
I ALWAYS USE FEMTO
Why my center is 100% laser cataract surgery.
By Sheraz M. Daya, MD, FACP, FACS, FRCS(Ed), FRCOphth
We introduced the »Victus Femtosecond Laser platform (Bausch + Lomb) to our practice in 2012 and decided at the outset that we would perform laser lens surgery on all patients undergoing cataract or refractive lens exchange (RLE). We did not know if the laser procedure was going to be better than the standard approach, but we felt that, as a premium private provider with a greater than 95% premium lens implant rate, we could not rationalize or justify differentiating surgery options based on upselling the laser. Our goals have always been to provide the best possible outcomes to patients and to do whatever it takes to provide good vision and depth of focus.
Having experienced a similar issue with the introduction of the IntraLase femtosecond laser (now »iFS; Johnson & Johnson Vision) for LASIK in 2004, we decided to follow a similar process. We increased the overall price of the procedure—in this case cataract surgery or RLE—by a small amount (£450) and now provide laser lens surgery as a standard for everyone. We inform patients that we perform refractive and premium surgery on all patients, no matter their age, with the aims of reducing dependence on spectacles and fulfilling the goals of those who come to see us in trust looking for maximal freedom from spectacles.
The package also includes treatment of astigmatism up to 1.50 D at no additional cost. We would not be able to provide patients with a good outcome without treating astigmatism of 0.75 D or greater, and, as there is no additional cost to us besides a bit of time marking the cornea and a few seconds more on the laser, we could not justify increasing the cost to the patient for this service.
KEY FINDINGS
What have we found after more than 5 years and more than 3,000 cases of Victus-assisted lens surgery? (I differentiate the Victus-assisted procedure from the generic laser cataract surgery, as I know from experience that the available lasers behave differently, with differing rates of complications.)
Here are our key findings:
No. 1: Almost identical visual outcomes. Visual outcomes compared with manual phacoemulsification surgery are almost identical, with no statistically significant advantage.
No. 2: Reduced enhancement rates. Enhancement rates using photorefractive ablative surgery were reduced from about 3% to less than 1% with the laser.
No. 3: Reduction in some associated surgical side effects. There has been a dramatic reduction in clinically significant cystoid macular edema. We used to have a case, often bilateral, every 6 to 8 weeks, and now we hardly ever see a case.
No. 4: The same procedural time. Throughput of surgery remained the same, at three to four cases per hour, using one OR with the laser in the room and operating on the laser bed (Figure 1).

Figure 1. Dr. Daya performs lens surgery on the femtosecond laser bed.
No. 5: Less stressful surgery. I used to go home feeling exhausted after a day of surgery and dying for a glass or two of wine. After incorporation of the Victus, this is no longer the case. It is interesting how reliable reproducibility led to less stressful surgery; there was a similar finding when we introduced IntraLase to our practice. (Perhaps I shall live longer!)
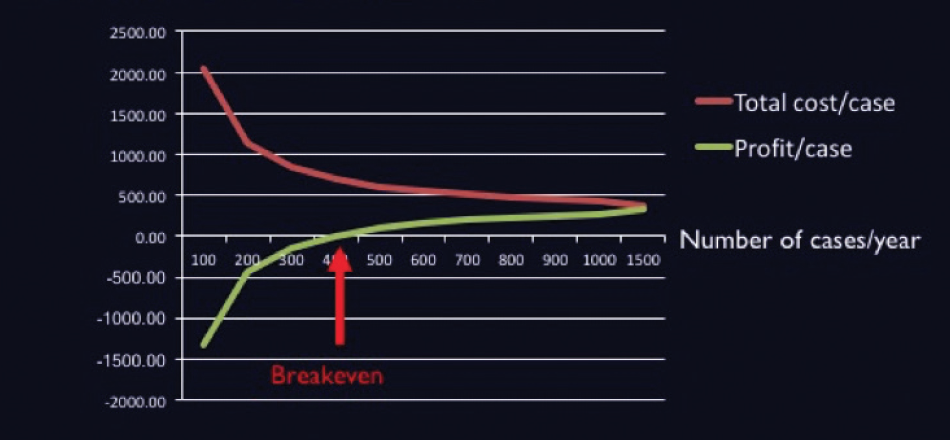
No. 6: From an economic standpoint, we became more profitable. Although our fixed costs increased from 36% to 37% in the year we adopted the technology, surgical volume increased by 15%, and profit increased by 10%. The break-even point based on current pricing is about 400 cases per year per laser with a price increase of £450 per lens surgery case (see Price Point below).
