Previsit Counseling Is Telling
Balamurali K. Ambati, MD, PhD, MBA, and Noraliz García-O’Farrill, MD
Eugene, Oregon


Increasing maturity (ie, age) comes with reduced focusing adjustment (ie, accommodation). In patients with cataracts, the restoration of excellent visual function can be achieved through cataract extraction coupled with presbyopia technology.
PREFERENCES AND PROCESSES
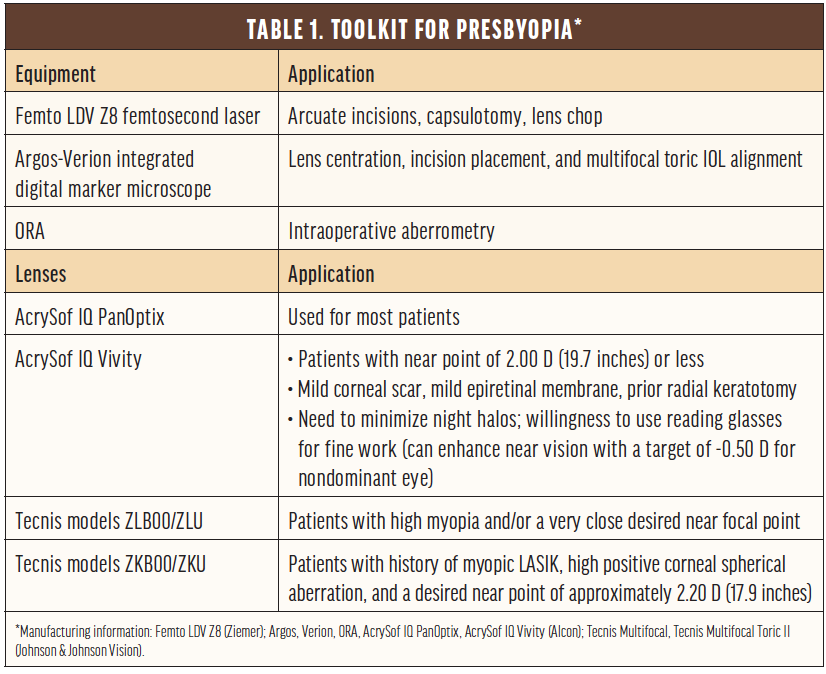
In the surgical suite. Table 1 shows our preferences for correcting presbyopia. Although most presbyopia-correcting IOLs can correct only 2.57 D of astigmatism, that is not an upper limit because lens technology can be combined with intrastromal corneal ring segments, laser arcuate incisions, and limbal relaxing incisions to allow presbyopia correction even in patients with 6.00 or 7.00 D of preoperative astigmatism. Short or long eyes may require a piggyback lens in addition to a presbyopia-correcting lens.
In the clinic. Equally important to what occurs in the OR is what happens before and after surgery. Previsit counseling using Surgiorithm’s system has increased the percentage of our patients who elect to undergo astigmatic and presbyopia correction at the time of cataract surgery from 43% to 53%. This system synergizes educational videos, a lifestyle questionnaire, and information on available options.
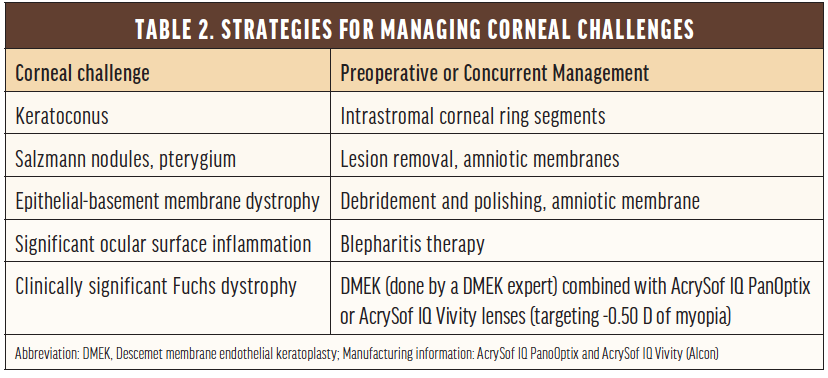
During the preoperative visit, patients learn that they may see rings after surgery because of lens-edge effects, will likely have dry eyes for a few months postoperatively, will likely need laser treatment for scar tissue behind the lens implant in 4 to 12 months after surgery, and may need a free touch-up for residual astigmatism or refractive error. Preoperative measurements are typically performed on at least two different occasions for patients who have a history of radial keratotomy to improve accuracy, and counseling addresses the lower precision of preoperative measurements in these eyes and the higher touch-up rate as a result. No matter the patient, it is essential to optimize the corneal surface before planning presbyopic cataract surgery (Table 2).
Younger patients without cataracts are offered refractive lens exchange (RLE), especially if they have high refractive errors, or monovision LASIK with a general target of -1.25 D sphere in the nondominant eye if they are not highly dependent on depth perception. In patients who have not tried monovision before, we first perform a contact lens trial.
Caution is required when treating patients in the zone of emmetropia or low myopia (0 to -3.00 D) because they have adapted well to their situation. Rocking the boat, so to speak, can be traumatic. These patients assume that they will retain their preexisting focal point and their quality and range of vision and that their visual function will increase. In reality, there are trade-offs. We ask patients specifically if they read without glasses and if they will be okay with a change in their near point.
CONCLUSION
In the future, patients with presbyopia but not cataracts and patients with low myopia may benefit from presbyopia-correcting eye drops. For now, however, we prefer the presbyopia-correction methods discussed herein.
