Addressing Inefficiency With Automation
Nicole R. Fram, MD

In any industry, automation is only as good as the reliability of the data entered and the potential for increased efficiency. For example, electronic medical records (EMRs) and image management systems can improve access to medical records in real time. This advantage is not realized, however, if the data entered are wrong or images cannot be integrated.
The key to successful automation in ophthalmology is to understand the inefficiencies in day-to-day operations that detract from the practice’s focus on improving patient care and outcomes.
Practices have increasingly more imaging machines that do not necessarily communicate with each other, there are multiple points of potential data entry errors with intraoperative digital devices, and ophthalmologists have a limited ability to analyze outcomes. To address these issues, companies have developed software that can integrate technology irrespective of its manufacturer and serve as a platform for planning surgery and reviewing patient outcomes.
AUTOMATED SOLUTIONS IN PRACTICE
My practice has adopted several automated solutions to improve efficiency. We implemented an automated training system (Alchemy Vision Project) for new staff members. The system provides standardized courses to onboard new employees quickly and efficiently. It also facilitates an assessment of their level of aptitude and highlights where further training is required. We also developed one-click protocols in our EMR system for our most commonly treated conditions. These protocols include checklists for best practices. Additionally, we use an image management system that integrates imaging obtained with all of our devices with the click of a button.
SURGICAL PLANNING AND OUTCOMES ANALYSIS
My practice uses Veracity (Carl Zeiss Meditec) for surgical planning and outcomes analysis. The software integrates imaging machines (biometry, topography, tomography) irrespective of manufacturer, EMR cataract evaluation notes and relevant features, patient responses to a questionnaire that includes key information such as corneal refractive surgery status, latest IOL formulas, and toric IOL and limbal relaxing incision calculators. The software assigns the IOL technology and aim to be selected for various IOL platforms. It also facilitates outcomes analysis after the postoperative refraction is entered to evaluate how well a lens technology is performing and allow optimization.
Before. In the past, I would receive a thick chart that contained printouts from the Lenstar (Haag-Streit) and IOLMaster700 (Carl Zeiss Meditec) biometers, topography, tomography, macular OCT scans, and results with the ASCRS calculator, to name several. If the refractive target was incorrect or changed, I had to ask my staff to print the updated paperwork. I would circle the lens I approved. The surgical scheduler would then type out a sheet that listed the patient’s allergies, the IOL type and power, the patient’s date of birth, and the refractive aim. The process was not ideal in terms of time management and risk of transcription errors, not to mention environmental considerations.
Now. The Veracity system allows us to integrate images and data, pick lenses, automate a surgical schedule, and include special comments with one click and to print it for the day of surgery (Figures 1 and 2). Once the postoperative refractions are performed 2 to 4 weeks after surgery, the EMR note with refraction is added to the system, allowing us to analyze our outcomes and optimize our lenses.
