All panelists are paid consultants of Johnson & Johnson Vision.
PP2022CT5011
INTRODUCTION
Modern cataract surgeons have so many different IOLs—indeed, so many different classes of technology—at their disposal that it is understandable how some may feel overwhelmed by options. Given most cataract surgeons by nature wish to know the pros and cons of each platform that they may implant in a patient’s eye, it is incumbent upon those with familiarity with new technology to share with their colleagues their subjective opinions and experiences, to review objective trial data, and to discuss surgical pearls that may decrease the learning curve of surgeons adopting new technology.
This fall, Johnson & Johnson Surgical Vision will debut the InteliLight™ portfolio. InteliLight™ technology comprises three proprietary innovations: violet light filtration, a new echelette design, and achromatic technology. When added to Johnson & Johnson’s line of presbyopia-correcting IOLs, InteliLight™ will support the gap in contrast and low-light performance. InteliLight™ technology will be added to the TECNIS Symfony™ IOL Legacy, thereby creating a next-generation technology that pushes presbyopia-correcting IOLs into the future.
The new TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ (Johnson & Johnson Vision) maintains the numerous strengths of the legacy design while capitalizing on the latest manufacturing advancements proprietary to Johnson & Johnson IOL production. These improvements are expected to minimize the unwanted visual symptoms experienced by some patients with the TECNIS Symfony™ IOL Legacy—all while maintaining quality, contrast, and clarity of vision in all lighting conditions.
Surgeons know that contrast sensitivity and low-light visual performance are critical as patients age, and that reducing slips and falls and empowering patients to drive—even at night—are key to improved quality of life, mobility, and confidence. By filtering violet light and reducing light scatter, the intensity of halos, glare, and starbursts will be reduced; by allowing blue-wave light to remain unblocked, nighttime contrast sensitivity remains at an all-time high.1 High-resolution lathing will also reduce halo intensity and light scatter, and leveraging achromatic technology will enhance daytime and nighttime contrast via correction of chromatic aberrations.2,3
All of these innovations boil down to a single essential: that InteliLight™ IOLs offer great contrast and low-light performance among presbyopia-correcting IOLs. These new lenses marry the proven TECNIS® IOL platform with the latest InteliLight™ innovations to create a new family of IOLs: the extended depth of focus TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ and the high performance hybrid TECNIS Synergy™ IOL3—both of which will be offered with TECNIS® Toric II haptics for astigmatism correction.
At the 2022 ASCRS annual meeting, a panel of doctors convened to discuss the newest offering in the InteliLight™ portfolio: the next-generation extended depth of focus TECNIS® Symfony™ OptiBlue™ IOL with InteliLight™. The roundtable was moderated by George Waring IV, MD, and the panel comprised Daniel Chang, MD; Douglas Grayson, MD; Douglas Koch, MD; J. Morgan Micheletti, MD; and Karolinne Rocha, MD, PhD. During their discussion, the panel reviewed how the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ delivers excellent distance and intermediate vision, as well as functional reading vision for many patients. They also discussed the tolerance of the TECNIS Symfony™ IOL to refractive error; using the lens in challenging patient profiles, reliable material, high Abbe number, and low chromatic aberration of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™; and the science behind blocking violet light and how violet light filtration and new high-resolution lathing reduces halos and dysphotopsias.
TECNIS Technology
George Waring IV, MD: Before we start an in-depth discussion about our personal experiences with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, I’d like to zoom out and begin our conversation by focusing on the TECNIS® family of IOLs in general. What makes TECNIS® technology unique?
Daniel Chang, MD: The best part of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™is its heritage in the TECNIS® line of technology. The TECNIS® portfolio uniquely offers patients the full spherical aberration correction of the average cornea on a hydrophobic acrylic material with the highest Abbe number and lowest chromatic aberration in its class. All of this is crafted with a precise cryolathing process that drives the high visual quality for which TECNIS® is known.4
The primary goal of cataract surgery is to improve quality of vision, so IOLs should always prioritize image quality to provide best visual quality for patients. Patients who wish to address presbyopia at the time of cataract surgery will need to balance three elements: visual quality, range of vision, and dysphotopsias. While some surgeons think of these three elements as a zero-sum game, new innovations such as the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ can change the equation. For example, while some IOL platforms decrease dysphotopsias by reducing range of vision, InteliLight technology can reduce dysphotopsias and even increase visual quality—all the while maintaining range of vision. This allows us to focus on patient consultation, surgical precision, and follow-up, thereby allowing us to provide the optimal preoperative, intraoperative, and postoperative experience.
Karolinne Rocha, MD, PhD: Surgeons commonly think of monofocal IOLs as a separate class from presbyopia-correcting IOLs for obvious reasons, including that monofocal IOLs do not commonly result in dysphotopsia occurrence. Given Dr. Chang’s framing of TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ technology, it seems like the gap between presbyopia-correcting lenses and monofocal lenses in the TECNIS® family of technology has grown smaller, representing a major positive change for our field.
J. Morgan Micheletti, MD: When the TECNIS Symfony™ launched 6 years ago, it aimed to provide image quality comparable to the TECNIS® Monofocal 1-Piece IOL (Johnson & Johnson Vision). While the quality of vision reported by patients after implantation with TECNIS Symfony™ IOL was excellent, some patients reported dysphotopsias such as halos and starbursts, which ultimately led to some surgeons moving away from using TECNIS Symfony™ IOL.
Douglas Koch, MD: We should note that dysphotopsias are linked to presbyopia-correcting IOLs in general, and not exclusively to a particular technology. Fortunately for our patients (and us surgeons), the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is designed to minimize those dysphotopsias without sacrificing the strong quality of vision earlier patients experienced. Several technical specifications of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ distinguish it from earlier iterations and from similar IOLs in the same class of technology, thereby allowing diminution of dysphotopsias without compromising vision quality.
