Strong Medical Education Collaborations Continue During the Pandemic
Nisha Chadha, MD
New York, New York

In March 2020, an email message with the subject line “medical student clerkships canceled effective immediately” popped into my inbox. Elective surgery, including cataract surgery, was also canceled, and New York City, where I practice, was shut down as cases of COVID-19 surged. As an ophthalmologist and a medical educator, I was challenged not only with abruptly transitioning to virtual patient care but also with adapting educational strategies to maintain a high-quality experience for trainees, particularly medical students hoping to match into ophthalmology. Although COVID-19 certainly affected medical education, my community of educators collaborated in real time to find rapid solutions.
IMPACT OF COVID-19 ON MEDICAL EDUCATION
When the volume of COVID-19 cases began surging in the United States, medical student clerkships and visiting rotations were canceled, jeopardizing the timeline of graduation for fourth-year medical students and their residency planning. At the residency and fellowship levels, the cancellation of elective surgery significantly reduced surgical volume and paused job searches. Traditional networking opportunities such as with visiting grand rounds speakers or during research presentations at conferences were also put on hold. These are just a few examples of how COVID-19 negatively affected medical education.
SOLUTIONS
As the challenges snowballed, collaborative efforts to find solutions developed rapidly. Social media was a key means of collaboration. There are numerous examples of successful collaborative efforts, including the following:
- One group of recently matched students hosted a webinar to advise prospective applicants on navigating matching during the pandemic1;
- Faculty, residents, and medical students began to connect and develop both formal and informal mentorship2;
- Local program directors and medical student educators started meeting regularly over Zoom to discuss educational challenges3,4;
- Interinstitutional didactic series were developed in many regions, and more wet labs were conducted with increased faculty mentorship to allow residents to develop their surgical skills while elective surgery was paused; and
- At my institution, the program director started a humanities series that allowed residents to reflect on their experiences working in COVID-19 units.5
Medical educators across the country began developing and sharing virtual ophthalmology curricula, and many programs offered virtual ophthalmology electives as an alternative for students whose visiting electives were canceled. In time, the difficult decision was made to conduct residency interviews virtually.6 In response, many residency programs hosted virtual open houses to allow students to learn about the programs and to meet faculty and residents (Figure 1).
Figure 1. Virtual open houses like the one promoted here give students safe opportunities to learn about residency programs and to become acquainted with faculty and residents.
Courtesy of Nisha Chadha, MD
SILVER LININGS
The collaborations and innovations in medical education that continue to occur are heartening. Once the current public health crisis ends, I am confident that we will emerge stronger and that many of the educational practices we’ve cultivated will endure.
1. Ahmed H, Law JC, Felsted D, et al. Matching ophthalmology amidst coronavirus disease 2019 (COVID-19): lessons that went viral. J Acad Ophthalmol. 2020;12(02):e200-e204.
2. Pettey JH, Abugo UE, Knight OJ, Sun G. Training future ophthalmologists amid and beyond the COVID-19 pandemic, part 2. EyeNet Magazine. November 2020. Accessed December 3, 2020. https://www.aao.org/eyenet/article/training-future-ophthalmologists-amid-covid-part-2?november-2020
3. Duong AT, Van Tassel SH, Alzaga Fernandez AG, et al. Medical education and path to residency in ophthalmology in the covid-19 era: perspective from medical student educators. Ophthalmology. 2020;127(11):e95-e98.
4. Chen RWS, Abazari A, Dhar S, et al. Living with COVID-19: a perspective from New York City ophthalmology residency program directors at the epicenter of the pandemic. Ophthalmology. 2020;127(8):e47-e48.
5. Rosenberg JB, Nair A, Jin S, et al. Editorial: perspectives from the front lines of COVID-19: New York City ophthalmology resident narratives. Curr Opin Ophthalmol. 2020;31(5):386-388.
6. American Association of Medical Colleges. Conducting interviews during the coronavirus pandemic. Accessed December 3, 2020. https://www.aamc.org/what-we-do/mission-areas/medical-education/conducting-interviews-during-coronavirus-pandemic
Virtual Learning and Engagement Are Key in the COVID-19 Era
David Felsted, DO, and Camila Albo
Flagstaff, Arizona
Augusta, Georgia


COVID-19 has had a profound impact on medical education and the application process for all specialties, including ophthalmology. For medical students, this pandemic has disrupted both their in-house and away-rotation experiences. It has also caused a fundamental shift in how medical students connect and engage with members of the ophthalmic community. Many of these changes present challenges, but they also present novel opportunities for medical students pursuing ophthalmology.