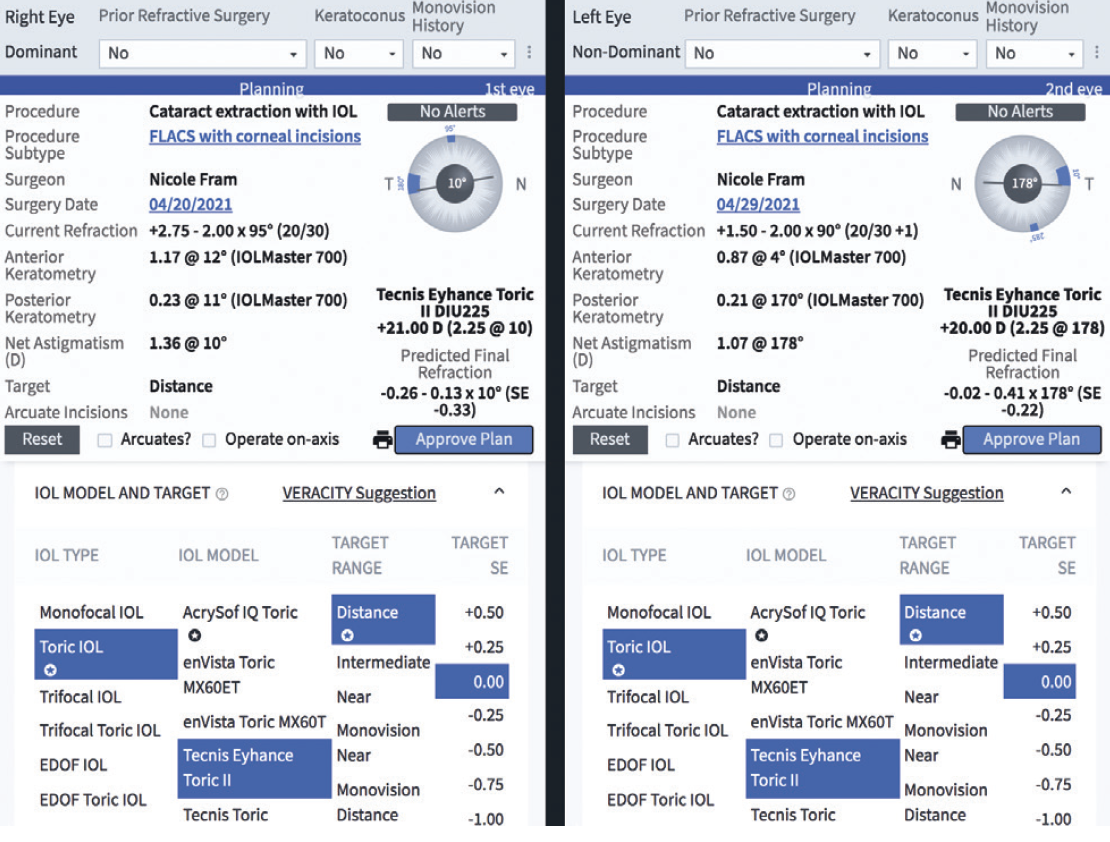
Figure 1. Sample Veracity surgical plan.
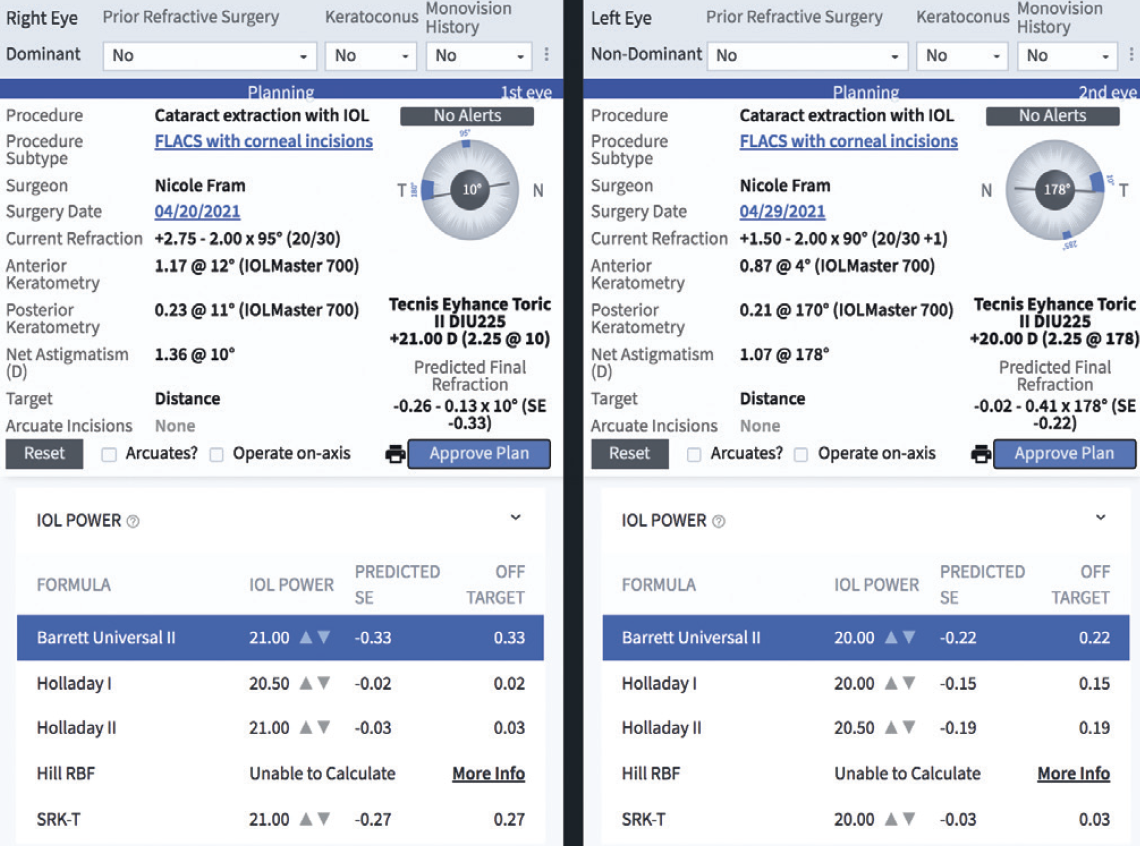
Figure 2. Sample Veracity IOL formula display.
Figures 1 and 2 courtesy of Nicole R. Fram, MD
A Streamlined Approach to Surgical Planning
John A. Hovanesian, MD

Practice automation is a broad term that implies the use of computerized processes to complete tasks that would otherwise be done by a person. Automated solutions generally optimize the accuracy and efficiency of the processes they facilitate, so both patients and practices benefit.
The widespread availability and variety of automated solutions mark the start of the second phase of electronic systems integration in medical practices. The first phase began around 12 years ago with the almost forced adoption of EMRs by medical practices. Many practices resisted, but most gave in to external pressure and transitioned to an EMR system. The initial EMR systems had only basic features and required a significant investment of time and effort to implement while offering little benefit in return.
Government mandates that dictate which functions an EMR system must include have kept the development plates of most EMR companies too full to expand their systems’ functionality. Other companies have stepped in with their own automated solutions for niche needs within a practice or medical specialty. In ophthalmology, automated systems now exist for everything from patient communication to surgical planning and certain aspects of surgery itself. My comments focus on the benefits of leveraging an automated system for cataract surgical planning.
STANDARD APPROACH