Dr. Chang: The violet-filtering technology used in the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ design is one of its most important elements, since it filters the precise wavelengths needed to reduce dysphotopsias while maintaining the visual quality that patients have come to expect with presbyopia-correcting lenses, particularly in scotopic conditions. The first approved OptiBlue™ IOLs were approved by the US Food and Drug Administration (FDA) approximately 10 years ago; it was first engineered as an improvement to existing blue-light filtering chromophores.
As researchers learned more about the effects of light filtering and dysphotopsia, it became clear that filtering only the highest energy wavelengths of visible light could improve light scatter and contrast while maintaining scotopic vision and color perception—in short, it could reduce dysphotopsias and improve quality of vision. Still, knowing that broad-spectrum light filtration could have deleterious effects on scotopic vision and circadian rhythms, researchers and engineers refined the specificity of the chromophore used in the manufacturing of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ to balance these long-term safety concerns with the optimized visual function.
Douglas Grayson, MD: I do think we should note that, when talking to patients about light-filtering technology, we should make it clear that TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is not a part of the current trend of blue light filtration that our patients see in commercial, nonmedical settings. Rather, it optimizes visual function through transmission of blue light and filtering violet light. That is, the light-filtering technology leveraged by TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is not the same as the blue light-filtering glasses a patient buys online to mitigate the effects of increased screen time in the digital era.
Dr. Waring: Dr. Chang, can you provide further details about the engineering of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ vis-à-vis the reduction of dysphotopsia intensity?
Dr. Chang: Violet light scatters more than blue light due to the former’s shorter wavelength and higher energy, meaning that while the dysphotopsias that patients experience are broad spectrum, they are most severely affected by violet light. The specific filtering of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ blocks light less than 430 nanometers (nm), a wavelength that is strictly violet.3 The cutoff curve for this technology is steep, and having such a steep curve means that only violet light shorter than a particular wavelength is specifically blocked, rather than a broad spectrum of wavelengths that include blue. Thus, while other broad-spectrum blue-light filters block some blue light yet still transmit a significant amount of violet wavelengths as short as 410 nm, the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™blocks more harmful high-energy violet light while transmitting all of the healthy blue light.5
Dr. Rocha: Design changes that filter violet light appeal to the engineer in all of us, but I think putting the upshot of those changes into a modern context illustrates the practicality of blocking shorter wavelengths of light.
After implantation of any type of presbyopia-correcting IOL, our patients often complain about dysphotopsias complicating their driving ability, and they point to streetlights and traffic signals as areas of concern. When we consider that modern infrastructure changes have brought about wider adoption of lamps and traffic lights that use light-emitting diodes (LEDs), which have a shorter wavelength than incandescent lights, we might better understand why so many patients report difficulty driving at night. As LEDs are becoming more prevalent in our society, the need for blocking short-wavelength light may become more important in this patient population.
Dr. Waring: The customized manufacturing process of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is worth noting, too. All IOLs in the TECNIS® family are cryolathed and tumble polished to smooth any lathing marks. Johnson & Johnson engineers have learned to create echelettes via use of high-resolution lathing, which allows a polishing effect without interfering with the ability to properly diffract light, thereby reducing scatter (Figure 1). In short, high-resolution lathing allows the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ to reduce light scatter while maintaining refractive characteristics.
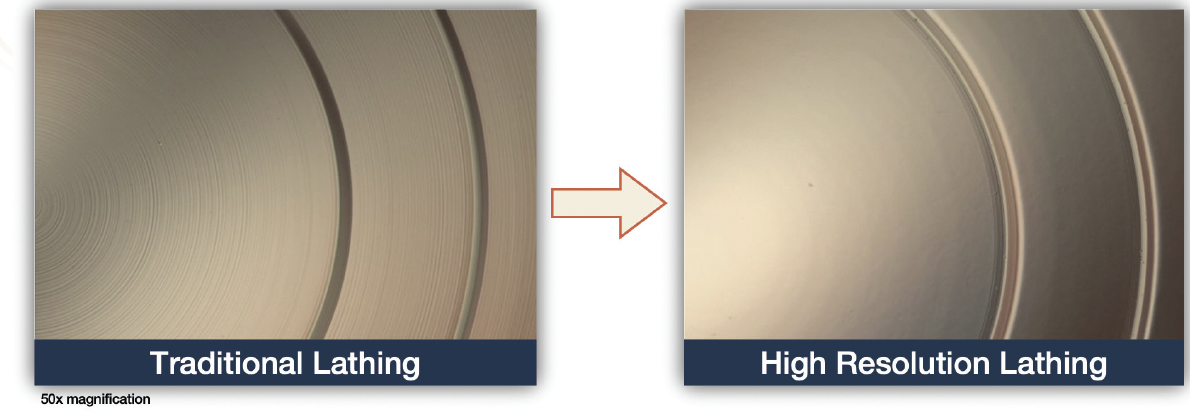
Figure 1. Traditional lathing relies on echelettes that are difficult to tumble polish due to their steep curves. High-resolution lathing creates echelettes that are essentially polished, which reduces light scatter.
