There is a wide variety of surgical treatments for presbyopia that target correction at the lens, the cornea, or the sclera. Most lens-based procedures involve removing the crystalline lens and replacing it with bifocal, trifocal, accommodating, or extended depth of focus (EDOF) IOLs. Lens-based solutions are appropriate for patients who are in dysfunctional lens syndrome (DLS) stages 2 and 3: that is, those who present with moderate to severe cataracts.
Cornea-based solutions include laser refractive surgery, intrastromal treatments, and corneal inlays, and they can be options for patients who experience the symptoms of presbyopia but still have a relatively clear lens (DLS stage 1).
Patients in DLS stage 1 are also candidates for sclera-based solutions, which today include implants and laser scleral microporation (LSM). This article discusses these procedures and briefly reviews the history behind sclera-based solutions.
HISTORY OF SCLERA-BASED SOLUTIONS
Sclera-based solutions for presbyopia are unique among these three broad categories, in that they attempt to address the biomechanical dysfunction associated with presbyopia rather than manipulating the optics of the cornea or the lens.
Thornton pioneered sclera-based solutions with anterior ciliary sclerotomy (ACS).1 In ACS, radial incisions were made in the sclera, over the ciliary muscles, in an attempt to increase the space between the lens and the ciliary muscles, tighten the zonules, and improve accommodative ability. Initially, improvement in accommodative amplitude of 2.20 D on average was observed, but this regressed to approximately 0.80 D over 12 months postoperative, primarily due to wound healing.2 Fukasaku devised a modified ACS treatment using silicone implants to reduce the regression; however, this procedure was not well received. Both the ACS procedure and Fukasaku’s modification are no longer performed.
SCLERAL IMPLANTS
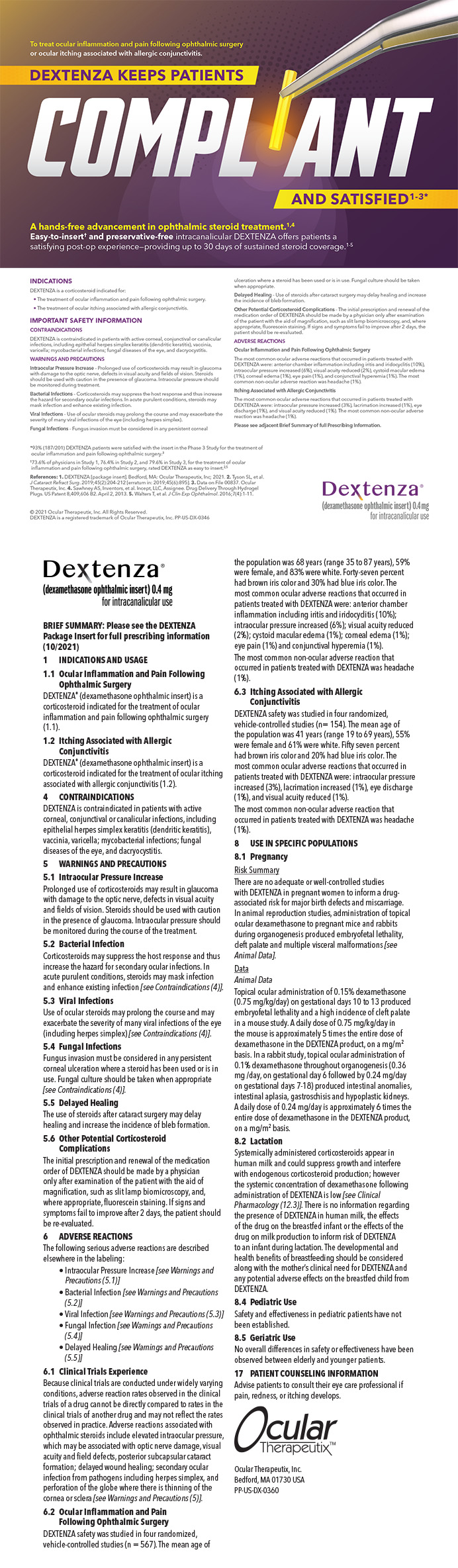
As with ACS, the rationale for scleral implants is based on the accommodation model of Schachar and colleagues, who described a decrease in the space between the ciliary ring and the lens as the cause of presbyopia.3 The only scleral implant currently with the CE Mark is the VisAbility Micro Insert System (Refocus Group). This device is limited to investigational use in the United States. In this procedure, patients are placed under monitored anesthesia care for approximately 1 hour while the device is implanted bilaterally. Four PMMA implants are placed in four oblique quadrants of each eye, 3 to 4 mm from the limbus and approximately 0.4 mm deep in the sclera (Figure 1).4
Figure 1. Implantation of the VisAbility Micro Insert.