Most cataract surgeons still plan their procedures on paper. A printout from a device, typically the biometry unit, presents different IOL power options for a given patient using various IOL formulas. Often, these do not include the most modern formulas. The surgeon circles the appropriate IOL power for the patient, and the printout is transferred to the OR through whatever processes the practice has in place.
The surgical planning process is more complicated for patients with a history of ocular surgery because many surgeons prefer to use advanced IOL formulas that are only available online. The patient’s basic biometry information is entered manually, and transcription or printing of the calculated lens power is required. Either way, there is the potential for transcription errors, and the amount of time required is great.
Studies have demonstrated an error rate of between 1% and 3% when humans transcribe data in a medical environment.1,2 Measures can be taken to mitigate but not eliminate the risk of transcription errors in surgical planning. That’s a real concern because the data affect patients’ vision.
SURGICAL PLANNING
Automated systems provide an opportunity to enhance the accuracy and efficiency of surgical planning. Several software solutions are available to facilitate surgical planning, and each has its own unique features, design, and functionality.
My practice has been using SmartCataract Planner (Alcon) for just over a year. In addition to the benefits of improved efficiency and accuracy, the SmartCataract Planner assists with IOL selection. Because the software is compatible with devices from other manufacturers, it can integrate with existing biometry units to export patient data, apply the intended IOL formulas, output the suggested IOL powers, and share the data with other devices.