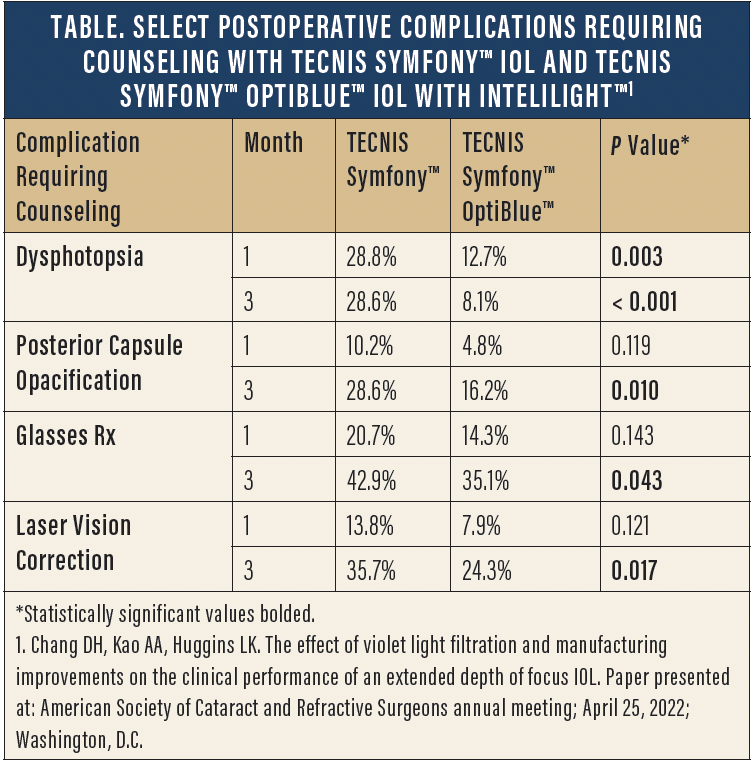
Dr. Chang: At the 2022 ASCRS annual meeting, my colleagues and I shared retrospective clinical data from a prospective, single-center consecutive case series comparing outcomes following implantation of either the TECNIS Symfony™ IOL (63 eyes of 43 patients) or the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ (73 eyes of 48 patients).6
Visual and refractive outcomes were similar among both groups at months 1 and 3. The TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ group also showed a 45% reduction in dysphotopsia complaints at months 1 and 3. The percentage of patients who have any documented postoperative counseling for dysphotopsia was significantly lower at months 1 and 3 in the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ group compared with the TECNIS Symfony™ IOL group, with a 72% reduction in dysphotopsia-related counseling occurring at 3 months.6 For more information regarding postoperative counseling rates for dysphotopsia, posterior chamber opacification, postoperative spectacle use, and laser vision correction—all of which were significantly lower among patients implanted with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™—see the Table.
Dr. Micheletti: We may sense subjectively that the patient experience is enhanced with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, and it’s reassuring to hear that our observations are confirmed by datasets such as the one you outlined from your research, Dr. Chang. Were there any other significant differences observed, perhaps outcomes that might affect clinical workflow?
Dr. Chang: There were significant reductions in the volume of secondary interventions and the overall number of patient visits. We observed that rates of YAG capsulotomy were lower in the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ group vs the TECNIS Symfony™ IOL group (2.7% vs 8.3%; P = 0.011).6 IOL exchange was needed in 1 patient in the TECNIS Symfony™ IOL group compared with no patients in the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ group (P = 0.038).6 Overall, patients in the TECNIS Symfony™ IOL group required 2.1 ± 1.7 visits compared with 1.7 ± 1.1 visits in the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ group (P = 0.033), an outcome that will be particularly attractive to surgeons with busy clinics and to patients who wish to get back to their routine lives.6
IDENTIFYING PROPER CANDIDATES
Dr. Waring: Cataract surgeons must be experts in gauging which patients are good candidates for specific technologies. I’d like to hear from my colleagues how they decide which patients are good candidates for premium technology in general, and which of those patients should be considered for the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™.
Dr. Micheletti: Any patient who presents to my clinic seeking spectacle independence is considered for an advanced technology IOL. If I determine that a patient is not a good fit for continuous range of vision technology—due to concerns such as patient personality, pathologic findings, or anatomic limitations—then I move on to considering whether they’re a good fit for TECNIS Symfony™ OptiBlue™ IOL with InteliLight™.
If a patient is looking to reduce spectacle dependence but is concerned about dysphotopsias, then my initial algorithm shifts to considering them for an extended depth-of-focus (EDOF)IOL, such as TECNIS Symfony™ OptiBlue™ IOL with InteliLight™.
Dr. Waring: You mentioned that patient personality and examination findings affect your decision-making. Can you further expand on that?
Dr. Micheletti: I find that patient satisfaction after surgery is directly linked to the management of expectations preoperatively. As such, thorough preoperative education and counseling helps to provide the foundation for reasonable expectations. After this discussion about the benefits and limitations of the technology, I exercise caution when considering patients with unreasonably high expectations or a sense of perfectionism.
Regarding the clinical exam, if a patient shows evidence of a progressive retinal disease or has moderate to severe glaucoma, then I do not consider that patient a candidate for a presbyopia-correcting IOL. Before the latest generation of EDOF IOLs, I ruled out presbyopia-correcting technology in any patient with an epiretinal membrane (ERM). Today, however, I believe that patients with mild ERMs are eligible for EDOF IOLs that maintain high levels of contrast sensitivity, and TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is an excellent option in those patients for this reason.
Dr. Koch: I agree that a condition such as mild ERM—particularly if I sense that it will develop slowly—is not a disqualifying factor for patient selection regarding the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, although it commonly is a disqualifying factor for other presbyopia-correcting IOLs. If there is a mild retinal condition that, at worst, might take years to minimally affect the patient’s contrast, then the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, in my opinion, may provide excellent vision for that time period and will not impair even after it sets in.
Like many of us on the panel, I first started using the TECNIS Symfony™ line of IOLs several years ago. Use of the earliest iterations of TECNIS Symfony™ IOL technology resulted in patients having positive responses to distance vision, intermediate vision, and contrast sensitivity. Among patients who had issues with dysphotopsia—an issue linked with all presbyopia-correcting IOLs—a few had intense reactions to severe glare, and there was little I could do to satisfy them.
Knowing that the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ was designed to specifically address these issues, I have implanted it in a handful of patients. During follow-up consultations, I pay specific attention to dysphotopsia concerns. So far, many of my patients have said that they love their vision with the lens. They cited better overall quality of vision and contrast.
Dr. Waring: I have found that patients who want strong distance vision are great candidates for the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™. Have you had a similar experience?
Dr. Koch: I often implant the TECNIS Symfony™ IOL in patients with a history of refractive surgery, assuming fairly regular central topography. That history alone tells me that the patient prioritizes distance vision and may want intermediate vision that does not require glasses. In today’s world, intermediate vision includes seeing fine print on a cell phone or tablet held at arm’s length; I call this range ‘intermediate plus.’ The TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ works at that range to our patients’ satisfaction, which is an advantage in the digital age.