On March 18, 2020, the AAO advised all major ophthalmology programs in the United States to limit treatment to only urgent and emergent care.1 Almost overnight, there was a 79% reduction in eye care across the country.2 Consequently, medical students were unable to complete core rotations and subspecialty electives at a crucial period in their training. COVID-19 surges throughout the year resulted in additional times when medical students were unable to scrub in or rotate in surgical services. Limited personal protective equipment, restrictions to OR access, and reduced ophthalmology clinical services decreased medical student exposure in the field.
VIRTUAL COLLABORATION
During the pandemic, we have seen a dramatic increase in communication and collaborations conducted virtually.
Online interviews.Barriers such as COVID-19 travel restrictions have limited the ability of medical students to obtain rotations outside their home institutions or to attend interviews in person. This has placed students without a home program at a greater disadvantage this year. Scheduling for future rotations also poses challenges because shifts in the environment and with the COVID-19 pandemic can occur at any time. Students lack quality face-to-face interaction with program directors, faculty, and residents. However, more widespread use of an online interview process allows students to access programs in places that they might not have considered before because of time, travel, or geographical restrictions. There has also been a significant financial benefit without travel and housing expenses.
Social media. One of this pandemic’s silver linings has been the blossoming of social media use for networking opportunities. Online programs for students pursuing ophthalmology have been supported by leading ophthalmologists in the field, industry, and groups like Bryn Mawr Communications (see YoungMD Connect: A Novel Resource for Young Ophthalmologists).
There has also been a surge in valuable information on medical education for medical students and young ophthalmologists in podcasts, small group forums, and virtual mentorship opportunities. Twitter, Instagram, and other social media platforms are also used more frequently to disseminate information on the resources and mentorship opportunities available to students interested in ophthalmology. It is to be hoped that the increased popularity of and engagement with these platforms and with virtual communication in general are here to stay.
We have also noticed how receptive ophthalmologists in both academia and private practice are to medical students who reach out for advice. Many members of the ophthalmic community are willing and eager to share their insights with future ophthalmologists. Communication within the ophthalmic community is changing this year, in many ways for the better.
CONCLUSION
COVID-19 has presented some formidable challenges for ophthalmology applicants, residency programs, and the ophthalmic community at large. However, the explosion of social media, virtual meeting forums, and creative mentorship opportunities has—in some ways—fundamentally improved how medical students engage with the ophthalmic community.
1. American Academy of Ophthalmology. Recommendations for urgent and nonurgent patient care. March 18, 2020. Accessed December 3, 2020. https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care
2. The Commonwealth Fund. The impact of the COVID-19 pandemic on outpatient visits. 2020. May 19, 2020. Accessed December 3, 2020. https://www.commonwealthfund.org/publications/2020/apr/impact-covid-19-outpatient-visits
3. Ahmed H, Law JC, Felsted D, et al. Matching ophthalmology amidst coronavirus disease 2019 (COVID-19): lessons that went viral. J Acad Ophthalmol. 2020;12(2):e200-e204.
Medical School and Residency Are Free of Charge for Students
Deli Krizova, FEBO, and Pavel Kuchynka, CSc, FCMA
Prague, Czech Republic


Medical training in the Czech Republic lasts 6 years. At the end of training, students must complete rigorous state examinations to obtain the title of general doctor (MUDr). A recent graduate may seek employment in any clinical field of medicine.
TRAINING SPECIFICS
Ophthalmology residency is divided into two parts: basic ophthalmologic training and specialized training. Residency training takes place at workplaces that are accredited for specialized education in ophthalmology and other clinical fields.
To complete the program, residents must complete 2.5 years of basic ophthalmological training followed by examinations and 2 years of specialized training followed by attestation examinations—a total of 4.5 years. Attestations are organized by medical faculty twice a year; the venue depends on the institution of the faculty. Fellowships are offered by individual clinics or organized centrally by the Institute for Postgraduate Medical Education.
PROS AND CONS
The country’s educational system works well as a whole. A major positive is that most of the education, including medical school and the residency program, is free of charge for students. Moreover, the residency program is revised every 2 to 3 years to reflect evolutions in medicine.
