
The stalwart friendship and sharing of knowledge among medical colleagues has a deeper meaning than simply the act of patient referral. The Greek philosopher Aristotle recognized the power of collaboration and spoke of it often in his works, as in this example:
Whatever ‘to be’ means for each type of men, whatever it is for whose sake they value life, in that they wish to occupy themselves with their friends; and so some drink together, others dice together, others join in athletic exercises and hunt together, or philosophize together, each type spending their days together in whatever they love most in life; for since they wish to live with their friends, they do and share in those things which they count as living together. … while the friendship of the good is good, being augmented by their companionship; and they are thought to become better too by being active and by improving each other.1
AT A GLANCE
- Current trends dictate that the number of ophthalmologists will not grow, as future attrition is likely to exceed the number of new entrants into the field.
- With regard to patient education of laser cataract surgery and other trending technologies, optometrists are in prime position to address perioperative issues that include dispelling myths, setting appropriate levels of expectation, and answering questions about the experience and qualifications of the ophthalmologist to whom he or she is referred.
- Optometrists should have a deep understanding of the laser cataract surgery procedure itself and of the available technologies, so they can be on the front lines of patient education.
These principles he mentions, of “companionship” and “improving each other,” can at times be lost during our busy lives in the practice and the surgery center. Nonetheless, these seminal concepts define the relationship between optometrists and ophthalmologists, especially for patients embarking upon the cataract surgery experience.
The optometrist begins the educational process for these patients, relaying the treatment and management options, including laser cataract surgery. This then allows the ophthalmologist to continue the consultative dialogue. After the optometrist has set the table, the surgeon can serve up a shared vision of what the surgical outcome and goals might be for the patient.
Although I describe this interprofessional symbiosis with ease, it can be a challenge to realize. There are multiple moving parts and gears that can facilitate a more efficient relationship. The coming generation of optometrists is acutely aware that surgical and medical collaboration will be an increasing part of their practices. They want to embrace this role and become an extension of surgical eye care services.
MIRROR, MIRROR
It is no secret that the gerontification of the baby boomer generation will weigh increasingly heavily on our health care system. The 65-and-older population is growing at four to five times the rate of the overall population.2 At the same time, there is a convergence of eye care service needs, as this aging demographic group will be more susceptible to age-related disease states such as cataracts, macular degeneration, and glaucoma.
Furthermore, we cannot expect the number of ophthalmologists to grow to manage this increased caseload. Current trends dictate that the number of ophthalmologists and other surgical specialists will not grow, as future attrition is likely to exceed the number of new entrants into these fields. The Association of American Medical Colleges has forecast that there could be a shortfall of as many as 33,200 physicians by 2025 (Figures 1 and 2).2
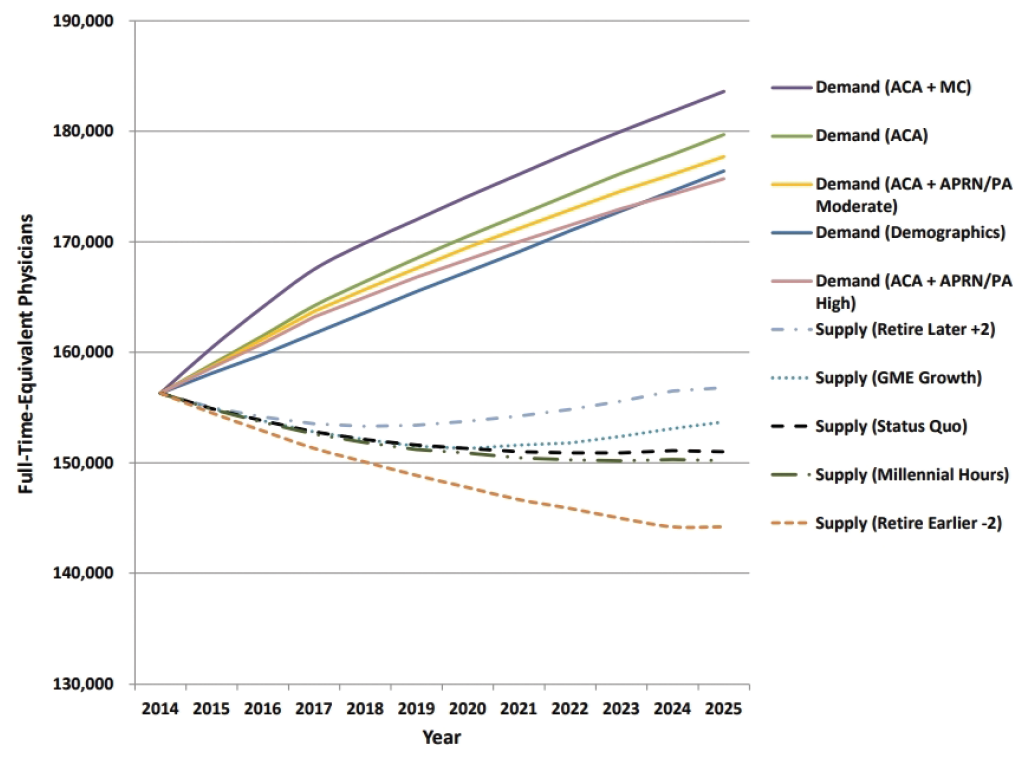
Figure 1. Projected supply and demand for surgeons, 2014 to 2025.