In January, results of a 360-patient FDA clinical trial with the device were posted on clinicaltrials.gov.5 In this trial, patients at 14 sites received VisAbility Micro Inserts in their first eye, then in their second eye no sooner than 14 days later. All patients were followed for 24 months. At that endpoint, patients showed improvement in near visual acuity. Of patients included in the analysis, 84% (289 of 344) had a distance-corrected near visual acuity (DCNVA) in the primary eye of 20/40 or better and a gain of at least 10 letters.
A randomized substudy of 60 patients at three sites compared the DCNVA of patients who received the implants with control patients who had their implantations deferred for 6 months. A higher percentage of patients who received the implants (18 of 28, 64%) versus the control group (2 of 29, 7%) had DCNVA of 20/40 or better and a gain of 10 letters in their primary eye. These results have not been published, and therefore no explanation has been proposed for the change in the control group.
The efficacy results with these scleral implants are encouraging; however, their safety remains under investigation. There is risk for anterior segment ischemia (ASI) from mechanical vascular compression of the implants on surrounding blood vessels. Earlier versions of these implants were also at risk for movement or displacement. An ongoing 5-year follow-up clinical trial investigating the long-term safety of the VisAbility Micro Insert System will assess safety endpoints including ASI, segment exposure from scleral or conjunctival erosion, and adverse events.6
LASER SCLERAL MICROPORATION
The LSM procedure, not currently available in the United States, is not based on the Schachar theory of accommodation. Rather, it is based on the VisioDynamics Theory, the proposition that age-related changes in connective tissue result in crosslinking and loss of pliability of these tissues in the eye—similar to the effects of aging on connective tissue in other parts of the body.7,8 In addition to the lens, extralenticular factors such as the ciliary muscle, zonules, choroid, and sclera are affected by increasing age and are implicated in influencing the progression of presbyopia.9,10
The LSM procedure is designed to reduce ocular rigidity that occurs progressively with age by uncrosslinking collagen and elastin fibrils in the sclera. LSM aims to restore the mechanical efficiency of the natural accommodative forces by creating regions of biomechanical pliability. This is accomplished through the creation of a micropore matrix in the sclera.11
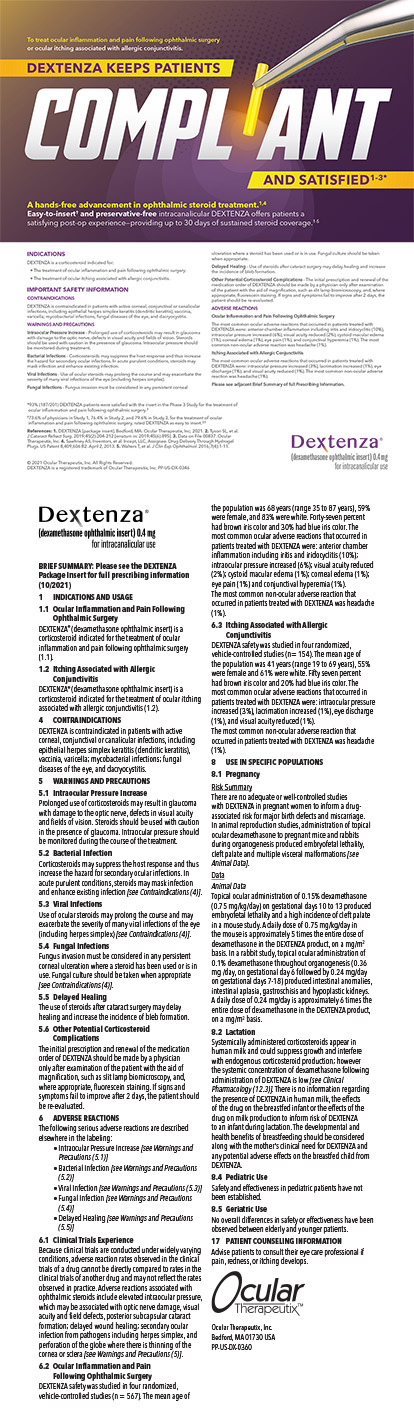
Data from an Institutional Review Board–registered Taiwan FDA clinical trial of LSM were published in 2017.11 In that trial, a handheld Er:YAG laser with a wavelength of 2.94 μm (VisioLite, Ace Vision Group) was used to create, within a 5 x 5 mm matrix in each of four oblique quadrants of the sclera overlying the ciliary muscles, nine 600-µm pores, 0.5 mm from the limbus, to a depth of up to 80% of the sclera (Figure 2).

Figure 2. The LSM procedure performed with the VisioLite device. Reprinted with permission from Hipsley et al.11
In the study, 52 eyes of 26 patients underwent the LSM procedure. Patients demonstrated improvements in both intermediate and near visual acuity while their distance visual acuity remained stable. At 24 months postoperative, 83% of patients had binocular DCNVA of 20/32 or better. Patients also self-reported high postoperative satisfaction.