The system’s main drawback is the organization of attestation examinations. In the past, these examinations were organized by the Institute for Postgraduate Medical Education, which falls under the Ministry of Health. In 2012, the examinations were transferred to the Ministry of Education, and now their organization is handled by the medical faculties at six institutions. Periodic rotation of the examination site in a relatively small field such as ophthalmology injects differences into the conditions and organization of the examinations, which can confuse young doctors.
Transformations in Training Modules
Wanjiku Mathenge, MBChB, MMed, MSc, PhD
Kigali, Rwanda

The goal of undergraduate and graduate medical training in Rwanda is to produce general doctors and specialists with competencies and skills that meet patients’ reasonable expectations.
The University of Rwanda is the country’s oldest medical school. It admits students who have completed 12 years of formal education, rank at the top of the cohort, and have passed the Advanced General Certificate of Secondary Education. The university’s training program requires 5 to 6 years to complete and culminates with the awarding of a bachelor’s degree in medicine and surgery with honors. The University of Rwanda also offers nine programs that confer a Master of Medicine to doctors who have performed 2 years of public service as general doctors; most of these are 4-year programs.
In order to address a massive shortage in medical doctors in Rwanda, three private universities have opened medical schools, but they have yet to graduate any doctors. The pool of doctors to recruit into ophthalmology residency training remains limited.
Ophthalmology residency training is the only specialty hosted not by the University of Rwanda but by the Rwanda International Institute of Ophthalmology (RIIO), a constituent training program of the College of Ophthalmology of Eastern Central and Southern Africa (COECSA). This program admits doctors from Rwanda, Burundi, and Congo, and it awards a fellowship in ophthalmology after a minimum of 4 years of training. This college-based training is becoming more popular. The emphasis is on equipping every graduate with defined core competencies, including all of the requisite knowledge, technical skills (Figure 2), and soft skills (eg, communication, ethics, patient safety, and professionalism) that are deemed to be essential in the medical profession.
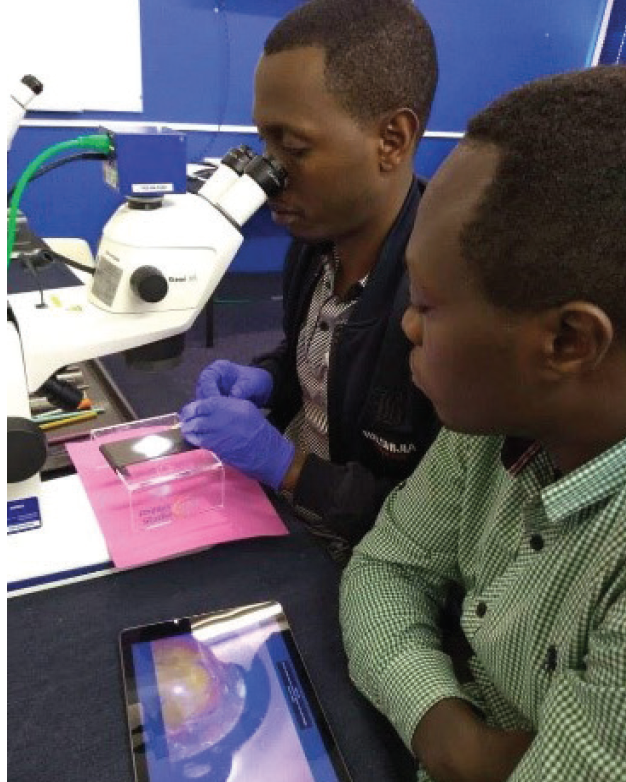
Figure 2. RIIO trainees use surgical simulation training for cataract surgery.
Courtesy of Wanjiku Mathenge, MBChB, MMed, MSc, PhD
The program draws on the best practices of the UK’s Royal College of Ophthalmology1 and the International Council of Ophthalmology (ICO). Trainees at the RIIO must pass the ICO’s examinations in visual sciences, optics and refraction, and instruments as well as in clinical sciences before presenting for a clinical examination offered by the COECSA. Candidates must show that they have achieved all of the COECSA residency training milestones and charted their progress during clinical placements using workplace-based assessments.
COECSA has members from 12 African countries. Adoption and enforcement of the college training standards have been possible at new institutions like the RIIO, but the transition is happening more slowly at older institutions with Master of Medicine in ophthalmology training programs that are governed under institutional frameworks that existed before COECSA.2 For example, training lasts 3 years in some programs and 4 years in others. A goal of the COECSA is to develop its own written examinations and either to slowly replace the ICO examinations or to have a blend of both.