Dr. Grayson: Like Dr. Koch, I consider those with a history of laser-based refractive surgery as a special subset of patients. I found that this patient population did very well with the TECNIS Symfony™ IOL—so well, in fact, that it was my primary go-to lens for post-refractive presbyopic patients seeking improved depth of focus following cataract surgery. The high patient satisfaction rates were due, in part, to the forgiving nature of the TECNIS Symfony™ IOL: low levels of residual refractive error did not greatly impact patient satisfaction. In my estimation, use of the next-generation TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ in this patient population delivers the same—if not better—overall outcomes compared with the TECNIS Symfony™ IOL Legacy.
I’m impressed by surgeons who have a talent for the science of optics, and whose framework for understanding the relationship between patient satisfaction and implantable technology relies on the concepts such as ray patterns and chromatic aberrations. I, however, tend to focus more on the real-world consequences of surgery. For example, if a patient returns to me for several postoperative visits to complain of trouble while driving at night, that tells me all I need to know about whether the lens they received was right for them.
In my estimation, I explanted approximately one TECNIS Symfony™ IOL every 6 to 12 months due to issues with dysphotopsia, which is equivalent to explanting 1 in every 500 TECNIS Symfony™ IOLs. Since the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ came on the market, I moved all patients who would otherwise be eligible for a TECNIS Symfony™ IOL Legacy to this new platform. Several hundred of my patients have received the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ and, so far, I have not explanted any due to dysphotopsia issues.
Drs. Micheletti and Koch discussed their comfort with implanting the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ in eyes with mild ERMs. I would add that, in my experience, eyes with mild glaucoma and eyes with ocular surface disease do well with this lens, too. Both conditions need to be properly managed, of course. Still, my ability to offer the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ to a wider set of patients has expanded my practice’s goal of helping as many patients as possible to achieve optimized vision.
Dr. Rocha: As with all other premium IOLs, ocular surface optimization is key to success. When patients understand that delaying surgery a few weeks in order to optimize the ocular surface will pay large dividends in the future, then they are likely to be patient with their preoperative regimen. Accurate biometry and topography measurements, too, are foundational to success. Proper power calculations using newer generation formulas may help mitigate the intensity of dysphotopsia in some patients, as patients who end up with residual myopic refractive error are likely to experience dysphotopsias.
DYSPHOTOPSIA WITH PRESBYOPIA-CORRECTING LENSES IN MODERN CATARACT SURGERY
Dr. Rocha: One thing we should not forget to mention is that the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is conducive to mixing and matching. I have implanted both the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ and the TECNIS Synergy™ IOL (Johnson & Johnson Vision) in several patients who expressed an interest in customization. The ability to provide J1+ near vision in these patients has led to very positive responses.
Dr. Waring: I have had a handful of patients in my clinic with a TECNIS Symfony™ IOL Legacy in their first eye who received a TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ in their contralateral eye after our clinic participated in a Limited Market Release of the technology. This allowed my practice to gather data on the different dysphotopsias as reported by patients. As expected, eyes with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ had less intense dysphotopsia. Starbursts in particular were notably better in TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ eyes than in TECNIS Symfony™ IOL eyes.
Dr. Micheletti: These data align with my personal experience as well.
Dr. Waring: Risk of developing disruptive dysphotopsia is the primary barrier to adoption of presbyopia-correcting IOLs. Earlier in our discussion, Dr. Micheletti mentioned that patient counseling in the preoperative period is effective at setting expectations. I’d like to know more about how the panel approaches preoperative discussions regarding dysphotopsia.
Dr. Rocha: During my initial consultations with patients who I have deemed good candidates for the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, I illustrate why glare and halos may occur at night. I also explain that contrast under mesopic conditions is usually excellent. So far, patients seem to tolerate the dysphotopsias and are very excited about their evening contrast vision. The improved design of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ plays a role in their satisfaction, of course, but I have found that proper preparation is key to setting expectations.
Dr. Chang: During these counseling sessions, I keep an eye on a patient’s body language. You can often sense whether or not they’re comfortable with the dysphotopsias being described based on how they react.
When it comes to actually explaining which types of dysphotopsias a patient may experience following implantation of any presbyopia-correcting IOL, I remind myself that the person I’m talking to has probably never thought about visual disturbances apart from the cataracts that they may be experiencing. With that in mind, I like to specifically illustrate the types of dysphotopsias that they may experience. For example, when describing dysphotopsias that may occur with night driving, I explain that halos (specifically described as multiple fine rings of light) and starbursts (specifically described as lines of light extending outward) may appear around oncoming headlamps, creating a spiderweb appearance. I don’t rush this portion of the counseling. Additionally, I’ve found that an educational aid, such as a chart illustrating different dysphotopsia patterns (Figure 2) can be helpful.
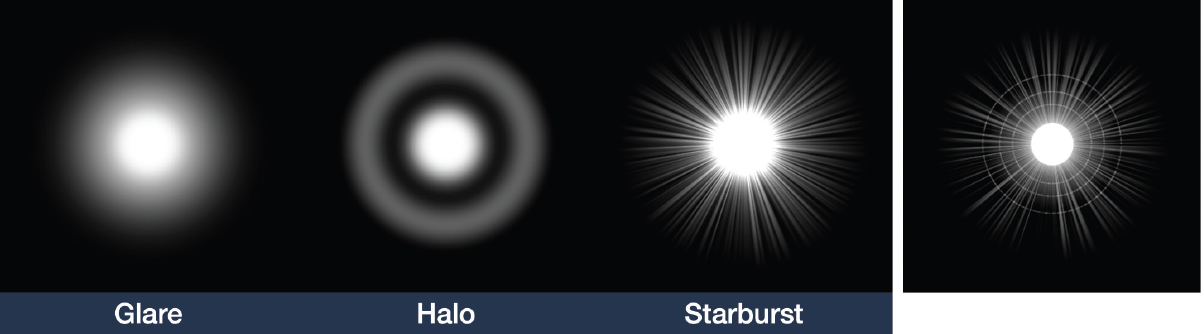
Figure 2. Illustrations of different types of dysphotopsias can prepare patients, especially those who do not appear to have grasped verbal descriptions, for this postoperative phenomenon.