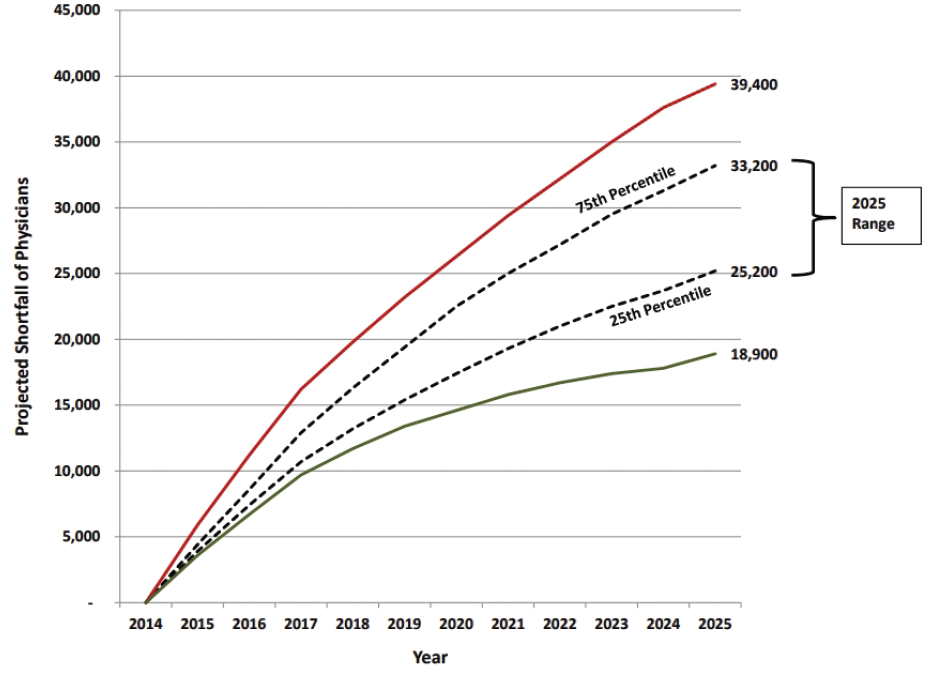
Figure 2. Projected surgical physician shortfall range, 2014 to 2025.
How will these changes translate to patient care? On the surface, it is an opportunity to hone the aforementioned interprofessional cataract surgery collaboration. In reality though, it is also a call for optometrists to broaden the responsibilities we share with our surgical colleagues, from pre- and postoperative care to assisting in the OR during laser cataract surgery. Some of our peers already are performing these roles, although participation in such responsibilities must be based on the comfort level of the eye care provider.
THE HUMAN ADVENTURE
As primary eye care providers, optometrists have often seen cataract patients for most of their lives prior to referring them for surgery. When questions arise regarding the options available, they pick up the phone, text, or email us for advice. In my experience, many patients feel more comfortable about surgery after they share their concerns with me to ensure they are making the right choice. From the layperson’s perspective, the decision to have any surgery is intimidaing.
Our job is to act as a safety valve, especially in light of recent health care pressures and the advent of trending technologies such as laser cataract surgery and adjustable IOLs. Additionally, patients may have questions about the level of experience and qualifications of the ophthalmologist we will be referring them to. We are here to dispel myths and, more important, to set appropriate levels of expectation. Optometrists are in prime position to address all of these perioperative issues.
STEPPING FORWARD EDUCATIONALLY
In order to walk the walk, our practice provides periodic in-house education to staff members and to the local optometric community. Some community optometrists may have formed less-than-favorable opinions regarding premium IOLs and laser cataract surgery based on earlier technology platforms or a cost-conscious perspective. Inviting these eye care providers into our clinics and surgery centers and offering our peer-to-peer guidance allows them to better appreciate the screening procedures and the work that goes into providing premium surgical outcomes. Putting in these extra outreach efforts can pay dividends in working relationships for the surgeon.
After the optometrist lays out the options, the cataract patient deserves a meeting with the surgeon to hear his or her opinions and recommendations. For our patient education, we use commercially available animations that illustrate, for example, how the lens optics of extended depth of focus IOLs function. We also have video testimonials on tablet computers featuring patients describing different stages of their journeys.
EMISSARIES
Cataract patients often have comorbidities such as ocular surface challenges or a glaucomatous condition that may either delay or accelerate the need for surgery. These complexities can complicate the decision-making process, and it may require more hand-holding and chair time.
To motivate patients to make these daunting decisions, we must demonstrate that we all believe in the ability of these advanced technologies to enhance their lives. This belief must emanate directly from all sources, from all personnel, so that patients are inspired to buy into the process. We must also convey the reality that these optical systems have nuances that may take time for patients to adapt to, retraining the brain in their new visual environment.
Optometrists are the patients’ support beams in the pre- and postoperative periods, but our team of technicians is a further buttress, fielding any questions or concerns that may arise. They can provide help with medication prior authorizations and general therapeutic dosing questions. These individuals have a deep understanding of the technologies we offer and the cataract procedure itself, so they can be on the front lines of patient education regarding laser cataract surgery. They are unsung heroes who bind us all together, and they should be recognized for their unwavering commitment to the process.
WHAT IS THE KOBAYASHI MARU?
In the fictional Star Trek universe, the Kobayashi Maru was a training exercise designed to test the characters of Starfleet Academy cadets. This no-win test was depicted in the opening scene of Star Trek II: The Wrath of Khan and in the 2009 film Star Trek.
THE KOBAYASHI MARU SOLVED
Surgical success is measured by patient happiness. Innovative practices will embrace evolving technologies and will promote collaborative care to deliver cataract surgery, whether laser or conventional, and other services effectively and efficiently. Today’s optometrists share the surgeon’s vision and are at their service.
1. Hitz Z. Aristotle on self-knowledge and friendship. Philosophers’ Imprint. 2011;11(12):1-28.
2. The complexities of physician supply and demand: projections from 2014 to 2025: 2016 update. Association of American Medical Colleges. April 5, 2016. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Accessed January 5, 2018.