An Overview of Past and Current Solutions
Francis Raymond Mendoza-Castor, MD, FPCS, FPAO
Calamba City, Philippines

I had relatively few options for correcting presbyopia when I started practice in 2007. Monofocals were the most commonly used lenses, and I opted for monovision strategies in select patients. My approach was conservative in patients with mild glaucoma or retinal pathology; I targeted emmetropia or mild myopia and prescribed spectacles. My approach has evolved with advances in lens technology.
THEN
Multifocal IOLs can decrease contrast sensitivity, which is a problem in patients whose vision has been compromised by glaucoma or retinal disease. For patients with glaucoma or retinal disease, my earliest choice of a presbyopia-correcting IOL was the Crystalens (Bausch + Lomb), which provided distance acuity comparable to that achieved with a monofocal IOL and better contrast sensitivity and uncorrected intermediate visual acuity than a multifocal IOL.1
Later, I transitioned to using the AT LISA 839 MP (Carl Zeiss Meditec) or the FineVision (PhysIOL) for patients with relatively uncompromised central visual fields and stable glaucoma.
NOW
Some of the latest presbyopia-correcting IOLs can improve near and intermediate visual acuity without reducing contrast sensitivity as much as earlier generations of these IOLs.
The Lentis Comfort LS-323 MF15 IOL (Teleon Surgical) has a low near add (+1.50 D) and acts like an extended depth of focus (EDOF) lens. This IOL is built on the company’s Mplus platform. I typically use the Düsseldorf strategy in normal eyes and in patients who have glaucoma or retinal disease. With this approach, emmetropia is targeted in either the dominant or better-seeing eye, and -0.50 D is targeted in the nondominant or worse-seeing eye to produce a mini-monovision effect.
For patients with full visual fields, I implant a Lentis Comfort lens in the dominant eye and either a Lentis Mplus MF20 or MF30 in the contralateral eye, depending on the patient’s visual needs. I have been using this strategy for most of my patients and have found that it enhances visual performance at both intermediate and near.
Compared with monofocal lenses, EDOF IOLs do not seem to affect visual field sensitivity. I have safely implanted EDOF IOLs in glaucoma patients with mild visual field loss not affecting the central 10º.
Takahashi et al2 compared the mean deviation (MD) in eyes implanted with bifocal, EDOF, and monofocal lenses. MD was -0.24 ±0.58 dB in the EDOF group, -1.38 ±0.58 dB in the bifocal group, and 36.6 ±1.4 dB in the monofocal group. In both MD and foveal threshold, there was a significant difference between the bifocal and the EDOF and monofocal groups (P < .001) but no difference between the EDOF and the monofocal groups. In my experience, EDOF IOLs afford a better quality of vision for my patients who have glaucoma without compromising visual field monitoring.
I have used the aforementioned strategy for patients with mild to moderate glaucoma, those with a stable epiretinal membrane, and those with stable diabetic macular edema.3 I seek to maximize the visual potential of the better-seeing eye and to improve functional near and intermediate visual acuity in the worse-seeing eye.
I look forward to using other EDOF lenses and accommodating lenses when they become available in the Philippines, where I practice.
1. Vilupuru S, Lin L, Pepose JS. Comparison of contrast sensitivity and through focus in small aperture inlay, accommodating intraocular lens or multifocal intraocular lens subjects. Am J. Ophthalmol. 2015;160:150-162.
2. Takahashi M, Yamashiro C, Yoshimoto T. Influence of extended depth of focus intraocular lenses on visual field sensitivity. PLoS One. 2020;15(9).
3. Grzybowski A, Kanclerz P, Tuuminen R. Multifocal intraocular lenses and retinal diseases. Graefes Arch Clin Exp Ophthalmol. 2020;258(4):805-813.
Current Technology Provides Excellent Results, Newer Treatments Are on the Horizon
Alaa Eldanasoury, MD, FRCS
Jeddah, Saudi Arabia

Rising life expectancy and a greater dependence on digital devices have increased patients’ demand for good functional vision at distance, intermediate, and near. My experience with laser treatments and IOLs for presbyopia correction has led me to recommend one of two options to most of my patients: excimer laser ablation using the Optimized Prolate Ablation (OPA; Nidek) algorithm1 or implantation of a FineVision IOL. I base my recommendation on the patient’s age, lens status, occupation, and lifestyle.
EXCIMER LASER ABLATION
The algorithm. The OPA ablation algorithm incorporates patient-specific ocular spherical aberration, corneal topography, and corneal curvature to maintain a prolate cornea over a scotopic pupil. This algorithm addresses induced spherical aberration, and it uses increased depth of focus from spherical aberration and a mini-monovision strategy to deliver excellent quality of vision and functional visual acuity at near, intermediate, and distance.
Study results. In a small study that my colleagues and I conducted (unpublished data), 15 patients underwent bilateral LASIK using the Navex Quest excimer laser system (Nidek) with OPA and a target of -0.30 µm of spherical aberration aimed at increasing the depth of focus for both eyes. The average age of patients was 48 years, and the average manifest refractive spherical equivalent was -4.29 ±1.83 D. Full correction was planned for the dominant (distance) eye and undercorrection of -0.50 D for the nondominant eye.
Three months after surgery, binocular uncorrected distance visual acuity was 20/20 or better in 92% of patients. Binocular uncorrected near visual acuity was J3 or better in all of the patients and J1 in 40%. No eye lost 2 or more lines of best-corrected distance visual acuity. Spherical aberration decreased by -0.26 µm, and the modulation transfer function decreased by 0.03 for the cohort.
Patient selection. In my experience, this ablation strategy is effective, predictable, and safe for the correction of presbyopia in young patients with myopia who have no or only mild nuclear sclerosis and retain some accommodative reserve (Figure 1).