Dr. Waring: Providing patients with language to articulate and identify different types of dysphotopsias in the preoperative period allows them to understand that these occurrences were expected in the postoperative period. How do you interact with patients on postoperative day 1?
Dr. Chang: I agree with your assessment. Patients who know that, say, halos or starbursts have names and are a common occurrence don’t feel as though they’ve experienced a complication. Rather, they feel that their visual function is within the expected range of outcomes. In my conversations with patients on the first day after surgery, I always ask if they saw the halos or starbursts that we discussed before surgery during the previous night. Framing the discussion this way ensures they know that whatever dysphotopsias they’re experiencing are already on my radar.
I insist that patients have enough time to assess their postoperative quality of vision before operating on their second eye. If the patient likes their vision, then the decision is easy: implant the same IOL in the fellow eye. If the patient has concerns with their vision, then I begin weighing which path forward will result in the patient having the highest level of satisfaction.
Dr. Koch: If a patient has 20/25 vision with their cataract, then they are likely already experiencing some glare while driving at night. I use that experience as a point of reference when describing dysphotopsia. In that case, I’ll tell the patient that the glare they see may get a little worse with any of the presbyopia-correcting IOLs on the market, but that their overall sharpness of vision will be much better. Patients with more advanced cataract and vision loss, say to 20/40 or worse, experience worse glare than patients with 20/25 vision. I tell these patients that we can reduce their dysphotopsias and increase their sharpness with a premium lens, or we can really reduce that glare with a monofocal lens. Both options are appealing at that point.
Dr. Chang: For most patients, what they really observe is the change in their visual experience. If they are used to glare and they don’t mind mild or moderate dysphotopsia, then they are unbothered by the possible side effect profile of a presbyopia-correcting lens. If they aren’t experiencing any glare, then the prospect of introducing it may be concerning.
Dr. Waring: Are there any signals a patient may give—whether through body language, verbal cues, or something else—that clearly indicate that they will be dissatisfied with any level of dysphotopsia?
Dr. Koch: I practice in Texas, where many patients have to drive long distances at night to get from here to there. I try to keep it simple with them when it comes to dysphotopsia: if they say that they don’t want any glare at night, then I immediately pivot to explaining how the monofocal IOLs available to them will eliminate any of those concerns. I tell my patients that I have an enhanced monofocal IOL called the TECNIS Eyhance™ (Johnson & Johnson Vision), and that reassures them that monofocal technology is not ‘less than’ other IOL options.
I frame my conversations with patients after surgery similarly to the way Dr. Chang does. I always ask my premium IOL patients to describe their night vision on the day 1 and week 3 visit. I prefer to implant an IOL in the nondominant eye first. Based on my discussions with the patient in the postoperative period, I determine which IOL is the best fit for the contralateral, dominant eye.
Dr. Chang: While I prefer the advantages of operating on the dominant eye first, I have found that the strategy Dr. Koch describes of implanting the nondominant eye first provides an even safer and more conservative approach with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ among patients with particular needs and/or professions. I recently performed cataract surgery on a California Highway Patrol officer who, despite being in his 40s, had moderate bilateral cataracts. Because he rides a motorcycle at night for his profession, he was naturally concerned about dysphotopsias. We planned for him to have the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ implanted in his nondominant eye first so he could assess his satisfaction with nighttime driving. As it turns out, he was quite happy with both the quality of vision as well as the dysphotopsia profile in his first eye, and he soon received a TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ in his fellow eye.
Dr. Koch: Younger patients such as the one Dr. Chang described are typically tolerant of some glare and halo, so I do not worry about implanting a presbyopia-correcting IOL in that population. For that reason, I used to lean toward using the TECNIS Symfony™ IOL in younger patients. Now, with innovations on the TECNIS Symfony™ IOL line playing out in the real world with positive results, I am confident that the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is going to provide someone in their 40s with excellent depth of focus and contrast for decades, while introducing fewer dysphotopsias. For those reasons, it has become a lens of choice for young patients.
Dr. Waring: Dr. Rocha, I understand that you have adjusted your practice pattern regarding dominant/nondominant placement, correct?
Dr. Rocha: That’s right. Innovations in our field have strengthened my confidence that I can start with implanting the dominant eye in a patient to establish distance vision, almost always aiming for plano. I’m implanting most patients with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ now, and I will assess their satisfaction with near vision during follow-up. If they’re readers, for example, then I suggest that we implant a TECNIS Synergy™ IOL in their fellow eye due to its ability to provide excellent near vision.3 But if they’re as happy with their distance and near vision as I expect them to be, then we usually schedule them to receive another TECNIS Symfony™ OptiBlue™ IOL with InteliLight™.
Dr. Waring: The take-home message from this portion of the discussion is that setting expectations and empowering patients to make their own choices are the keys to success. If we tell patients who are implanted with a TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ that small bouts of glare or other dysphotopsias are evidence of the technology providing an enhanced depth of field, then they’ll feel that their postoperative experience is expected. If we don’t prepare them for these visual disruptions, then they’ll be dissatisfied. In short, it’s the difference between a complication and an expectation: the former is an unwanted surprise and the latter is anticipated.
FURTHER SURGICAL CONSIDERATIONS
Dr. Waring: Part of the beauty of the TECNIS Symfony™ IOL platform is its refractive forgiveness. I have found that the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is quite forgiving in terms of refractive target. Has anyone else had that experience?
Dr. Rocha: All cataract surgeons aim to hit the refractive target during surgery. Knowing that patients implanted with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ are able to tolerate some degree of refractive error is comforting in the OR but should not provide so much comfort that we deviate from our standard goal of hitting our target.
Dr. Chang: I like to think of the TECNIS Symfony™ IOL as having one larger target to hit rather than two smaller targets. On top of that, my study showed that patients with TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ needed fewer enhancements than patients with the original TECNIS Symfony™ IOL, even though more TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ patients (19.1% vs 12.7%, P = 0.029) had previous laser vision correction surgery prior to cataract surgery.