The first cohort of ophthalmology residents at the RIIO are on track to complete their training by mid-2022. Once they begin practicing in hospitals, the quality of their services will give a true indication of the value of this training model.
1. Corbett MC, Mathenge W, Zondervan M, Astbury N. Cascading training the trainers in ophthalmology across Eastern, Central and Southern Africa. Global Health. 2017;13(1):46.
2. Dean W, Gichuhi S, Buchan J, et al. Survey of ophthalmologists-in-training in Eastern, Central and Southern Africa: A regional focus on ophthalmic surgical education. Wellcome Open Res. 2019;4:187.
Using Seven Key Recommended Goals for Training
Radhika Rampat, MBBS, BSc(Hons), FRCOphth, and Andrew Scott, PhD, MD, FRCOphth, MRCSEd, FEBO
London, United Kingdom


After 4 to 6 years in medical school in the United Kingdom, students graduate with a bachelor of medicine/bachelor of surgery (MBBS) degree with or without a bachelor of science degree. Full registration is achieved by completing another 2 years of foundation training (Figure 3).
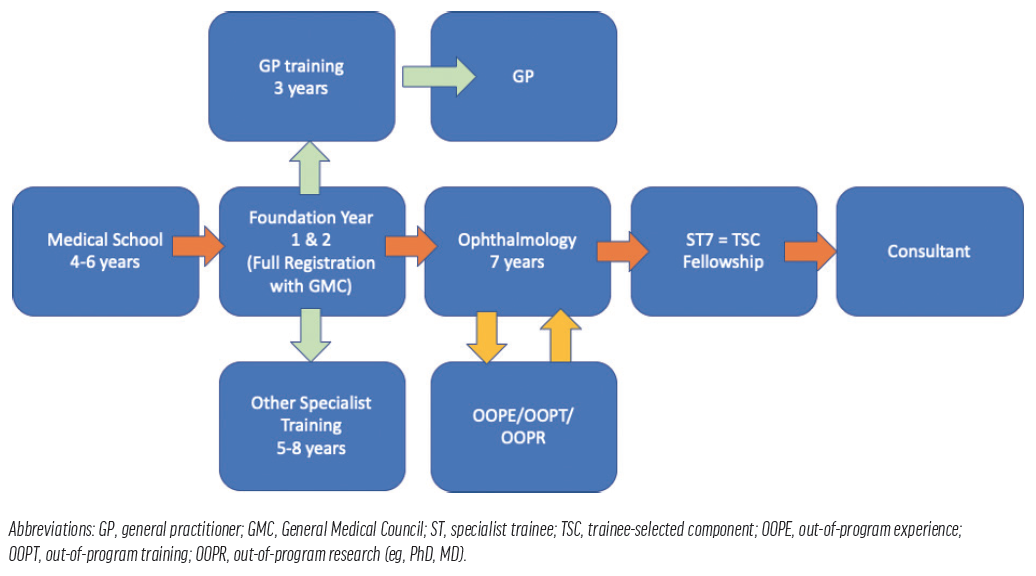
Figure 3. A summary of training in the United Kingdom.
Selection into ophthalmology programs in our country is highly competitive. Participants may choose to pursue either an academic route by incorporating research into their training program or other degrees prior to application to an ophthalmology training program in order to improve their chances of selection. Each of the 7 years of training includes a rigorous Annual Review of Competence Progression, and participants must complete three tough examinations that include a refraction certificate and two Fellowship of the Royal College of Ophthalmologists examinations (FRCOphth parts 1 and 2).
Specialty training occurs within National Health Service (NHS) hospitals, but it is the Deanery and Royal College of Ophthalmologists that ensures standards and quality of training are upheld. Clinical governance plays a major role in UK training; participants are not only taught about it but must also submit evidence of practicing it. Figures 4 and 5 show our specific training journeys.