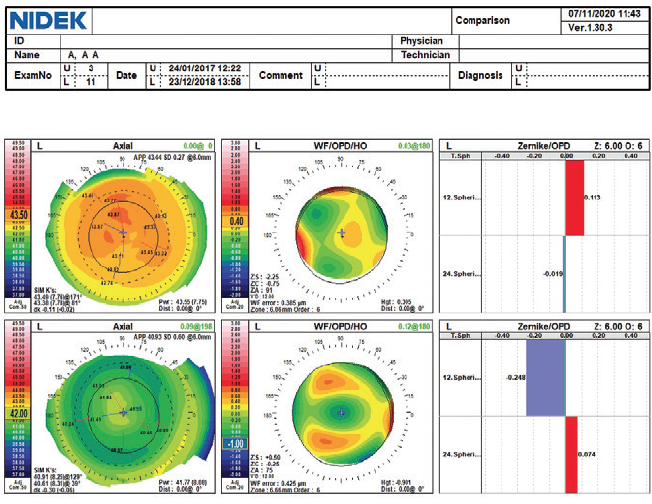
Figure 1. Examinations (top, preoperative; bottom, 2 years postoperative) of an eye that underwent LASIK using the Optimized Prolate Ablation profile. Axial maps (left) show a postoperative prolate cornea over the mesopic pupil entrance. Aberrometry (center) of the entire eye shows the induced negative spherical aberrations. Zernike graphs (right) show -0.25 µm of negative spherical aberration with a 6-mm pupil after surgery.
IOL IMPLANTATION
Study results. The FineVision diffractive trifocal IOL (Figure 2) is designed to address the drawbacks of bifocal IOLs and to enhance intermediate vision. In an unpublished study, my colleagues and I recently evaluated results in 38 patients who underwent bilateral implantation of spherical (model POD F) and toric (model POD FT) versions of this aspheric IOL. The mean age of patients was 54.7 ±9.2 years.
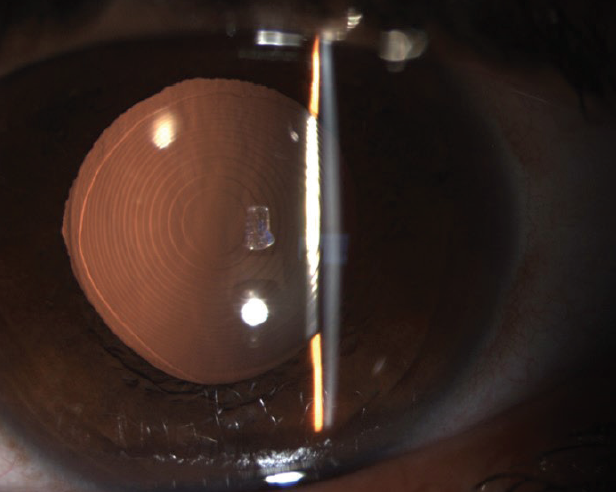
Figure 2. Model POD F of the FineVision IOL in situ. This hydrophilic acrylic, apodized, one-piece, foldable, diffractive, aspheric IOL has a multizonal design. The diffractive steps, placed on the anterior surface of the lens, divide incoming light to create two additional add powers (+1.75 and +3.50 D) at the IOL plane corresponding to 80- and 40-cm foci, respectively.
Patients achieved excellent functional vision and objective visual quality (Figure 3). The mean manifest refractive spherical equivalent decreased from -1.82 ±5.15 D preoperatively to -0.01 ±0.54 D at 6 months. Binocular UCVA was 0.1 logMAR or better at 4 m in 32 patients (94%), at 80 cm in 30 patients (83%), and at 40 cm in 28 patients (78%). Based on these results, we concluded that both IOL models provided excellent distance, intermediate, and near visual acuity.
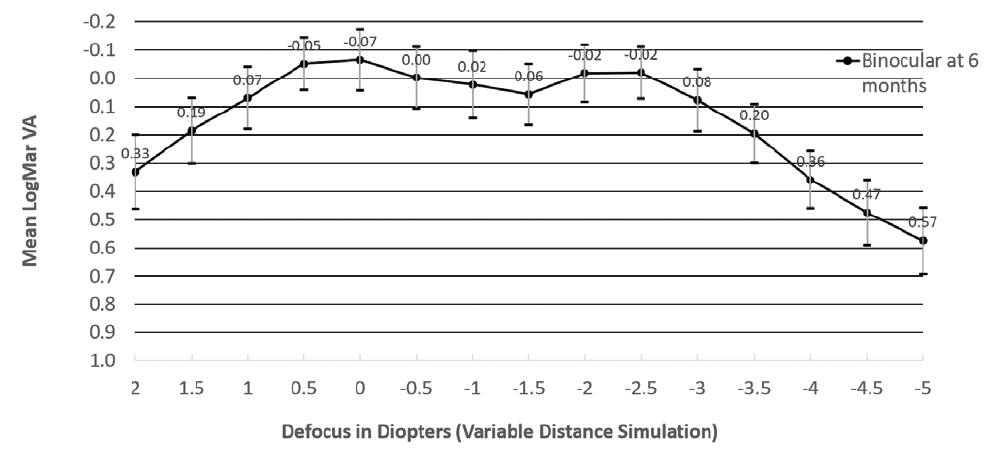
Figure 3. Binocular defocus curve for 36 patients 6 months after binocular implantation of a diffractive trifocal IOL (models POD F and POD FT of the FineVision IOL). The curve presents a visual acuity of -0.07 logMAR with defocus of 0.00 D, simulating distance vision, and -0.02 logMAR< with defocus of -2.00 and -2.50 D, simulating 50 and 40 cm, respectively. The intermediate logMAR visual acuity was 0, 0.02, and 0.06 with defocus of -0.50 D (2 m), -1.00 D< (1 m), and -1.50 D (67 cm), respectively.