To leverage the lens’ tolerance to refractive error in patients with potential variable refractive outcomes, like in patients with previous refractive surgery or variable biometry, a surgeon can aim about 0.5 D plus. This targeting would shift the defocus curve to the left, thus providing more consistent 20/20 distance vision in spite of some shifts in the patient’s refraction. This, of course, comes at the expense of near vision, so appropriate preoperative counseling and expectation setting should take place.
We should note that Johnson & Johnson Vision recommends targeting plano to first minus when first gaining experience with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™.
Dr. Koch: I always set the expectation with my patients that they will need reading glasses for near vision after bilateral implantation of the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™. As long as they know that going into the procedure, they’re comfortable. Fortunately, many in fact have very minimal needs for near correction.
Dr. Rocha: As I said earlier, patients with residual myopia after surgery are likely to experience dysphotopsia. If employing the strategy Dr. Chang describes, I would avoid being too aggressive with that myopic shift.
Dr. Waring: Try as we may, we cannot predict effective lens position, and the result is that patients may end up slightly off target. I have observed that, in patients with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ who are slightly off target, their satisfaction is still high. I am performing fewer enhancements than with traditional bifocal or trifocal technology.
Dr. Grayson: I have found that, in the event that I need to perform an IOL exchange, lenses in the TECNIS® family are easier to explant than other brands. This, too, leads to improved efficiency of a practice. In other lines of IOLs, the haptic design and the adhesiveness of acrylic to the capsule makes exchanges very challenging. While this might not make patients any happier, it certainly provides peace of mind for the surgeon.
Dr. Micheletti: Both patients and surgeons benefit from the refractive forgiveness of TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, which can help to minimize postoperative enhancements. I’ve noticed that they’re also happier about their mesopic vision. In my experience, visual quality in mesopic conditions with TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ is similar to monofocal IOLs. When you consider the exceptional contrast sensitivity we’ve already reviewed, as well as the ‘wow’ factor patients describe regarding their distance vision, it’s understandable why some surgeons consider the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ as their first-line presbyopia-correcting IOL.
Dr. Waring: Cataract surgeons wear many hats: surgeon, physician, engineer, and patient advocate. We’re ultimately in the business of creating the highest level of patient satisfaction possible, and I expect that, as more patients undergo procedures with the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™, we’ll hear positive results. The happiest patients are the ones who don’t return to the clinic beyond the final postoperative follow-up. If the TECNIS Symfony™ OptiBlue™ IOL with InteliLight™ results in fewer returns due to complaints, then we know we’ve selected the right technology for the job.
1. DOF2020CT4011
2. DOF2020OTH4010
3. TECNIS Symfony™ OptiBlue™ IOL with TECNIS Simplicity® Delivery System. DFU Z311558E
4. Holladay JT, Piers PA, Koranyi G, van der Mooren M, Norrby NES. A new intraocular lens design to reduce spherical aberration of pseudophakic eyes. J Refract Surg. 2002;18(6):683-691.
5. van Norren D, van de Kraats J. Spectral transmission of intraocular lenses expressed as a virtual age. Br J Ophthalmol. 2007;91(10):1374-1375.
6. Chang DH, Kao AA, Huggins LK. The effect of violet light filtration and manufacturing improvements on the clinical performance of an extended depth of focus IOL. Paper presented at: American Society of Cataract and Refractive Surgeons annual meeting; April 25, 2022; Washington, D.C.
Johnson & Johnson Surgical Vision, Inc. does not engage in the practice of medicine and any clinical tips within this presentation are not substitutes for appropriate medical education and training or for the exercise of independent medical judgement or review and understanding of the products’ Directions For Use (DFU). Each medical situation should be considered unique to each patient and all treatments individualized accordingly based on the respective physician’s medical judgement. Johnson & Johnson Surgical Vision, Inc. does not (1) warranty the accuracy or completeness of any of the clinical tips, or (2) endorse or recommend any particular technique unless and to the extent such technique is expressly stated in the product labeling.
This promotional education activity is brought to you by Johnson & Johnson Surgical Vision, Inc. and is not certified for continuing medical education. Drs. George Waring, Daniel Chang, Douglas Grayson, Douglas Koch, J. Morgan Micheletti, and Karolinne Rocha are compensated by and presenting on behalf of Johnson & Johnson Surgical Vision, Inc. and must present information in accordance with applicable FDA requirements.
Drs. George Waring, Daniel Chang, Douglas Grayson, Douglas Koch, J. Morgan Micheletti, and Karolinne Rocha are paid consultants of Johnson & Johnson Vision.
INDICATION AND IMPORTANT SAFETY INFORMATION for the TECNIS SYMFONY™ OPTIBLUE™ EXTENDED RANGE OF VISION IOL with TECNIS SIMPLICITY® DELIVERY SYSTEM AND TECNIS SYMFONY™ TORIC II OPTIBLUE™ EXTENDED RANGE OF VISION IOL with TECNIS SIMPLICITY® DELIVERY SYSTEM
Rx Only
INDICATIONS:
The TECNIS Simplicity® Delivery System is used to fold and assist in inserting the TECNIS Symfony™ OptiBlue™ Extended Range of Vision IOL, which is indicated for primary implantation for the visual correction of aphakia, in adult patients, with less than 1 diopter of pre-existing corneal astigmatism, in whom a cataractous lens has been removed. The lens mitigates the effects of presbyopia by providing an extended depth of focus. Compared to an aspheric monofocal IOL, the lens provides improved intermediate and near visual acuity, while maintaining comparable distance visual acuity. The lens is intended for capsular bag placement only. The TECNIS Simplicity® Delivery System is used to fold and assist in inserting the TECNIS Symfony™ Toric II OptiBlue™ Extended Range of Vision IOLs that are indicated for primary implantation for the visual correction of aphakia and for reduction of residual refractive astigmatism in adult patients with greater than or equal to 1 diopter of preoperative corneal astigmatism, in whom a cataractous lens has been removed. The lens mitigates the effects of presbyopia by providing an extended depth of focus. Compared to an aspheric monofocal IOL, the lens provides improved intermediate and near visual acuity, while maintaining comparable distance visual acuity. The lenses are intended for capsular bag placement only.