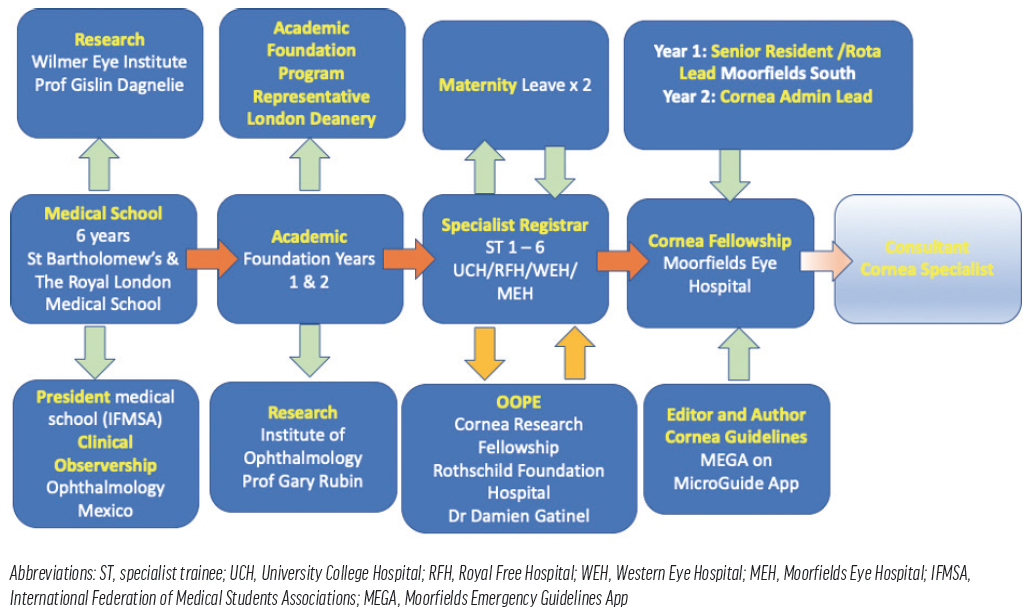
Figure 4. Dr. Rampat’s journey from medical school to present, as she embarks on consultant applications and completes her second fellowship.
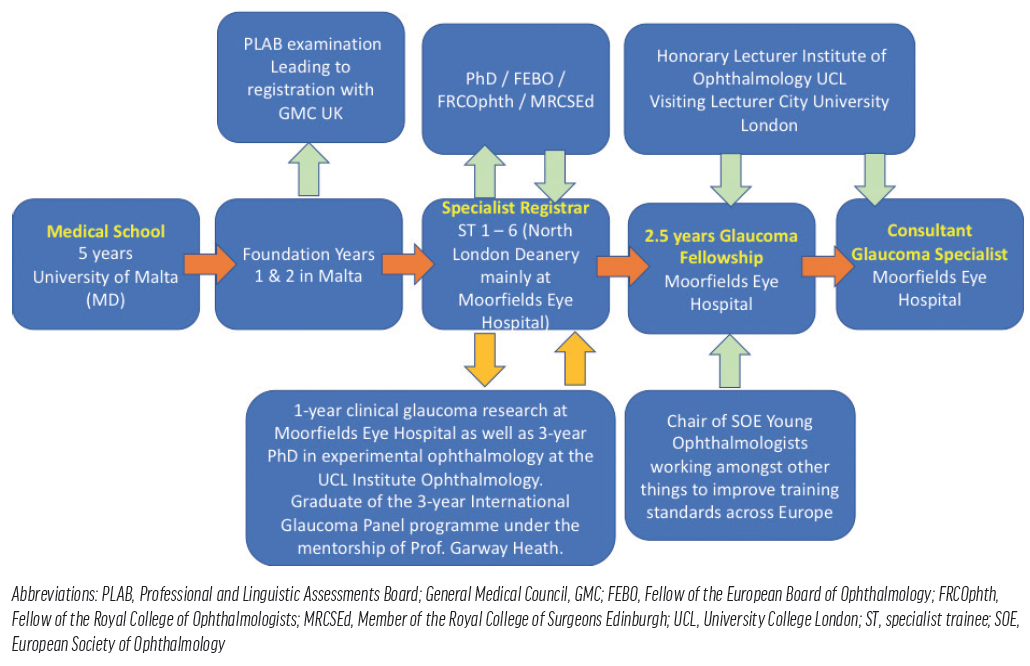
Figure 5. Dr. Scott’s journey from medical school to his current glaucoma specialization at Moorfields Eye Hospital.
QUALITY
The United Kingdom’s structured training programs are held in high regard internationally and attract participants from overseas. Because salaries for training doctors are partly funded by the Deanery, there is an incentive for NHS hospitals to provide a high standard of training in order to retain their trainees. These individuals provide invaluable work to support the NHS, and the Deanery may remove them from a hospital if the training standards are not met.