The SmartCataract Planner integrates with our EMR system, which allows us to do outcomes analysis (Figure 3). The longer we use the SmartCataract Planner, the more data we will have for this purpose.
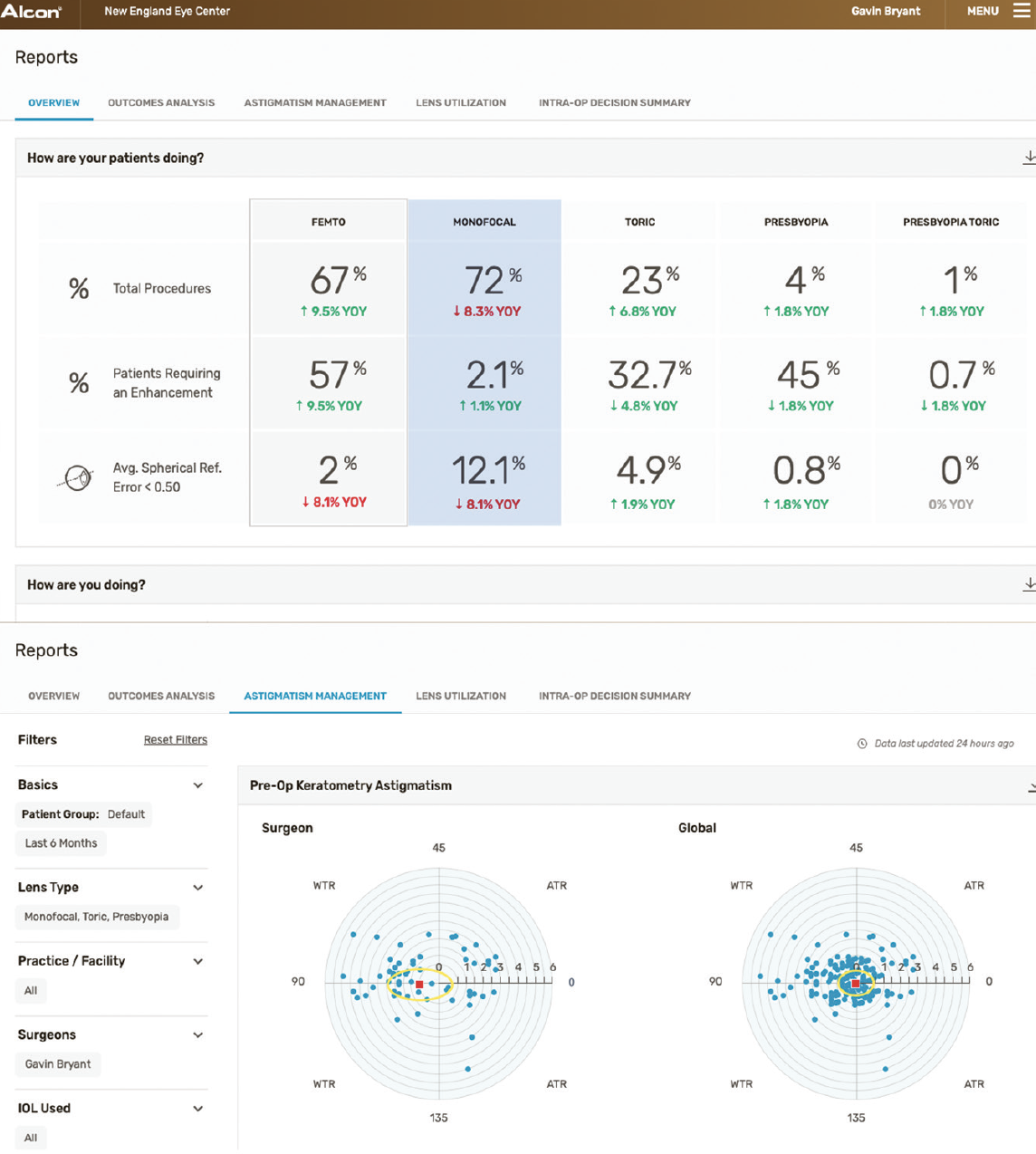
Figure 3. Sample outcome reports with the SmartCataract Planner.