Figures 1–3 courtesy of Alaa Eldanasoury, MD, FRCS
An informal patient survey indicated a high level of postoperative satisfaction. In general, patients reported that the benefits of spectacle independence for their daily activities outweighed the drawback of a slight reduction in vision quality.
Patient selection. Trifocal IOL implantation and RLE are appropriate options for patients who have cataracts and for patients in whom laser vision correction and phakic IOL implantation are contraindicated.
CONCLUSION
The preoperative discussion of presbyopia correction with patients must address the inherent compromise of reduced optical quality and the potential for photic phenomena after surgery. It is important to ensure that patients have realistic expectations about the outcomes of presbyopia-correcting surgery.
In addition to the technologies I currently use, I look forward to introducing the latest version of the EVO Visian ICL (STAAR Surgical), the EVO Viva presbyopia-correcting lens. Early results in patients with -0.50 to -20.00 D of presbyopic myopia have been promising.
1. Eldanasoury A. NIDEK Optimized Prolate Ablation for the treatment of myopia with and without astigmatism. J Refract Surg. 2009;25(1):S136-S141.
Excited For What’s to Come
Erika N. Eskina, MD
Moscow, Russia

Each of the current options for the correction of presbyopia has advantages and disadvantages. Selecting an approach depends on the patient’s expectations, precise diagnostics, the surgeon’s knowledge of and experience with the technology and its underlying principles, and the accessibility of postoperative support for the patient. I favor two strategies for correcting presbyopia, but I am excited about a third on the horizon.
LASER ABLATION
Sphere Eye Clinic is a reference center for Schwind and Carl Zeiss Meditec. My colleagues and I therefore have been working predominantly with the Schwind CAM PresbyMax module (Schwind eye-tech-solutions), which creates a multifocal cornea, induces slight anisometropia, and extends depth of focus by increasing spherical aberration in the cornea.1 Postoperatively, neural adaptation can take up to 4 weeks. During this period, patients may experience some blurring and a decrease in distance visual acuity.
Postsurgical observation of my patients now extends beyond 5 years, and treatment has remained effective for that time.2 Theoretically, the effect of treatment could be preserved after the development of a cataract because of the stability of the corneal profile.
I recommend this form of presbyopia correction to patients whose crystalline lenses are clear, who:
- Retain some accommodative amplitude;
- Have a strong desire for spectacle independence; and
- Prioritize comfort and a long-lasting effect but are not ready to undergo intraocular surgery.
The software is designed to allow reversal of the procedure, but fortunately, we have yet to test reversibility.
MULTIFOCAL AND EDOF IOLS
The second strategy I use is RLE. Because this option is permanent, it is essential to ensure that it will satisfy the patient’s expectations and visual needs both at present and in the future. It is also important to consider any concomitant diseases and their potential impact on visual function.
Generally, the decision in our practice is mostly between bifocal and trifocal IOLs, but we also implant EDOF lenses. Candidate selection takes into account a patient’s need to drive at night, level of perfectionism, corneal spherical aberration and ability to tolerate a period of neural adaptation, and unwanted visual phenomena.
It is important for surgeons to understand the specifics of each lens design, including light distribution, main points of focus, and optics. We consider these parameters in conjunction with the size and mobility of patients’ pupils and their visual requirements.
THE HORIZON
An ideal solution to presbyopia does not currently exist. I am excited, however, about pharmaceutical agents (ie, presbyopia-correcting eye drops) in development for the treatment of this condition.
1. Eskina EN, Manjago T, Shkurenko IV, Rybakov PO, Parshina VA, Stepanova MA. Experience of PRESBY LASIK operations on excimer laser system SCHWIND AMARIS. Prakticheskaja Medicina. 2012;1-4(59):55-58.
2. Pajic B, Massa H, Eskina EN. Presbyopiekorrektur mittels laserchirurgie. Klin Monbl Augenheilkd. 2017;234(9):e29-e42.
The Demand for Presbyopia Correction Is Growing
Erik L. Mertens, MD, FEBOphth
Antwerp, Belgium

The demand for presbyopia-correcting procedures increases year over year, and the surgical options keep expanding as a result. When the gradual loss of vision interferes with simple everyday tasks, including reading, looking at a smartphone or tablet, and working on a computer, many patients find that it is time to seek a more permanent and convenient solution than reading glasses. This is especially true today, when wearing a face mask in public aggravates the drawbacks associated with wearing glasses.
Before counseling patients on their options, I evaluate them for presbyopia with a simple eye exam. I then explain to them that there are a lot of possible solutions available to help them. I note that multifocal eyeglasses and multifocal or monovision contact lenses are simple options for presbyopia correction and discuss with them the aesthetic concerns and nuisances. Monovision contact lenses can be problematic for those who have a difficult time with neural adaptation because visual acuity and depth perception can be affected.
PREFERENCES
When patients express interest in the surgical correction of presbyopia, I recommend the solution that I think is best suited for them. I do not have a preference for one procedure over another in general, but I recognize that all procedures involve a compromise.
Cornea-based procedures. Monovision laser treatments such as PRK, LASIK, SMILE, and SmartSight (Schwind eye-tech-solutions) correct the dominant eye for distance vision and leave the nondominant eye nearsighted. The problems with this approach are that depth perception may be affected and distance vision often is not as crisp as it could be. Careful preoperative selection is therefore crucial.
Presbyopic LASIK (presby-LASIK) procedures increase the magnitude of negative or positive spherical aberration in order to provide the eye with some multifocality. The same careful patient selection as with monovision is required with this technique.