Only through high-quality training can the highest standard of care for patients be ensured (see Seven Key Recommended Goals for Training).
Seven Key Recommended Goals for Training
- Established structure
- Standardized curriculum
- Adequate supervision
- Regular appraisals and assessments
- Surgical logbook evidence
- Portfolio of training evidence and appraisals
- Formal fellowships
TIME
A complaint sometimes voiced about the UK’s training program is that it is too long, but it is the only one in Europe that incorporates a mandatory year of fellowship in a specific specialty of choice.
Moreover, the length of the program helps to ensure a depth and breadth of experience. For instance, participants are not only taught technical skills but also how to approach practice with emotional, analytical, and creative intelligence that supports their surgical independence and decision-making ability when they receive a Certificate of Completion of Training and start applying for jobs as a consultant.
possible improvements
A possible change to the system would be to reduce general training time and increase fellowship time. Efforts could also be made to develop fewer but higher-qualified, dedicated trainers. Additionally, the number of trained medical ophthalmologists could be expanded to help manage a growing burden of vision loss that does not require surgical intervention.
Integrating Competency-Based Care Into Residency Programs
Jorge E. Valdez-García, MD, PhD
Monterrey, Mexico

The goal of graduate medical education is to ensure that physicians-in-training become competent to practice in their field of medicine. Training in ophthalmology residency programs is highly competitive.
In Mexico, medical residency is defined as a set of academic, care, and research activities that are endorsed by universities and the operative programs implemented by the clinical training sites. Each residency program must be registered with the National Medical Residence System of the Interinstitutional Commission for the Training of Human Resources in Health.
TRAINING OPPORTUNITIES
There are 13 academic residency programs in ophthalmology endorsed by universities that operate in 28 clinical training sites (hospitals), and the National Autonomous University of Mexico endorses 46% (n = 13) of these training sites.
Access. Training programs are concentrated in a few cities; the cities with the highest concentration are Mexico City (46%), Monterrey (14%), and Guadalajara (11%). Geographically, of the 32 states that make up the Mexican Republic, only 30% (n = 10) have a residency program in ophthalmology.
In order to obtain a spot in a residency program, the graduate physician must pass the highly selective National Examination of Medical Residency Applicants. Candidates compete for 292 spots (271 for Mexicans and 21 for foreigners) in the different academic programs. The largest number of training opportunities (115 or 42%) are located in the clinical facilities of the Mexican Institute of Social Security. Another 54 slots (19%) are available from the Ministry of Health. Approximately 20% of training opportunities are available through five nongovernmental organizations; one of them, Tecnológico de Monterrey, has an innovative public-private (nonprofit) approach.
Certification. After completing a 3- to 4-year training period (only three programs require 4 years to complete), residents graduate with a university degree of specialist in ophthalmology. To practice ophthalmology, graduates must obtain a cedula professional license, which requires passing the Mexican Board of Ophthalmology certification examination. This is a practical and theoretical examination.
Accreditation. Excellence in clinical care demands quality medical education. This principle has prompted initiatives for evaluation and accreditation in Mexico’s residency programs. The National Council of Science and Technology established an accreditation system for medical residencies, the List of the National Graduate Quality Program. Only 10 (35%) clinical training sites are accredited—one with an international competence level (Tecnológico de Monterrey), three with a consolidated level, and six with a development level.
CONCLUSION
Competency-based medical education is gaining strength as a solution to the challenges of the modern era. The goal is to develop Mexico’s ophthalmology residency programs to provide this type of education.
In Europe, Most Ophthalmology Fellowships Are Found Abroad
Riccardo Vinciguerra, MD
Monterrey, Mexico

Ophthalmology residency in Italy is not only medical but surgical as well. In some ways, this design provides those of us who completed residencies in Italy with an advantage over those who completed residencies in countries that do not include surgical rotations. The problem in Italy is that not every resident gets the same type of surgical experience and that some do not get any surgical experience at all. It is highly dependent on the program and the faculty.
After completing a 4-year ophthalmology residency in Italy, the next logical step, I believe, is fellowship. Fellowships are not mandatory, but to my mind, they should be—especially for individuals who want to specialize in areas like cornea, glaucoma, and vitreoretinal surgery. How else are you to truly prepare for all of the procedures required in anterior and posterior segment surgery? How else can you experience full-on what you’re going to do for the rest of your life?