The software facilitates the accurate and efficient transfer of surgical planning data and provides seamless access to the latest IOL formulas (Figure 4). Improved efficiency saves staff time, saves money by reducing the need for expedited shipping of an IOL for a scheduled surgery, and eliminates the risk of manual transcription errors.

Figure 4. The SmartCataract Planner surgical planning interface.
Figures 3 and 4 courtesy of Alcon
CONCLUSION
In the future, further advances in online planning will allow even greater understanding of outcomes and predictive analytics for which patients are most likely to do well with which technologies. Today’s technology is advanced enough that it has already demonstrated its value for saving time, increasing accuracy, and contributing to safer outcomes for our patients.
1. McSwiney RR, Woodrow DA. Types of error within a clinical laboratory. J Med Lab Technol. 1969;26(4):340-346.
2. Tuckerman JF, Henderson AR. The clinical biochemistry laboratory computer system and result entry: validation of analytical results. Comput Methods Programs Biomed. 1985;20(1):103-116.
Bringing Intelligence to Surgical Planning
Mark Lobanoff, MD

For years, I felt that IOL calculations were a major pain point in ophthalmology. In the past, the onerous process of IOL calculation started in my practice with my surgery coordinator. She would gather printouts from the many diagnostic machines used for each patient and manually enter the data into an IOL calculator—a step that was fraught with the possibility of transcription errors. I then received a paper chart with all the printouts, selected an IOL formula, calculated the IOL power, selected a spherical power, and did more data entry. If the IOL was a toric model, I had to log into that manufacturer’s toric IOL calculator and enter the same data again. The process was inefficient and rife with opportunities for error.
To address the inefficiency of traditional surgical planning processes, several companies have developed cloud-based platforms. My company, Lochan, is building one such platform: Eyetelligence (Bausch + Lomb).
THE EYETELLIGENCE PLATFORM
My primary goal is for using Eyetelligence to be effortless. One of my favorite things about the software is that the clinic does not have to change anything in terms of the current patient flow. Patients are refracted, and the data are entered into the EMR system as usual. Patients are examined at diagnostic machines such as the Pentacam (Oculus Optikgeräte), iTrace (Tracey Technologies), or Lenstar. When the exam is complete, the patient is moved to another room. Eyetelligence works in the background through the entire process.
The software creates a record for each patient in the cloud. Data obtained from the EMR system include the diagnosis, allergies, medications, and past surgeries. Data from the diagnostic machines also flow to the cloud, and no effort is required from the technicians or surgeons to make it happen. There is zero chance of a transcription error.
When it comes time to calculate the IOL power for a given patient, Eyetelligence can review the practice’s database to determine which IOL formula is most accurate for eyes with similar features (Figure 5). This capability is unique to Eyetelligence. The IOL calculator also permits the comparison of diagnostic data taken from two different biometers. Eyetelligence has an app for smartphones using the Android or Apple operating system. The app can be used to access data from the platform and confirm the patient’s identity and IOL selected. This can help to avoid the wrong eye, wrong patient mistake (Figure 6).