The implantation of corneal inlays is another option. However, these implants require precise centration during surgery, and they may decrease the patient’s distance vision and increase the risk of corneal haze, blurred vision, starbursts, and refractive regression. For these reasons, I no longer offer corneal inlays. Allograft inlays recently became available, and early reports suggest that they are well tolerated.1 As with corneal inlays, a precise implantation technique is required. (Editor’s note: Allograft inlays will be covered in more detail in CRST’s February issue.)
Lens-based procedures. Posterior chamber phakic IOLs can be used to correct presbyopia. Patients typically experience a fast visual recovery and good refractive stability. Further, the lenses can be removed when patients are not satisfied with the result. Some available options include the Implantable Phakic Contact Lens (IPCL, Care Group), which has a diffractive optical zone of 5.8 mm and is available with near additions between +1.50 and 4.00 D, and the EVO Viva ICL (STAAR Surgical), an EDOF posterior chamber phakic lens that uses higher-order aberrations to smooth out the dips in the defocus curve. Early clinical results are encouraging.2
RLE may be performed when corneal laser surgery is not possible or cannot achieve the desired refractive outcome.3 In some clinics, RLE is a controversial practice because the risk of endophthalmitis can be more devastating than corneal infections after keratorefractive surgery. Moreover, RLE may carry a higher risk of complications such as retinal detachment than conventional cataract surgery, especially in younger patients and those with high myopia.
Over the years, I have used many different presbyopia-correcting IOLs, including bifocal, trifocal, EDOF, accommodating, hybrid, and rotationally asymmetric models. In the end, I always come back to trifocal IOLs. In my hands, these lenses deliver the highest rate of patient satisfaction.
CONCLUSION
The best solution for presbyopia correction depends on the patient’s age, lifestyle, status of distance vision, and personal preferences.
1. Cummings AB. Allograft lenticules for the treatment of presbyopia. Cataract & Refractive Surgery Today. 2019;6:76-80.
2. Packer M, Alfonso JF, Aramberri J, Elies D, Fernandez J, Mertens E. Performance and safety of the extended depth of focus implantable collamer lens (EDOF ICL) in phakic subjects with presbyopia. Clin Ophthalmol. 2020;14:2717-2730.
3. Ang M, Gatinel D, Reinstein DZ, Mertens E, Alió Del Barrio JL, Alió JL. Refractive surgery beyond 2020. Eye (Lond). July 24, 2020. doi:10.1038/s41433-020-1096-5
Preferred Strategies in Mexico and a Personal Experience With RLE
Francisco Sánchez Leon, MD, and Rocío Sanchez Sanoja, MD
Ciudad de México


More than 25 million people live in Mexico City, and the metropolitan area is considered the most competitive place in the country in terms of practicing ophthalmology. Including us, there are close to 1,500 board-certified, registered ophthalmologists practicing in Mexico City but only a few colleagues with training in the latest corneal laser and phaco techniques to correct presbyopia. A variety of presbyopia-correction techniques used in our country are described herein.
One of us (F.S.L.) was involved in the development of various corneal inlays, including the Kamra (Figure 4; AcuFocus), and their implantation techniques. Although corneal inlays recently fell out of favor, they may become popular again if surgeons can learn to control the reproducibility of femtosecond laser corneal dissection and to avoid scarring and the light scatter it causes.
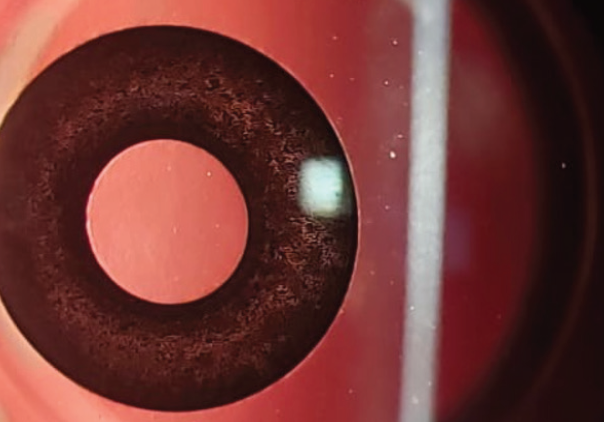
Figure 4. The Kamra corneal inlay in situ.
Corneal procedures such as Intracor (Bausch + Lomb) have also been used to treat presbyopia with some success, but until femtosecond lasers incorporate both a visual axis eye tracker and a corneal remodeling lock, like the lasers used for CXL, these procedures will not enjoy widespread popularity. Among the corneal laser-based surgical options for presbyopia correction, monovision-planned excimer laser surgery is therefore still the most common strategy used by refractive surgeons in Mexico. Very few clinics have the MEL 80 or 90 excimer laser platforms (Carl Zeiss Meditec), so the adoption of the company’s Presbyond Laser Blended Vision procedure is low. Even refractive fellows within the country who have access to one of the company’s excimer lasers are not convinced that this innovative corneal laser procedure is effective. In Latin America, the biggest reason for the low adoption of Presbyond and other laser blended vision techniques is economic.
LENS-BASED CORRECTION PREFERRED
The most popular approach to correcting presbyopia in Mexico is lens-based. Premium IOLs, including multifocals, have been used for the past decade for both cataract surgery and RLE. The latter is mainly performed on patients who are at least 50 years of age.