LOOKING ABROAD
In Italy and many other European countries, there are no real fellowship programs, so those who are interested in pursuing one look abroad. One popular fellowship destination is the United Kingdom. I completed two fellowships, one glaucoma and one cornea, in Liverpool. Both fellowships took place at referral centers, which provided me with the opportunity to perform complex surgeries. It also helped me to decide to pursue corneal surgery as a specialty.
Another benefit to looking abroad for fellowship is that it exposes you to other cultures, other languages, other people, and other landscapes. It helps you to grow, not only as a doctor, but also as a human, through the experiences you share with colleagues and other residents of the country in which you are living (Figure 6).

Figure 6. Dr. Vinciguerra (left) with his former fellows Esmaeil Arbabi, MD, and Argyrios Tzamalis, MD.
Courtesy of Riccardo Vinciguerra, MD
NEED FOR EXPANSION
In many cases, including mine, fellowships are found through referrals or word-of-mouth recommendations. Fellowships are not in mainstream practice in most of Europe, and many of those available are in large hospitals. This is different from in the United States, for instance, where many private practices offer specialized fellowships.
Hospital-based fellowships have advantages and disadvantages. On the one hand, they expose you to a variety of surgeries. On the other, it can take much longer to learn things, and there is a limited amount of technology.
If you look at the credentials of many of the rising stars in ophthalmology in Europe, you will notice that most of them have done a fellowship abroad—usually in the United States or the United Kingdom. I think there is a large unmet need in Europe for more fellowships, and it is something that as a Union we should think about improving.
Private Practice Fellowships Continue to Emerge
Robert J. Weinstock, MD
Largo, Florida

Medical training, and more specifically ophthalmology training, has not changed much in the United States for decades. After obtaining an undergraduate degree at a 4-year university or college and passing the medical school entrance exam, students may apply to allopathic and/or osteopathic medical schools. These typically 4-year programs involve 1 to 2 years of didactic training followed by 2 years of clinical training in hospitals and medical centers. Near the completion of medical school, students choose an area of expertise and apply for residency training at an academic university or a setting certified by the Accreditation Council for Graduate Medical Education (ACGME).
OPHTHALMOLOGY RESIDENCY CRITERIA
Residents typically begin with a 1-year internship program in internal or family medicine, or they complete a transitional internship year. This is followed by 3 years of specialty residency in a program certified by the ACGME. During ophthalmology residency specifically, a number of criteria must be met to graduate, including completing a certain amount of procedures as the primary surgeon and passing the Ophthalmic Knowledge Assessment Program (OKAP) examinations. OKAPs are administered by the AAO to US and Canadian ophthalmology residents in each year of training. Residents may also take step one of the written examination of the American Board of Ophthalmology (ABO) for board certification.
After completing 4 years of residency and the three steps of the United States Medical Licensing Examination, an ophthalmology resident may begin practicing as a general ophthalmologist. However, some may choose to pursue fellowship training in a desired subspecialty first. During the years immediately following residency, individuals may take the ABO step 2 oral examination to become board-certified. It is important to note that individuals are not permitted to practice medicine until they apply and are granted licensure by an individual state.
THE BENEFIT OF FELLOWSHIPS
As the field of ophthalmology becomes more complex with an ever-increasing body of knowledge and an expanding quiver of procedures and surgeries, subspecialty fellowships in retina, oculoplastics, glaucoma, pediatrics, and cornea have evolved in response. Today, the subspecialty of cataract and refractive surgery is beginning to blossom, and many fellowships are now available in this emerging space.
Some formalized ophthalmology fellowships require board exams and certifications, such as the oculoplastic surgery fellowships governed by the American Society of Ophthalmic Plastic & Reconstructive Surgery. Most, however, are more loosely governed. Fellowships can last 1 year or, like those in plastics and surgical retina, 2 years.
In the United States, surgeons in the academic and university settings are finding it increasingly challenging to obtain adequate training and experience, especially in cataract and refractive surgery, as will be addressed in this article. This is much of the reason why private practice fellowships have surfaced in this arena. (Editor’s note: For more on fellowships, see YoungMD Connect: A Novel Resource for Young Ophthalmologists.)
YoungMD Connect: A Novel Resource for Young Ophthalmologists
An educational hub for continued learning, mentorship opportunities, and meaningful connections.
By Laura Straub, Editor-in-Chief
Modern ophthalmology training and residency programs prepare young physicians to diagnose, evaluate, and treat ocular diseases. But, after 4 years of residency and studying for and passing the Ophthalmic Knowledge Assessment Program and United States Medical Licensing examinations, an increasing number of individuals choose to continue their training through fellowships before beginning practice.