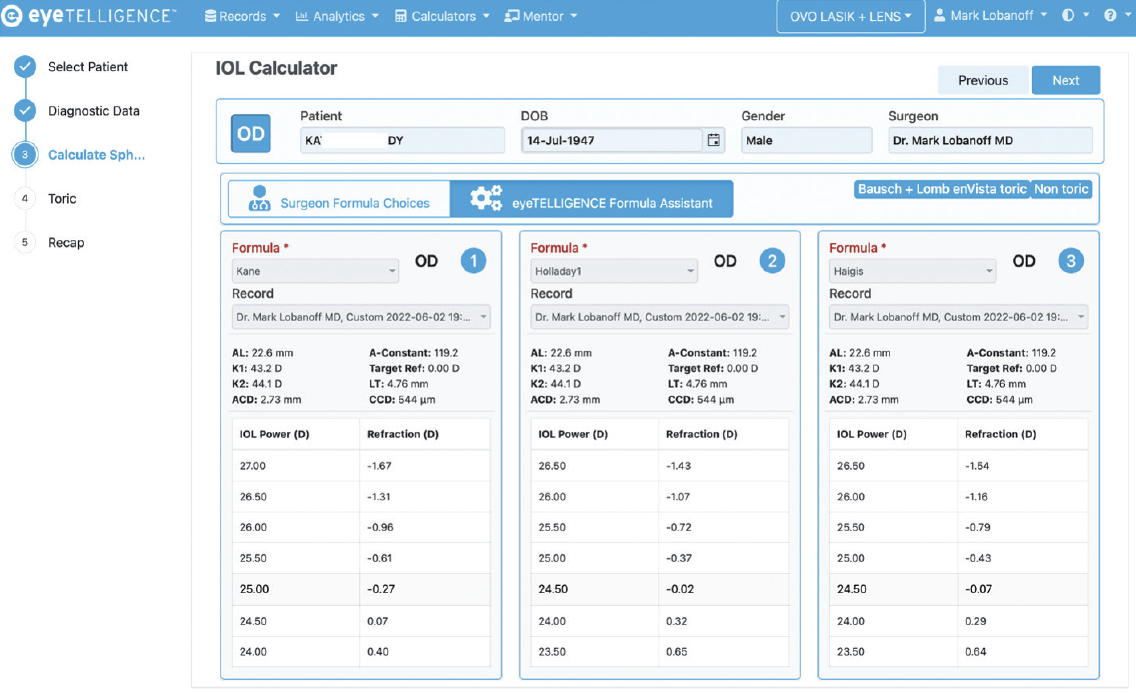
Figure 5. The Eyetelligence formula assistant provides a ranked list of IOL formula recommendations based on which should give the best outcome based on the eye’s unique physical characteristics.
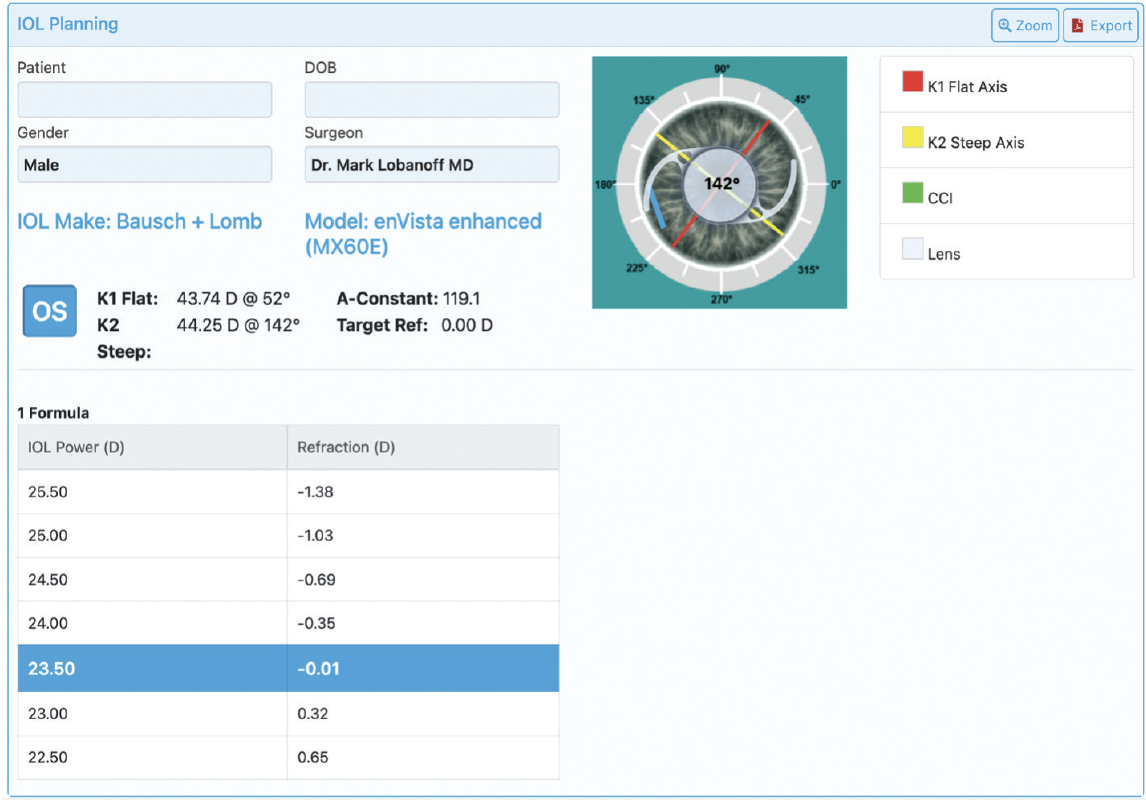
Figure 6. Sample Eyetelligence surgical plan, which can be displayed on the phone app or a monitor in the OR.