Popular premium IOLs in Mexico—and our preference—include the trifocal IOLs manufactured by PhysIOL. With the introduction of the company’s Triumf and IsoPure, this family of lenses represents a complete portfolio of options, including hydrophilic, hydrophobic, EDOF, and toric lenses. We also use the AT LISA, which is available in bifocal and trifocal designs. This IOL platform is a good option when a patient needs a lens with an extremely low power or requires between 6.00 and 12.00 D of astigmatism correction. We are also excited about the Tecnis Eyhance and Tecnis Synergy IOLs (both from Johnson & Johnson Vision), which should be available in early 2021. We also use the AcrySof IQ PanOptix (Alcon), Liberty (Medicontour), and SeeLens MF (Hanita).
PRACTICE WHAT YOU PREACH
After seeing the positive results achieved by my patients, I (F.S.L.) recently chose RLE for myself. My friend and colleague Ricardo Acosta, MD, performed my surgery at the Puerta de Hierro Hospital in Guadalajara (Figures 5 and 6) in November 2020.*

Figure 5. Dr. Sánchez Leon undergoes RLE at Puerta de Hierro Hospital (A–C).
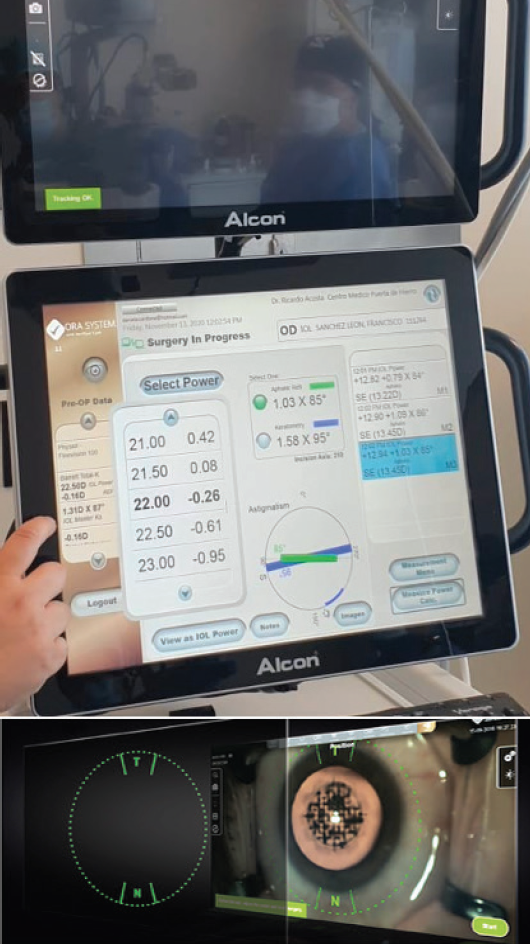
Figure 6. Dr. Acosta and his team perform laser cataract surgery on Dr. Sánchez Leon with intraoperative aberrometry assistance to decide the magnitude and axial alignment of the chosen IOL.
A FineVision Tri Toric POD F IOL was implanted bilaterally. This apodized, hydrophilic, diffractive IOL has a double C-loop haptic design and 5º of angulation for excellent centration and stability. I chose a hydrophilic IOL because it delivers fewer chromatic longitudinal aberrations compared to hydrophobic materials.1-3 The lens features UV filtration and a blue-light blocker. The optic body diameter is 6 mm, and the overall diameter is 11.4 mm. In addition to its far refractive power, the FineVision POD F provides two foci for intermediate and near visual acuity, with addition powers of 1.75 and 3.50 D, respectively.4
Combining laser cataract surgery and intraoperative aberrometry has been shown to optimize the positioning of a toric IOL.5 With keratometric astigmatism of 1.50 D in my right eye and 1.25 D in my left, I thought that this procedure was the best choice for my eyes. It has also been shown that eyes undergoing cataract extraction and implantation of a toric IOL aided by intraoperative aberrometry are 2.4 times more likely to have less than 0.50 D of residual astigmatism compared to standard methods of astigmatism correction.6 However, this procedure is cost-prohibitive for many patients in Mexico, so most RLE and cataract surgery procedures here are performed with a manual technique.
RESULTS
I had good near and distance visual acuity on postoperative day 1, even when driving at night, and I had sharp visual acuity by postoperative day 7. In fact, 1 week after my RLE procedure, I performed 26 cataract surgeries at our Novavision Acapulco Clinic without a problem (Figure 7), and I noticed an increase in my 3D perception under the microscope.

Figure 7. One week after his RLE procedure, Dr. Sánchez Leon performs 26 cataract procedures in a single day.
Figures 4–7 courtesy of Francisco Sánchez Leon, MD
Nine days after surgery, I performed three penetrating keratoplasties, one deep anterior lamellar keratoplasty, and one Descemet stripping endothelial automated keratoplasty. At the time of this writing (2 weeks after surgery), my visual acuity is excellent. I have had a positive experience recovering my near vision, and I enjoy clinic and surgery again.
CONCLUSION
Lens-based presbyopia correction using a variety of premium IOLs is the most popular technique in Mexico. A manual RLE/cataract surgery procedure is preferred over laser cataract surgery with intraoperative aberrometry because of economic issues. Cornea-based presbyopia correction with monovision is also common in this country, whereas laser procedures such as Presbyond have low penetration rates. We are sure that many of our colleagues in Mexico will use presbyopia drops when they become available.
*Editor’s note: Dr. Sánchez Leon would like to share his deepest gratitude to Dr. Acosta and Lina Preciado, MD, both from Puerta de Hierro Hospital, for his near vision recovery and their professionalism and kindness.
1. Bozukova D, Pagnoulle C, Jérôme C. Biomechanical and optical properties of 2 new hydrophobic platforms for intraocular lenses. J Cataract Refract Surg. 2013;39(9):1404-1414.
