Case Presentation
A 53-year-old woman presents for a consultation. The patient underwent bilateral radial keratotomy (RK) for myopia 28 years ago. She reports a growing dependence on reading glasses during the past 15 years, increasing dependence on spectacle correction for distance during the past 5 years, and diurnal fluctuations in her vision.
How would you proceed?
—Case prepared by Allon Barsam, MD, FRCOphth
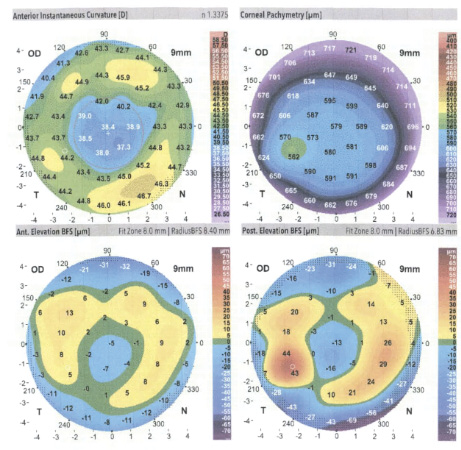
Figure 1. Corneal tomography of the patient’s right eye.
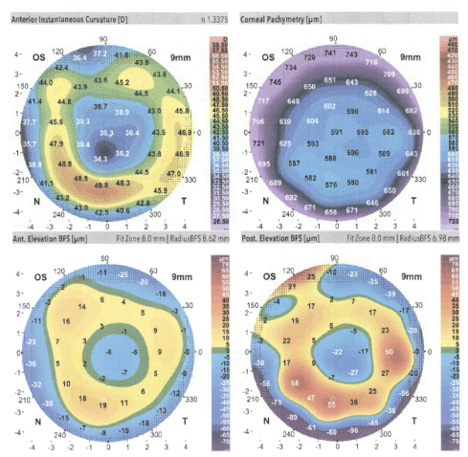
Figure 2. Corneal tomography of the patient’s left eye.


HERCULES LOGOTHETIS, MD; AND SHAMIK BAFNA, MD
The key to this case is the diurnal fluctuations in vision. A variable refraction automatically changes the paradigm of how to improve this patient’s vision for the long term. The first step is to stabilize the cornea with CXL.1 It will be important to explain to her that she may experience a hyperopic shift of 1.50 D after CXL that can be addressed at a later date.1
At our clinic, we have had great success with epithelium-on CXL (an off-label procedure), both objectively and in terms of patients’ level of comfort. We would wait 6 months after bilateral CXL before assessing the stability of the manifest refraction. Once stability was confirmed, the ideal strategy would avoid further corneal surgery in favor of a lens-based approach.
Given the patient’s history of RK, this would be a perfect opportunity to consider employing some new technologies. Debate continues regarding bilateral versus unilateral implantation of an IC-8 lens (AcuFocus, not approved by the FDA). We would implant this lens in the patient’s nondominant eye in order to minimize preexisting corneal aberrations and take advantage of the depth of focus provided by this IOL’s pinhole optic design. For the dominant eye, we would consider placing either a Light Adjustable Lens (RxLAL, RxSight) for distance or an IC-8 lens. The RxLAL would allow us to maximize UDVA in the dominant eye and preserve as much optical quality as possible. (Editor’s note: For more on treating post-RK patients, see “Arrrrrgh K: How Do We Best Care for Post-RK Patients?” on page 61.)
Overall, the goals are to stabilize the cornea and then maximize optical quality and spectacle independence through IOL selection.

KEITH A. WALTER, MD, FACS
In my experience, RK patients adapt well to fluctuating vision and nighttime glare. This patient, however, has excellent BCVA but is now totally dependent on glasses for both near and distance. If no cataracts are present, fitting her with scleral contact lenses may provide her with excellent distance visual acuity and ocular comfort despite extremely flat central keratometry readings. This strategy would, of course, require her to wear reading glasses for near tasks.
In my opinion, this patient is not a candidate for further surface refractive surgery, but the option of a refractive lens exchange for a Tecnis Symfony IOL (Johnson & Johnson Vision) in each eye could be considered. I would use a keratometry reading that was an average of measurements taken in the morning and night and calculate IOL power using the ASCRS online formula for prior RK (iolcalc.ascrs.org). I have achieved outstanding results using this strategy for cataract patients with a history of RK; most of them have not required glasses to see at near or distance after surgery.

WHAT I DID: ALLON BARSAM, MA, MBBS, FRCOphth
I performed a refractive lens exchange on the patient’s nondominant eye and implanted an IC-8 IOL. To calculate IOL power, I used the ASCRS online formula for prior RK. I placed all incisions between and posterior to the previous RK incisions, with the main incision located closest to the steep corneal axis. After surgery, UDVA was 20/20 (6/6), and uncorrected near visual acuity was N6 (J2).
After confirming that the patient was not experiencing dysphotopsia, I performed the same procedure on her dominant eye and achieved a similar outcome. UCVA at all distances and her quality of vision improved, and diurnal fluctuations completely resolved.
1. Bafna S, Wiley W, Trattler W. Refractive effect of corneal CXL in post-radial keratotomy patients. Poster presented at: ASCRS Congress & Symposium; April 9-14, 2019; San Francisco.