Price Point
Assuming the femtosecond laser costs €400,000 and with a £450 increase in the cost of laser cataract surgery, the break-even point at Dr. Daya’s clinic is about 400 cases per year per laser.
CONCLUSION
For a variety of reasons, performing laser lens surgery made sense for our practice. First, we demonstrated to patients that we are truly a premium provider by adopting what we believe to be a better and more reliable technology as standard for all. Second, this enabled us to concentrate on dealing with our patients and their goals for vision correction without confusing them with a menu of options and pricing.
There is only so much information patients can digest at consultation. It is best to concentrate on medically related issues, especially when it comes to complex options such as trifocal IOLs. Patients need time to understand the concept of neural adaptation for near vision and halos. Taking the time to explain these concepts, I believe, helps to ensure greater satisfaction and less trouble postoperatively. Why distract patients by trying to up-sell for a few hundred pounds, only to have them haunt you afterward because they did not digest the issues about adaptation and the need for time? And why jeopardize patient trust by bringing up an extensive menu of value options and providing choices?
If you know the numbers of patients undergoing surgery per year in your practice, reliable costing of surgery is possible, and a reasonable return on investment can be achieved. The best returns on that investment, however, are consistency of results, simplicity of surgery, and the happiness of your patients.

I Use Femto in Certain Cases
In some instances, the technology could make a difference in one’s ability to perform surgery.
By Harvey Reiser, MD
Femtosecond laser technology has been an important step forward, another incremental advance in the continuing evolution of cataract surgery. Although for some cases it may not seem to make a big difference in one’s ability to perform the surgery, in others I believe it can make a significant difference.
I have used the »LenSx Laser (Alcon) for approximately 5 years, and I currently do about 50% of my cases with the laser. The advantages I see are the laser’s ability to create a consistent and reproducible anterior capsulotomy and to fragment the nucleus. Less crucial but also helpful are the placement of the primary and secondary incisions and the creation of astigmatic corneal relaxing incisions.
ADVANTAGES
In my opinion, the biggest advantages of the femtosecond laser are most notably the capsulotomy and fragmentation steps, and these advantages are most helpful in potentially challenging cases. For example, in eyes with psedoexfoliation or those with zonular instability, having a complete capsulotomy that is large enough to allow the case to proceed with minimal nuclear manipulation is a huge benefit. With that step and nuclear fragmentation both completed before the eye is entered, and with good hydrodissection carried out, minimal stress is exerted on the patient’s compromised zonules.
Additionally, I’ve found the femtosecond laser helpful in patients with mature white cortical cataracts with no or virtually no red reflex. The laser consistently makes a precise anterior capsulotomy. I still use trypan blue dye to stain the capsule as a first step to be certain that a complete capsulotomy is achieved. Fragmentation must be turned off in these cases, as the laser cannot see through the cataract. The incisions, however, can be done without difficulty.
As with white cataracts, femtosecond technology adds similar benefits in very dense nuclear cataracts. Sometimes manual capsulotomies are difficult in these dense lenses for reasons that include poor visibility and zonular issues that are often seen in older patients. I program the laser to enlarge the capsulotomy in these eyes, thereby allowing easier nuclear disassembly. Further, femto allows me to fragment the nucleus to further ease nuclear removal.
POOR CANDIDATES
The reasons that a patient might not be the best candidate for laser cataract surgery are varied. For patients who simply cannot get comfortable or have positioning problems, docking of the laser may be poor, and these cases are more likely to be a challenge to complete.
Even if the laser makes an incomplete capsulotomy, however, it is no problem to manually complete it. The surgeon must in all cases identify the capsulotomy as complete and not assume that it is; this assures that there will be no issues with anterior capsule tear-outs. In more than 2,000 cases, I have never experienced a tear in an eye in which the capsulotomy was confirmed to be complete. Often I prolapse the nucleus, putting stress on the capsulotomy edge, and often I polish the capsule at the end of the case with the irrigation/aspiration tip.
Eyes with small pupils are also potentially poor femto candidates. I do not perform laser capsulotomy or fragmentation in these eyes, but if I want to use the laser for corneal relaxing incisions I simply program the laser to skip the capsulotomy and fragmentation steps. I believe that astigmatic corneal incisions made by the laser are more precise than those I can achieve manually. Some surgeons advocate opening the eye and placing a pupil expansion ring, then going back to the femtosecond laser and proceeding with all steps, but I do not do this. The LenSx Laser has a hard dock, as opposed to a liquid patient interface, and I believe this process would be somewhat difficult with this configuration. Lasers with liquid interfaces may have an advantage here.
Eyes with deep-set globes or small interpalpebral fissures may also be poor candidates for the laser. These anatomic features pose a challenge with docking. Once the eye is docked successfully, however, the case can proceed as usual. Choosing a speculum that provides good exposure is helpful in these eyes.
