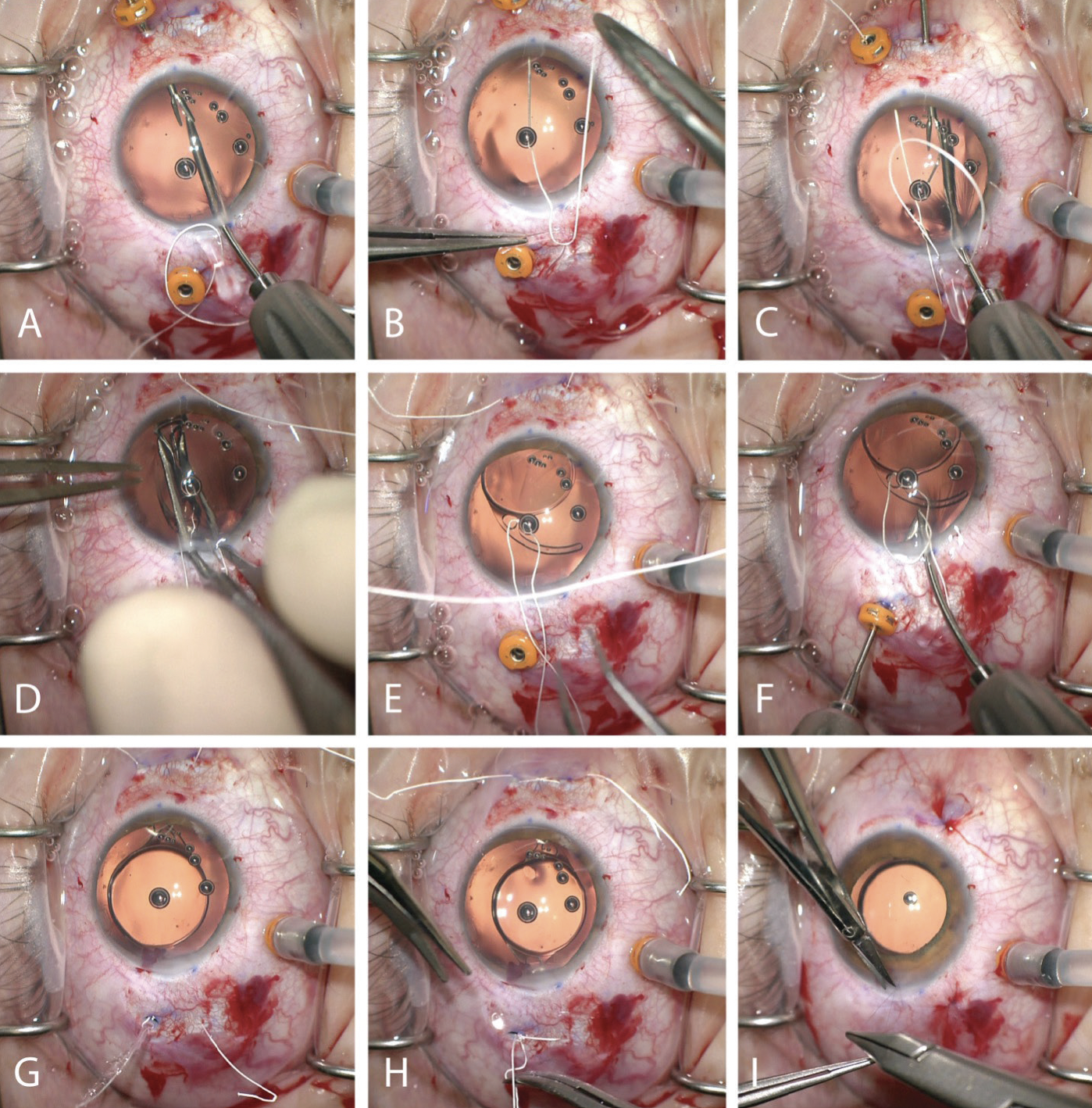
Figure 10. A sutured MX60E IOL (off-label uses of the suture and IOL). The first strand of the suture is passed through the main incision and withdrawn through the scleral incision using a handshake technique (A). The eyelet of the IOL is laced with a suture without placing torque on the IOL (B). The free end of the suture is externalized through the scleral wound to create a mattress suture (C). The opposing haptic is laced with a suture, and the IOL is folded and placed in the posterior segment (D). The trailing sutures are left prolapsing through the main incision. Care is taken to ensure they have not twisted and their orientation is correct (E). The trailing sutures are externalized through the scleral wounds (F and G) and carefully tied and buried (H). The scleral and conjunctival incisions are closed with a dissolvable (polyglactin) suture. The corneal wound is closed with a 10-0 polyglactin suture to avoid—owing to patient anxiety—the need for removal at the slit lamp postoperatively (I).
After the lens implant was in position, the trocars were removed. The PTFE suture was tied on the scleral surface. Care was taken to center the IOL without exerting too much stress on the haptics, which could have caused a fracture and dislocation. The suture knots were buried in the sclerotomy incisions, which were closed with a polyglactin suture. The peritomy was closed with the same polyglactin suture. Lastly, the infusion line that the retina surgeon had placed was removed, and the sclerotomy was closed with a polyglactin suture.
The IOL appeared to be well positioned, but a Seidel test of the temporal wound was negative. Moxifloxacin was injected into the anterior chamber, and the temporal wound was closed with a 10-0 polyglactin suture to avoid the need for its removal at the slit lamp. Before the patient was awakened, a retrobulbar block was administered, and a patch and eye shield were placed.
One day after surgery, the patch and shield were removed. The patient was so anxious that he refused to open his eye at the slit lamp. After receiving topical proparacaine and calming down, he allowed a limited examination to be performed, which found a well-formed globe and no sign of infection.
At the 1-week visit, the patient’s eye was much more comfortable, and his UCVA was 20/40 OS. At 1 month, his UCVA was 20/25 OS, and he was ready to schedule surgery on the second eye.
1. Judge DP, Dietz HC. Marfan's syndrome. Lancet. 2005;366(9501):1965-1976.
2. Rodrigo BJ, Paulina LL, Francesc Mde R, Eduardo TT, Alejandro N. Intraocular lens subluxation in Marfan syndrome. Open Ophthalmol J. 2014;8:48-50.
3. Brown OR, DeMots H, Kloster FE, Roberts A, Menashe VD, Beals RK. Aortic root dilatation and mitral valve prolapse in Marfan’s syndrome: an ECHOCARDIOgraphic study. Circulation. 1975;52(4):651-657.
4. Ariss MM, Qian Y, Singh R, Traboulsi EI. Management of lens subluxation in patients with Marfan syndrome: indications for cataract extraction. Invest Ophthalmol Vis Sci. 2009;50(13):5571.
5. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.