Every surgeon has their own landing page on the Eyetelligence platform (Figure 7). From it, they can navigate to patient information and view task prompts that highlight which cases lack IOL calculations or the OR schedule.
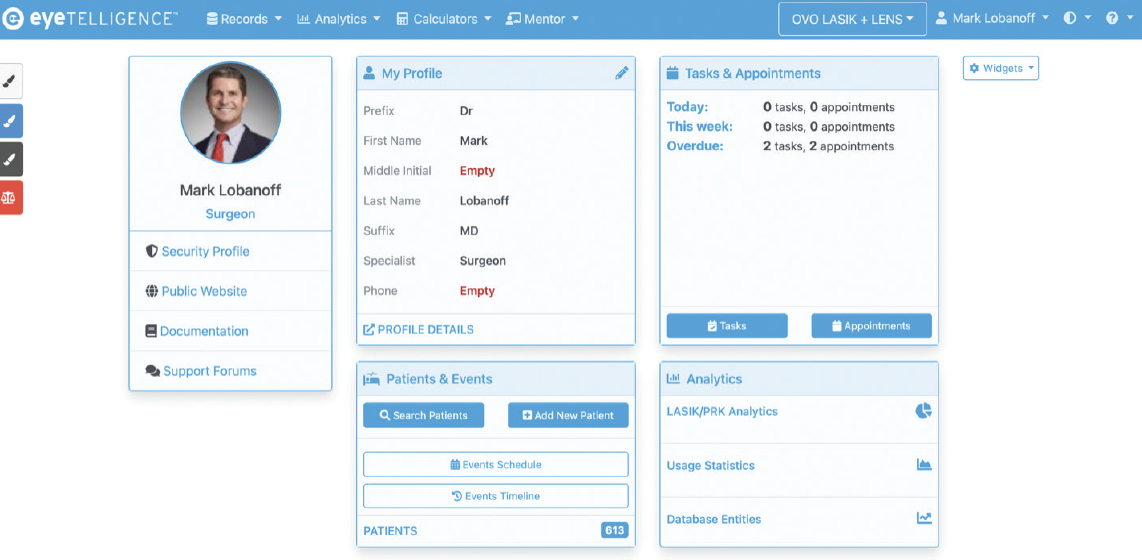
Figure 7. A surgeon landing page on the Eyetelligence platform.
Figures 5–7 courtesy of Mark Lobanoff, MD
CONCLUSION
The Eyetelligence platform is being designed from the ground up to make cataract and IOL surgery more efficient, accurate, and safe.