WARNINGS:
Physicians considering lens implantation under any of the following circumstances should weigh the potential risk/benefit ratio:
1. Patients with any of the following conditions may not be suitable candidates for an intraocular lens because the lens may exacerbate an existing condition, may interfere with diagnosis or treatment of a condition, or may pose an unreasonable risk to the patient’s eyesight:
a) Patients with recurrent severe anterior or posterior segment inflammation or uveitis of unknown etiology, or any disease producing an inflammatory reaction in the eye.
b) Patients in whom the intraocular lens may affect the ability to observe, diagnose or treat posterior segment diseases.
c) Surgical difficulties at the time of cataract extraction, which may increase the potential for complications (e.g., persistent bleeding, significant iris damage, uncontrolled positive pressure or significant vitreous prolapse or loss).
d) A compromised eye due to previous trauma or developmental defects in which appropriate support of the IOL is not possible.
e) Circumstances that would result in damage to the endothelium during implantation.
f) Suspected microbial infection.
g) Patients in whom neither the posterior capsule nor the zonules are intact enough to provide support for the IOL.
h) Children under the age of 2 years are not suitable candidates for intraocular lenses.
i) Congenital bilateral cataracts.
j) Previous history of, or a predisposition to, retinal detachment.
k) Patients with only one good eye with potentially good vision.
l) Medically uncontrollable glaucoma.
m) Corneal endothelial dystrophy.
n) Proliferative diabetic retinopathy.
2. The TECNIS Symfony™ OptiBlue™ IOL should be placed entirely in the capsular bag and should not be placed in the ciliary sulcus.
3. The TECNIS Symfony™ OptiBlue™ IOL may cause a reduction in contrast sensitivity under certain conditions, compared to an aspheric monofocal IOL. The physician should carefully weigh the potential risks and benefits for each patient, and should fully inform the patient of the potential for reduced contrast sensitivity before implanting the lens in patients. Special consideration of potential visual problems should be made before implanting the lens in patients with macular disease, amblyopia, corneal irregularities, or other ocular disease which may cause present or future reduction in acuity or contrast sensitivity, and patients implanted with the lens should be informed to exercise special caution when driving at night or in poor visibility conditions.
4. Some visual effects associated with the TECNIS Symfony™ OptiBlue™ IOL may be expected due to the lens design that delivers elongation of focus. These may include a perception of halos, glare, or starbursts around lights under nighttime conditions. The experience of these phenomena will be bothersome or very bothersome in some people, particularly in low-illumination conditions. On rare occasions, these visual effects may be significant enough that the patient may request removal of the IOL.
5. Patients with a predicted postoperative astigmatism greater than 1.0 diopter may not be suitable candidates for implantation with the TECNIS Symfony™ OptiBlue™ IOL, Model DXR00V, and the TECNIS Symfony™ Toric II OptiBlue™ IOLs, Models DXW150, DXW225, DXW300, and DXW375, as they may not obtain the benefits of reduced spectacle wear or improved intermediate and near vision seen in patients with lower astigmatism.
6. The effectiveness of TECNIS Symfony™ Toric II OptiBlue™ IOLs in reducing postoperative residual astigmatism in patients with preoperative corneal astigmatism < 1.0 diopter has not been demonstrated.
7. Rotation of TECNIS Symfony™ Toric II OptiBlue™ IOLs away from their intended axis can reduce their astigmatic correction. Misalignment greater than 30° may increase postoperative refractive cylinder. If necessary, lens repositioning should occur as early as possible prior to lens encapsulation.
8. Johnson & Johnson Surgical Vision, Inc. IOLs are single-use devices only. Do not reuse this IOL.
9. Do not attempt to disassemble, modify or alter the delivery system or any of its components, as this can significantly affect the function and/or structural integrity of the design.
10. Do not use if the cartridge of the delivery system is cracked or split prior to implantation.
11. Do not implant the lens if the rod tip does not advance the lens or if it is jammed in the delivery system.
12. During initial lens advancement quick advancement of the plunger is needed. Do not stop or reverse while advancing the plunger. Doing so may result in improper folding of the lens.
13. After initial lens advancement and the half turn rotation step, do not move the plunger forward until ready for lens implantation. Doing so may result in the lens being stuck in the cartridge.
14. The lens and delivery system should be discarded if the lens has been folded within the cartridge for more than 10 minutes. Not doing so may result in the lens being stuck in the cartridge.
15. Johnson & Johnson Surgical Vision, Inc. single-use medical devices are labeled with instructions for use and handling to minimize exposure to conditions which may compromise the product, patient, or the user. When used according to the directions for use, the delivery system minimizes the risk of infection and/or inflammation associated with contamination.
16. The reuse/ resterilization /reprocessing of Johnson & Johnson Surgical Vision, Inc. single-use devices may result in physical damage to the medical device, failure of the medical device to perform as intended, and patient illness or injury due to infection, inflammation, and/or illness due to product contamination, transmission of infection, and lack of product sterility.
PRECAUTIONS:
1. This is a single-use device. Do not resterilize the lens or the delivery system. Most sterilizers are not equipped to sterilize the soft acrylic material and the preloaded inserter material without producing undesirable side effects.
2. Do not store the device in direct sunlight or at a temperature under 41°F (5°C) or over 95°F (35°C).
3. Do not autoclave the delivery system.
4. Do not advance the lens unless ready for lens implantation.
5. The contents are sterile unless the package is opened or damaged.
6. The recommended temperature for implanting the lens is at least 63°F (17°C).
7. The use of balanced salt solution or viscoelastics is required when using the delivery system. For optimal performance when using OVD, use the HEALON® family of viscoelastics. The use of balanced salt solution with additives has not been studied for this product.