2. Vinas M, Dorronsoro C, Garzón N, Poyales F, Marcos S. In vivo subjective and objective longitudinal chromatic aberration after bilateral implantation of the same design of hydrophobic and hydrophilic intraocular lenses. J Cataract Refract Surg. 2015;41(10):2115-2124.
3. Poyales F, Garzón N, Pizarro D, Cobreces S, Hernández A. Stability and visual outcomes yielded by three intraocular trifocal lenses with same optical zone design but differing material or toricity. Eur J Ophthalmol. 2019;29(4):417-425.
4. Loicq J, Willet N, Gatinel D. Topography and longitudinal chromatic aberration characterizations of refractive–diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2019;45(11):1650-1659.
5. Orts P, Piñero DP, Aguilar S, Tañá P. Efficacy of astigmatic correction after femtosecond laser-guided cataract surgery using intraoperative aberrometry in eyes with low-to-moderate levels of corneal astigmatism. Int Ophthalmol. 2020;40:1181-1189.
6. Hatch KM, Woodcock EC, Talamo JH. Intraocular lens power selection and positioning with and without intraoperative aberrometry. J Refract Surg. 2015;31(4):237-242.
Consider Long-Term, Evidence-Based Outcomes When Selecting a Procedure
Pooja Khamar, MD, PhD, FCRS; Sneha Gupta, MD; and Rohit Shetty, MD, PhD, FRCS
Bangalore, India



The most common modality for the treatment of presbyopia is spectacle correction.1 However, in the current era of refractive surgery, the surgical correction of presbyopia has gained traction. Presbyopia can be managed surgically either through dynamic approaches that use the eye’s residual accommodative power such as accommodating IOLs and scleral expansion devices or through static approaches that improve near vision by increasing depth of focus such as monovision LASIK, presby-LASIK, corneal inlays, conductive keratoplasty, Intracor, and lens-based surgery.
There is a plethora of options in lens-based presbyopia correction, including multifocal IOLs, monovision, and phakic multifocal IOLs—although this last option is more suitable for patients in their 40s.2,3 Variety exists in the cornea-based approach of presby-LASIK. Procedures in this category can be divided into three groups: central presby-LASIK, peripheral presby-LASIK, and laser blended vision.
PATIENT SELECTION AND WORKFLOW
Careful patient selection for the surgical correction of presbyopia is crucial.4-6 This requires a thorough preoperative workup that includes general considerations for presbyopia correction.
Dominant eye. It is important to identify the dominant eye, especially when planning a monovision-based procedure. For this, emmetropia is targeted in the dominant eye to provide good distance vision, and the nondominant eye is targeted for low myopia to aid near vision.
Tolerance test. Patients must be able to tolerate anisometropia, especially with monovision treatments.
Dry eye evaluation. Evaluating patients for dry eye disease (DED) is essential. Evaporative and aqueous deficient DED is increasingly prevalent in older age groups.7,8 Assessments for DED are mandatory before any presbyopia-correction surgery is planned. Further, tear film quality may be assessed quantitatively with the Optical Quality Analysis System (Visiometrics).
Pupil evaluation. Preoperative pupillography plays a significant role in planning central and peripheral presby-LASIK.9 Patients with poor or sluggish pupillary dilation are not good candidates for presby-LASIK.
Orthoptic evaluation and assessment of strabismus. These evaluations are essential to prevent the postoperative development of diplopia and eye strain and to detect latent nonstrabismic binocular vision anomalies.4
Aberrometry. The measurement of refractive power with aberrometry is necessary to assess the internal aberrations, grade the dysfunctional lens syndrome,6 and detect the presence of early cataractous changes.6,10,11
Counseling. Patients should be counseled on the best type of treatment for their eyes, and they should understand the dynamic nature of presbyopia versus the static nature of treatment. The amount of near vision correction should be based on the patient’s profession and how much and how long they perform near work. They should be told that comparing the vision of both eyes is counterproductive and that a neural adaptation period of up to 3 months should be expected.
APPROACH TO PRESBY-LASIK AND OTHER PROCEDURES
Outcomes with presby-LASIK depend on the patient’s age, occupation, need and type of near work, and personality. Studies have shown that PresbyMax, Presbyond, and monovision LASIK are good choices for patients with myopia and emmetropia and that Supracor (Bausch + Lomb), PresbyMax symmetric, Custom Q (Alcon), and Presbyond are good choices for patients with hyperopia.5 Most of the time, presby-LASIK is executed as a hybrid procedure by incorporating some monovision.
The algorithm in Figure 8 outlines how we typically select the presbyopia-correcting procedure for our patients. In our experience, patients with a normal dysfunctional lens index (DLI), normal corneal topography, and good tolerance of monovision are best suited for monovision LASIK and presby-LASIK. Patients with a normal DLI and suspicious findings on topography or ocular surface abnormalities tend to do well with phakic IOLs. In patients with an impaired DLI, RLE with a monofocal or multifocal IOL can be planned.