Finding and applying for fellowships can be laborious. Enter YoungMD Connect (Bryn Mawr Communications), a new mentorship and educational platform designed to help young ophthalmologists establish meaningful connections, advance their training, and make informed decisions about the future of their careers. In addition to hosting a complete list of private practice and academic fellowship opportunities in the United States and some in Canada, YoungMD Connect boasts a variety of educational offerings.
PLATFORM FUNCTIONS
The YoungMD Connect platform is in its infancy. There currently are four main functions, with more in development. Each function is built on the foundation of peer-to-peer education and mentorship.
- Educational workshops. The aim of curated content in YoungMD Connect’s educational workshops is to help young ophthalmologists navigate the nuances of skills training, innovations in ophthalmology, business management, and advances in patient care.
- Mentoring sessions. Small group mentoring sessions and private office hours with ophthalmic thought leaders that are facilitated by YoungMD Connect offer invaluable opportunities for young ophthalmologists to network with giants in the field.
- Private practice and academic fellowships. The YoungMD Connect website is home to an interactive map of all US-based and some Canadian-based ophthalmology private practice and academic fellowship programs (Figure). Viewers can explore each fellowship opportunity and narrow their search for the perfect fit.
- Events. Educational and networking events organized by YoungMD Connect are designed to help young practitioners build connections with ophthalmic colleagues and members of industry.
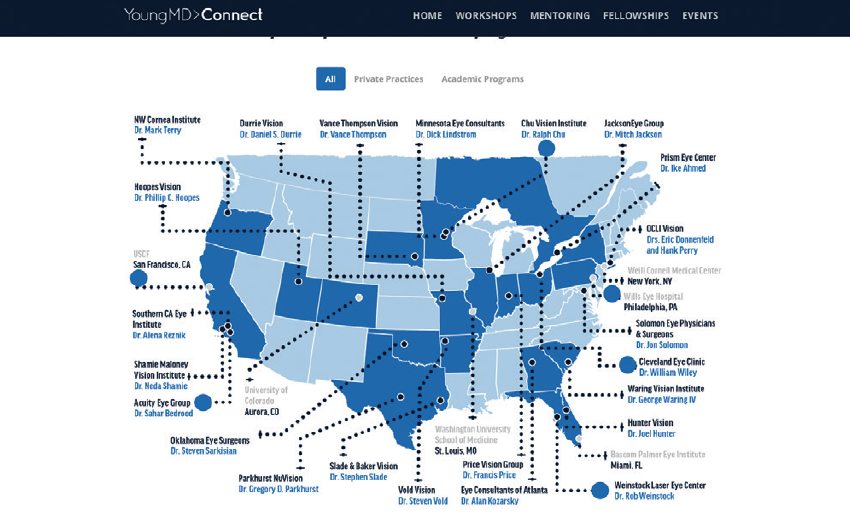
Figure. At press time, the current interactive map of fellowship programs featured on YoungMD Connect’s website.
CONCLUSION
Borne of the desire to connect aspiring and young ophthalmologists with their peers and mentors, YoungMD Connect is poised to become a modern hub for educational workshops and events, small group mentoring sessions, and information on academic and private practice fellowship opportunities. By promoting traditional and nontraditional educational opportunities, YoungMD Connect establishes and strengthens more meaningful connections in ophthalmology.
CHALLENGES AND MOVING FORWARD
Many challenges with ophthalmology training exist, frequently including a lack of funding in academic settings and the inability of academic centers to acquire new technology and stay current with the latest innovations.
Further, academic training institutions vary in the diversity of their subspecialty-trained faculty, causing flux in the level of trainees’ exposure to the various specialties in the field. To gain precious experience in cataract surgery, many residents work in Veterans Administration hospitals or seek positions abroad. Most of the advanced cataract and refractive surgery performed in the United States occurs in the private practice setting, as is an increasing volume of clinical research.
Another interesting feature of medical training in the United States is that formal traditional medical training is mostly limited to disease diagnosis, evaluation, and treatment. There is little exposure to holistic and preventive medicine.
Advancing the educational process
Medical training in the United States is evolved and functional, but there is always room for improvement. It is the responsibility of today’s leaders to evaluate what does and does not work and to continue to refine and incrementally advance the educational process.