The latest generation of the LSM procedure uses a semi-automated handheld Er:YAG laser with a wavelength of 2.94 μm (VisioLite Gen I MP, Ace Vision Group) to create more pores (42–49) with a smaller spot size (225 µm), again in a 5 x 5 mm matrix in four oblique quadrants in the sclera overlying the ciliary muscles, to a depth of up to 80% of the sclera (Figure 3).
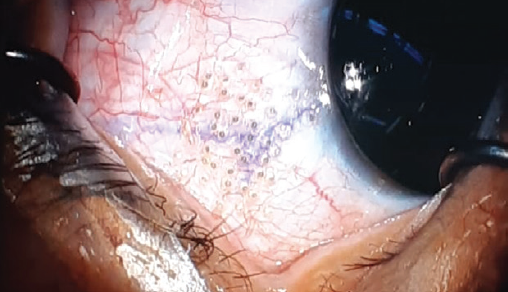
Figure 3. The LSM procedure performed with the VisioLite Gen I MP device.
Data from a pilot study using this procedure, including 10 eyes of five patients, were presented in 2018.12 At 1 month postoperative, patients demonstrated a gain of up to 8 lines in uncorrected near and intermediate visual acuity (median, 4.5 lines). Uncorrected distance visual acuity remained stable. Additionally, 100% of patients had binocular uncorrected near visual acuity of 20/40 or better.
CONCLUSION
Sclera-based solutions to the aging lens and presbyopia are biomechanical treatments or therapies rather than corrective procedures, as they aim to improve biomechanics without performing an optical treatment. Sclera-based procedures do not involve the visual axis, and they appear to restore near and intermediate visual acuity without affecting distance visual acuity. They have the potential to be good treatment alternatives for young presbyopes without cataract.
LSM is a therapeutic procedure that has exciting preliminary results and, thus far, has demonstrated good safety and efficacy in clinical studies outside the United States.
1. Thornton SP. Anterior ciliary sclerectomy (ACS), a procedure to reverse presbyopia. In: Sher NA, ed. Surgery for Hyperopia and Presbyopia. Philadelphia: Williams & Wilkins; 1997.
2. Fukasaku H, Marron JA. Anterior ciliary sclerotomy with silicone expansion plug implantation: effect on presbyopia and intraocular pressure. Int Ophthalmol Clin. 2001;41(2):133-141.
3. Schachar RA. Cause and treatment of presbyopia with a method for increasing the amplitude of accommodation. Ann Ophthalmol. 1992;24(12):445-445.
4. Davidson RS, Dhaliwal D, Hamilton DR, et al. Surgical correction of presbyopia. J Cataract Refract Surg. 2016;42(6):920-930.
5. A clinical trial of the VisAbility Micro Insert System for presbyopic patients. NCT02374671. https://clinicaltrials.gov/ct2/show/NCT02374671. Accessed January 30, 2020.
6. Long term follow-up of the VisAbility Micro Insert System for presbyopic patients. NCT03811249. https://clinicaltrials.gov/ct2/show/NCT03811249. Accessed January 30, 2020.
7. Hipsley A, Dementiev D. The LaserAce procedure: A revolutionary surgical approach for restoring accommodation in the aging eye. In: Ashok G, ed. Jaypee’s Video Atlas of Ophthalmic Surgery: Jaypee Brothers; 2009.
8. Pallikaris IG, Kymionis GD, Ginis HS, Kounis GA, Tsilimbaris MK. Ocular rigidity in living human eyes. Invest Ophthalmol Vis Sci. 2005;46(2):409-414.
9. Croft MA, Nork TM, McDonald JP, Katz A, Lutjen-Drecoll E, Kaufman PL. Accommodative movements of the vitreous membrane, choroid, and sclera in young and presbyopic human and nonhuman primate eyes. Invest Ophthalmol Vis Sci. 2013;54(7):5049-5058.
10. Croft MA, McDonald JP, Katz A, Lin TL, Lutjen-Drecoll E, Kaufman PL. Extralenticular and lenticular aspects of accommodation and presbyopia in human versus monkey eyes. Invest Ophthalmol Vis Sci. 2013;54(7):5035-5048.
11. Hipsley A, Ma DH-K, Sun C-C, Jackson MA, Goldberg D, Hall B. Visual outcomes 24 months after LaserACE. Eye Vis. 2017;4:15.
12. Shah S, Jackson MA, Hipsley A, Ang RT, Hsiao E. Functional visual outcomes and biomechanical changes after a new presbyopia therapy: laser scleral microporation. ASCRS ASOA Annual Meeting; April 13-17, 2018; Washington, DC.