Skittish or extra-sensitive patients can be a challenge with the femtosecond laser. As mentioned, the LenSx is a hard dock, so there is some sensation involved with docking. In view of this, I had my own eye docked to experience what the pressure is like. Although there was some pressure, it was minimal and easily tolerated. Therefore, I do not automatically exclude patients who are sensitive to touch in the exam lane. With most patients, I don’t sedate for the femto step, but for these sensitive or skittish patients I may give 1 mg of midazolam. Once the eye is docked, the entire laser procedure takes approximately 1 minute.
THE COST FACTOR
The biggest impediment to the use of the femtosecond laser, by far, is cost. I do not charge patients for the use of the laser; it is part of my package, but this package costs money. Patient resistance, therefore, is almost always financially based.
Surgeons may also experience their own financial resistance, as the femtosecond laser is an expensive piece of equipment with disposable costs per case that must be recovered. Further, time is money, and use of the laser does slow the case load down. There are real time requirements, though generally only a few minutes per case. I look at use of the femtosecond laser as another case, so to speak, as it is part of a package that brings additional revenue. Looked at in that regard, the extra time is not a disadvantage.
AN OVERALL ADVANTAGE
Overall, I believe that femtosecond technology is already an advantage to my practice. Figure 2, which shows my results with the first 332 eyes done with femtosecond laser assistance in my practice, represents a consecutive series of patients with no selection bias. The graph illustrates the most important outcome to me: postoperative binocular UCVA. These excellent results are a chief reason why I prefer laser cataract surgery in selected cases.
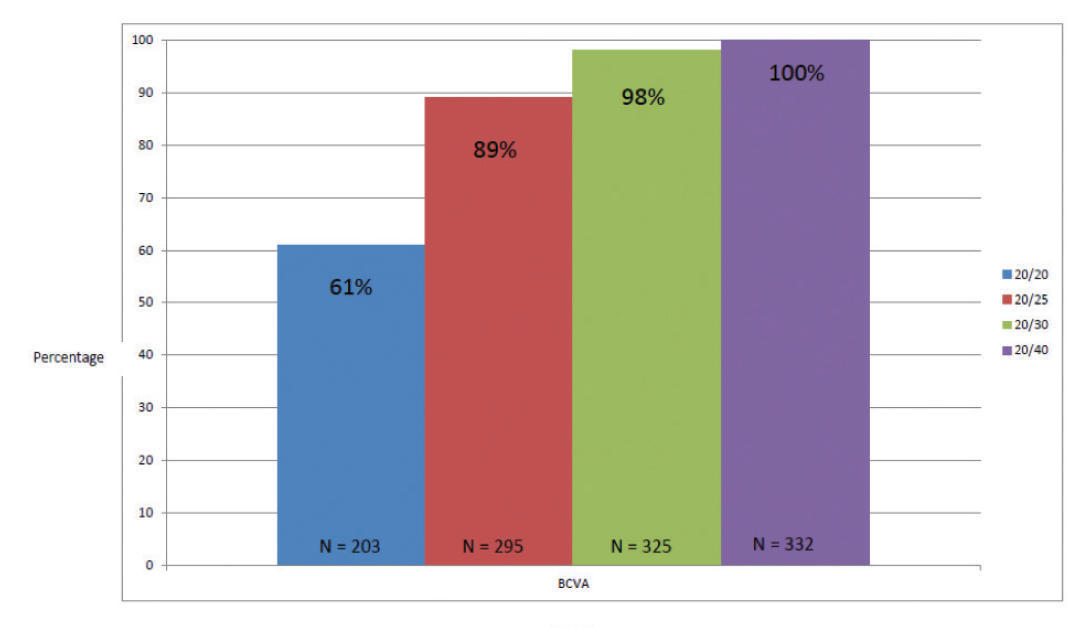
Figure 2. Binocular UCVA results in a consecutive series of the first 332 laser cataract surgeries in Dr. Reiser’s practice. All patients achieved 20/40 or better binocular UCVA.
As we move forward, I believe that the femtosecond laser will continue to improve cataract surgery as the technology evolves with software and hardware upgrades. This technology is in its infancy and, as a result of the incorporation of femtosecond laser, I believe we will start to see changes in IOL design, cataract surgical techniques, and other unforeseen advances that will take advantage of the laser’s performance capabilities.

Femto Fits, Sometimes
But other times, adjunctive devices fit better into the flow of my surgery.