8. Do not use if the delivery system has been dropped or if any part was inadvertently struck while outside the shipping box. The sterility of the delivery system and/or the lens may have been compromised.
9. Prior to surgery, the surgeon must inform prospective patients of the possible risks and benefits associated with the use of this device and provide a copy of the patient information brochure to the patient.
10. When performing refraction in patients implanted with the TECNIS Symfony™ OptiBlue™ IOL, interpret results with caution when using autorefractors or wavefront aberrometers that utilize infrared light, or when performing a duochrome test. Confirmation of refraction with maximum plus manifest refraction technique is recommended.
11. The ability to perform some eye treatments (e.g., retinal photocoagulation) may be affected by the TECNIS Symfony™ OptiBlue™ IOL optical design.
12. Recent contact lens usage may affect the patient’s refraction; therefore, in contact lens wearers, surgeons should establish corneal stability without contact lenses prior to determining IOL power.
13. The surgeon should target emmetropia as this lens is designed for optimum visual performance when emmetropia is achieved.
14. Care should be taken to achieve IOL centration, as lens decentration may result in a patient experiencing visual disturbances under certain lighting conditions.
15. Do not leave the lens in a folded position more than 10 minutes.
16. When the delivery system is used improperly, the lens may not be delivered properly, (i.e., haptics may be broken). Please refer to the specific instructions for use provided.
17. The safety and effectiveness of TECNIS Symfony™ OptiBlue™ IOLs have not been substantiated in patients with preexisting ocular conditions and intraoperative complications (see below for examples). Careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the benefit/risk ratio before implanting a lens in a patient with one or more of these conditions:
Before Surgery
- Pupil abnormalities
- Prior corneal refractive or intraocular surgery
- Choroidal hemorrhage
- Chronic severe uveitis
- Concomitant severe eye disease
- Extremely shallow anterior chamber
- Medically uncontrolled glaucoma
- Microphthalmos
- Non-age-related cataract
- Proliferative diabetic retinopathy (severe)
- Severe corneal dystrophy
- Severe optic nerve atrophy
- Irregular corneal astigmatism
- Amblyopia
- Macular disease
- Pregnancy
During Surgery
- Excessive vitreous loss
- Non-circular capsulotomy/capsulorhexis
- The presence of radial tears known or suspected at the time of surgery
- Situations in which the integrity of the circular capsulotomy/capsulorhexis cannot be confirmed by direct visualization
- Cataract extraction by techniques other than phacoemulsification or liquefaction
- Capsular rupture
- Significant anterior chamber hyphema
- Uncontrollable positive intraocular pressure
- Zonular damage
18. Carefully remove all viscoelastic and do not over-inflate the capsular bag at the end of the case. Residual viscoelastic and/or overinflation of the capsular bag may allow the lens to rotate, causing misalignment of the TECNIS Symfony™ Toric II OptiBlue™ IOL with the intended axis of placement.
19. The TECNIS® Toric IOL Calculator includes a feature that accounts for posterior corneal astigmatism (PCA). The PCA is based on an algorithm that combines published literature (Koch et.al, 2012) and a retrospective analysis of data from a TECNIS® Toric multi-center clinical study. The PCA algorithm for the selection of appropriate cylinder power and axis of implantation was not assessed in a prospective clinical study and may yield results different from those in the TECNIS® Toric intraocular lens labeling. Please refer to the Johnson & Johnson Surgical Vision, Inc. Toric Calculator user manual for more information.
20. The use of methods other than the TECNIS® Toric Calculator to select cylinder power and appropriate axis of implantation were not assessed in the parent TECNIS® Toric IOL U.S. IDE study and may not yield similar results. Accurate keratometry and biometry, in addition to the use of the TECNIS® Toric Calculator (www.TecnisToricCalc.com), are recommended to achieve optimal visual outcomes for the TECNIS Symfony™ Toric II IOL.
21. All preoperative surgical parameters are important when choosing a TECNIS Symfony™ Toric II OptiBlue™ IOL for implantation, including preoperative keratometric cylinder (magnitude and axis), incision location, surgeons estimated surgically induced astigmatism (SIA) and biometry. Variability in any of the preoperative measurements can influence patient outcomes, and the effectiveness of treating eyes with lower amounts of preoperative corneal astigmatism.
22. All corneal incisions were placed temporally in the parent TECNIS® Toric IOL U.S. IDE study. If the surgeon chooses to place the incision at a different location, outcomes may be different from those obtained in the clinical study for the parent TECNIS® Toric IOL. Note that the TECNIS® Toric Calculator incorporates the surgeon’s estimated SIA and incision location when providing IOL options.
23. Potential adverse effects (e.g., complications) associated with the use of the device include the following:
- Infection (endophthalmitis)
- Hypopyon
- IOL dislocation
- Cystoid macular edema
- Corneal edema
- Pupillary block
- Iritis
- Retinal detachment/tear
- Raised IOP requiring treatment
- Visual symptoms requiring lens removal
- Tilt and decentration requiring repositioning
- Residual refractive error resulting in secondary intervention.
Secondary surgical interventions include, but are not limited to:
- Lens repositioning (due to decentration, rotation, subluxation, etc.)
- Lens replacement
- Vitreous aspirations or iridectomy for pupillary block
- Wound leak repair
- Retinal detachment repair
- Corneal transplant
- Lens replacement due to refractive error
- Unacceptable optical/visual symptoms
- Severe inflammation.
SERIOUS ADVERSE EVENTS
The most frequently reported serious adverse events during the clinical trial of the TECNIS Symfony™ lens were cystoid macular edema (2 eyes, 0.7%) and surgical reintervention (treatment injections for cystoid macular edema and endophthalmitis, 2 eyes, 0.7%). No lens-related adverse events occurred during the trial. Overall, 2.7% (4/148) of TECNIS Symfony™ subjects experienced serious adverse events during the study and 0% (0/148) experienced device-related or unanticipated events.
ATTENTION
Reference the Directions for Use labeling for a complete listing of indications and important safety information.