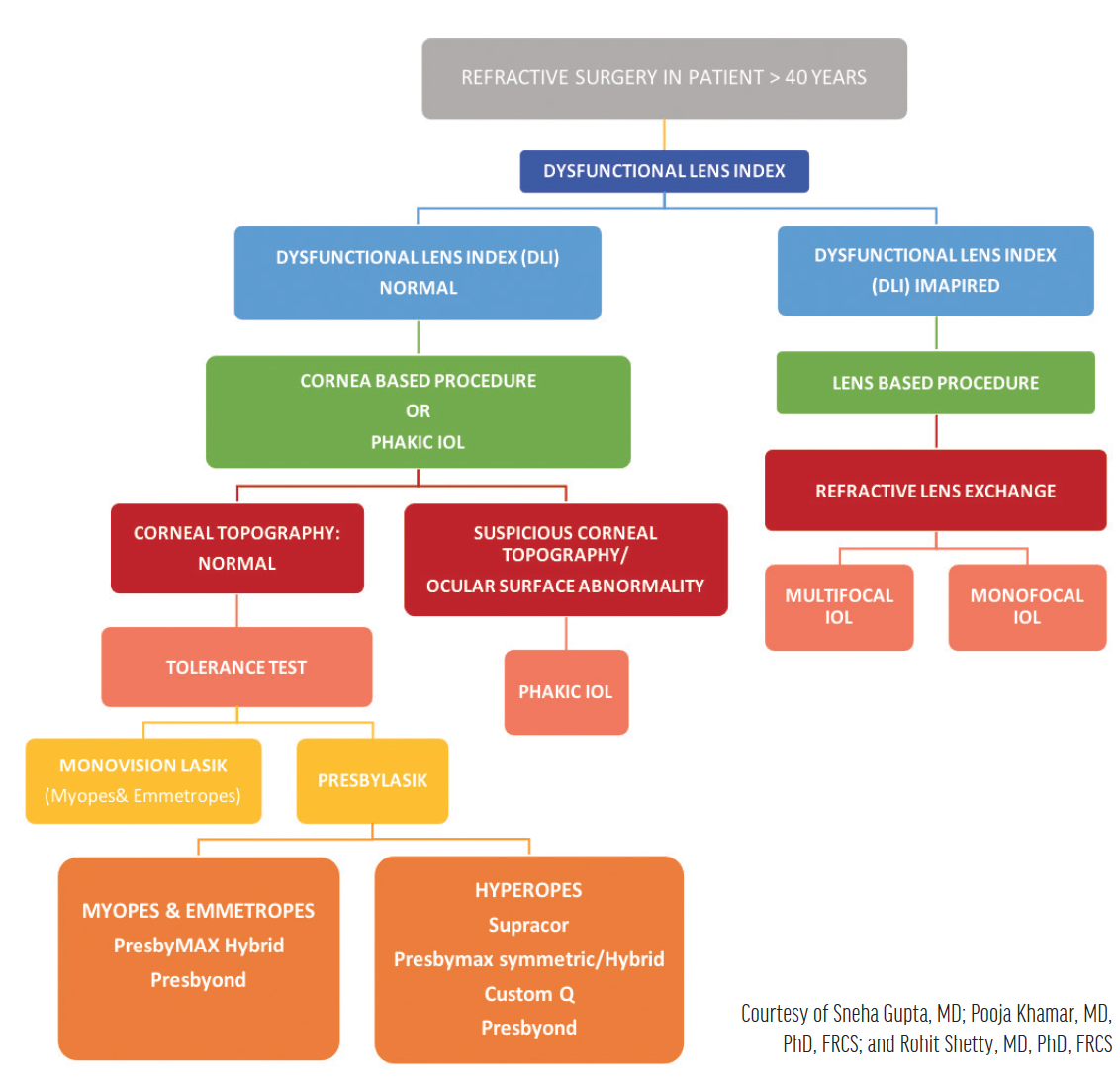
Figure 8. Algorithm for the selection of a presbyopia-correcting surgical procedure.
Nonsurgical treatment of presbyopia in the form of eye drops is being explored. Studies suggest that these eye drops improve near vision by 2 to 3 lines without affecting distance vision,12 but this approach requires further research.
CONCLUSION
Long-term, evidence-based outcomes should be considered before decisions on the medical management of presbyopia are made. We have found our current protocol to be useful for selecting a presbyopia-correcting procedure.
1. Wolffsohn JS, Davies LN. Presbyopia: effectiveness of correction strategies. Prog Retin Eye Res. 2019;68:124-143.
2. Charman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic Physiol Opt. 2014;34:397-426.
3. Zare Mehrjerdi MA, Mohebbi M, Zandian M. Review of static approaches to surgical correction of presbyopia. J Ophthalmic Vis Res. 2017;12:413-418.
4. Muthu S, Jethani J, Annavajjhala S, Gupta S, Gupta K, Khamar P. Integrating binocular vision assessment in refractive surgery work-up: proposition and protocol. Indian J Ophthalmol. 2020;68(12):2835-2846.
5. Shetty R, Brar S, Sharma M, Dadachanji Z, Lalgudi VG. PresbyLASIK: a review of PresbyMAX, Supracor, and laser blended vision: principles, planning, and outcomes. Indian J Ophthalmol. 2020;68(12):2723-2731.
6. Kaweri L, Wavikar C, James E, Pandit P, Bhuta N. Review of current status of refractive lens exchange and role of dysfunctional lens index as its new indication. Indian J Ophthalmol. 2020;68(12):2797-2803.
7. Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52:1994-2005.
8. Herbaut A, Liang H, Denoyer A, Baudouin C, Labbé A. Tear film analysis and evaluation of optical quality: a review of the literature. J Fr Ophtalmol. 2019;42:e21-35.
9. Wilhelm H, Wilhelm B. Clinical applications of pupillography. J Neuroophthalmol. 2003;23:42-49.
10. Faria-Correia F, Lopes B, Monteiro T, Franqueira N, Ambrósio R Jr. Scheimpflug lens densitometry and ocular wavefront aberrations in patients with mild nuclear cataract. J Cataract Refract Surg. 2016;42:405-411.
11. Fernandez J, Rodriguez-Vallejo M, Martinez J, Tauste A, Piñero DP. From presbyopia to cataracts: a critical review on dysfunctional lens syndrome. J Ophthalmol. 2018;2018:4318405.
12. Krader C. Topical drops show promise as treatment for presbyopia. Ophthalmology Times Europe. 2016;12:18-20.




