CASE PRESENTATION
A 67-year-old man is referred for an evaluation after experiencing a spontaneous IOL dislocation in the right eye. Cataract surgery with a three-piece monofocal IOL was performed on each eye 7 years ago. Three days ago, the patient noticed a change in the vision in his right eye. He saw neither flashes nor floaters.
Upon presentation, the patient says he has a congenital condition with bear tracks (ie, benign pigmented fundus lesions) that impair his peripheral vision. Based on an earlier retinal evaluation, he may have retinitis pigmentosa (RP).
On examination, the patient’s UCVA is 20/50 OD, and there is no improvement on refraction despite an autorefraction showing +5.75 +4.75 x 16º. His BCVA is 20/25+ OS. The IOP is 25 mm Hg OD and 22 mm Hg OS. The cup-to-disc ratio is 0.3 OU, and severe pallor of both optic nerves is evident (Figure 1). OCT scans of the macula show peripheral loss of outer segments. A slit-lamp examination is normal except for inferior subluxation of the IOL in the bag in the right eye (Figure 2).
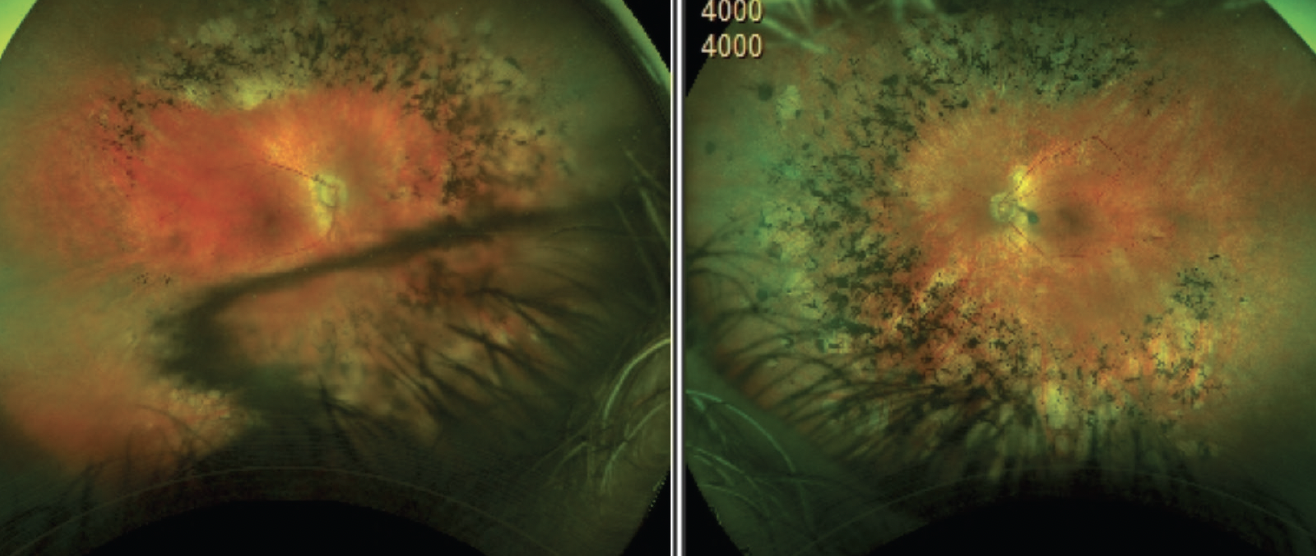
Figure 1. A fundus photograph shows bear tracks and bone spicules.

Figure 2. A spontaneously dislocated IOL.
How would you proceed?
— Case prepared by Cristos Ifantides, MD, MBA

CATHLEEN M. MCCABE, MD
IOL dislocation in the bag presents a management challenge, especially in the setting of dead bag syndrome with very little capsular fibrosis evident.1 I would begin the evaluation by determining if the patient was happy with his vision before the dislocation, in which case I might refixate the IOL. The preoperative evaluation would include an assessment of his BCVA to set expectations, the status of the zonules (generalized or localized weakness), the degree of capsular fibrosis, the type of lens implant and its haptic design, and the health of the cornea. Any ocular comorbidities would be noted. OCT scans of the macula and optic nerve would also be obtained.
The optic nerve pallor, bilateral retinal bone spicule changes, and zonulopathy in this case are common features of RP. I often observe capsular contraction and phimosis in these patients as well and place a capsular tension ring at the time of cataract surgery, especially when the individual is relatively young. Posterior capsular cataracts are common in this population. I would inform the patient that his visual prognosis is guarded because of his 20/50 BCVA OD and the progressive nature of RP.
At the start of surgery, a 23-gauge trocar would be placed 3.5 mm posterior to the limbus inferotemporally, and an anterior chamber maintainer would be inserted through a paracentesis at the limbus. I often create a belt loop with a 6-0 polypropylene suture and use a flanged technique for the scleral fixation of in-the-bag dislocated IOLs. Figure 2, however, appears to demonstrate dead bag syndrome with limited fibrosis of the capsular bag containing a three-piece IOL. If this impression proves correct, the haptic may slide through a suture loop over time.
After performing a limited anterior vitrectomy and clearing away the capsule, I would inspect the lens. If the IOL is undamaged, one of the following fixation techniques would be executed:
- The haptics would be externalized through the sclera and conjunctiva, and a flange would be created with low-temperature cautery (Yamane technique2);
- The haptics would be externalized under a scleral flap and buried in scleral tunnels (glued IOL technique3); or
- The haptics would be sutured to the iris (double needle technique4; see below for a demonstration).
If damage to the IOL is observed, it would be exchanged for either an Akreos (model AO60, Bausch + Lomb)5 or enVista (Bausch + Lomb). The new lens would be fixated to the sclera with a PTFE suture (Gore-Tex, W.L. Gore & Associates; off-label use) or using a flanged technique with a polypropylene suture.
Postoperatively, the patient would be advised not to rub his eyes, which would increase the risk of future IOL dislocation or flange erosion.

ERIK NAVAS-VILLAR, MD
The prevalence of IOL subluxation is increasing, which can be attributed in part to a growing volume of patients undergoing refractive lens exchange (ie, at a relatively younger age than for typical cataract surgery) and an increase in the number of patients with diseases such as diabetes that can cause early cataract formation. The management of a subluxated IOL is relatively straightforward in an otherwise healthy individual. RP, however, increases the risk of postoperative complications such as cystoid macular edema.
A thoughtful approach with two primary considerations is required. The first is whether the refractive and corneal astigmatism match. If the patient’s astigmatism is due entirely to IOL decentration/tilt, an IOL exchange is unnecessary.
The second consideration is how to avoid or minimize complications. Removing the entire IOL–capsular bag complex and performing scleral fixation of the IOL with or without a complete posterior vitrectomy could increase morbidity. Centering the bag with a lasso technique would therefore be my initial approach. Marks would be placed 180º apart in alignment with the haptics. A 1-mm–long vertical groove would be made toward the limbus to ensure that the suture is hidden in the sclera. A PTFE suture would be inserted at the 3-mm mark, passed under the haptic and through the IOL–capsular bag complex, retrieved with a 27-gauge hollow needle, and externalized. The same needle would then be inserted 2 mm from the limbus at the end of the initial groove to guide the suture, which would be passed over the haptic and externalized to create a loop. The procedure would be repeated with the other haptic to center the IOL.

WHAT I DID: CRISTOS IFANTIDES, MD, MBA
After leaning the patient backward and examining the lens, I could see clearly that the lens tilt was not significant. This step is important in situations like this one; otherwise, extreme posterior tilt or complete subluxation of the crystalline lens may not be detected until the day of surgery. Upon examination, no vitreous was visible anterior to the lens, either in the clinic or later in the OR.
I administer a retrobulbar block for any cases that require scleral work to minimize eye movement and prevent intraoperative and postoperative pain.
The IOL was still in the bag, which offered additional support for a sutured support system. Although the amount of fibrosis was less than in an eye with pseudoexfoliation, enough was present to prompt me to use a McCabe belt loop technique with a 6-0 polypropylene suture (Prolene, Ethicon).
Multiple paracenteses were created, and a 2.4-mm incision was made 180º away. A dispersive OVD was instilled in the eye. Marks were placed 2.5 mm posterior to the limbus and in the radial direction of where the sutured support system would provide the most support to the lens. A 6-0 polypropylene suture was threaded into the needle outside of the eye to ensure an adequate fit. The end of the suture was preplaced in the eye. A 30-gauge, thin-walled needle was introduced into the eye just posterior to the 2.5-mm mark and then passed under the IOL–capsular bag complex and through the capsule between the haptic and optic. The suture was threaded inside the needle and externalized with it. A small bulb was created. The process was repeated with the other suture end using a needle that was inserted just anterior to the 2.5-mm mark. The suture was then passed over the IOL–capsular bag complex (watch the surgery below).
The suture tension was adjusted until adequate IOL centration was achieved. The bulbs were buried in the sclera—an important step to prevent erosion. Next, a vitrectomy was performed to ensure vitreous remained posteriorly, and carbachol intraocular solution (Miostat, Alcon) and moxifloxacin were instilled in the eye.
The patient’s UCVA was 20/30 on postoperative day 1. It had improved to 20/25 at 1 month.
1. Culp C, Qu P, Jones J, et al. Clinical and histopathological findings in the dead bag syndrome. J Cataract Refract Surg. 2022;48(2):177-184.
2. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
3. Narang P, Agarwal A. Glued intrascleral haptic fixation of an intraocular lens. Indian J Ophthalmol. 2017;65(12):1370-1380.
4. Hart J Jr. Double needle iris/IOL fixation. VJCRGS. 2016;32(2). Accessed April 24, 2024. https://eyetube.net/series/vjcrgs-volume32-issue2/vj397
5. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528.