By Vance Thompson, MD
My premium cataract surgery journey has evolved over the years. My technique for capsular opening has gone from manual capsulorrhexis, to femtosecond laser capsulotomy, back to manual capsulorrhexis, and most recently to automated capsulotomy with the »Zepto Capsulotomy System (Mynosys) guided by the Purkinje method of visual axis centration.
As you read this opinion piece, realize that I believe the femtosecond laser has revolutionized refractive corneal and cataract surgery. I believe that its place in corneal refractive surgery is solidified because of the increased safety and accuracy of making a femtosecond laser flap in LASIK and beause it is the only way to create a precision lenticule in the small-incision lenticule extraction procedure.
I also believe that the femtosecond laser was one of the most significant aspects in my process of becoming a more complete premium cataract surgeon. Having said that, I think that its place in cataract surgery is potentially more evolutionary than golden, compared with the vital role it played in making corneal refractive surgery better.
LIKES AND DISLIKES
All aspects of laser cataract surgery have taught me about the importance of each step in cataract surgery. With experience, I learned where my preferences were to use the femtosecond laser.
When I first started working with the laser, I used it for all aspects of cataract surgery including the primary and sideport incisions, astigmatic keratotomy (AK) when indicated, anterior capsulotomy, and lens sectioning and softening. With experience, I stopped using it for clear corneal incisions (CCIs). I couldn’t do my preferred limbal incisions consistently with a laser, and I felt that my manual limbal incisions were better and more self-sealing. I was never a huge AK surgeon, preferring instead corneal laser ablation or toric IOLs to address astigmatism. As a result, I did few laser AKs.
I liked (but did not love) the laser’s nuclear sectioning. It is something that I simply did because I was there at the laser, doing what I truly loved about the laser: the anterior capsulotomy. I love the roundness and consistent size of a laser capsulotomy. What I didn’t love about the laser capsulotomy, however, was the lack of consistent 360º of anterior capsular overlap of the IOL optic.
MIsSING THE OVERLAP
Anterior capsular overlap lessens the chance of IOL tilt or decentration with capsular fibrosis and contraction. I try to achieve this overlap with every cataract surgery. I consider anterior capsular overlap the most important step to ensure good quality cataract surgery. I realized, however, that femtosecond lasers that center the capsulotomy on the pupil miss consistent capsule overlap more frequently than I would like.
Using a laser that performed OCT image-guided capsulotomies improved my capsular overlap rate, but these can be further improved. If the eye was tilted too much after suction, the tilt compensation was not enough. I experienced too many cases of a beautiful round capsulotomy of a perfect size but not overlapping the optic.
My frustration with laser capsulotomies coincided with my learning about the use of the Purkinje method of centering refractive procedures. An important 2014 paper by Chang and Waring taught me to use a 6-mm optical zone corneal marker centered on the first Purkinje image with the patient fixating on my microscope light.1 This allowed me to make an epithelial imprint to guide my capsulorrhexis, and the capsulorrhexis would then be centered close to the visual axis. If I stayed inside my optical zone marker, I would end up with a 5-mm round capsulorrhexis. With this technique, my capsular overlap rate rose higher than it had been with OCT-guided laser capsulotomies. My use of the femtosecond laser started to decline as I adopted this technique. Remember, in a well-performed cataract surgery, complete anterior capsule overlap minimizes lens tilt and decentration due to capsular contraction. This is one of the most important aspects of the procedure. I was achieving this more consistently with the subject-fixated, coaxially sighted corneal light reflex Purkinje corneal marking method for manual capsulorrhexis than I had with a femtosecond laser.
However, I was still not achieving it in all cases. It is a challenge to make a well-centered corneal mark and then follow it while working on a lens, when the patient is supposed to be fixating on the microscope light the whole time. This is why, in my opinion, the manual capsulorrhexis is the most stressful aspect of cataract surgery.
ENTER ZEPTO
I then learned about the Zepto technology. Just as with femtosecond corneal and lens surgery, I was an investigator in the infancy of this device. The capsulotomy tip of the disposable, handheld instrument consists of a compressible shape–memory alloy nitinol capsulotomy ring housed within a soft, clear silicone suction cup. The tip collapses to enter the primary corneal incision and expands within the anterior chamber back to a circular shape of a predetermined size. Suction is then used to appose the nitinol ring against the capsule, and a low-energy, multipulse algorithm is used to create a precision pulse capsulotomy in milliseconds, 360º along the circular capsulotomy path.
I found that the device fit right into the flow of my surgery, with no need for a second room as with the femtosecond laser. It creates a strong capsulotomy edge2 and costs much less than the femtosecond laser.
Because Zepto fits into the flow of my surgery, I am more efficient. In a half-day cataract surgery session, I can schedule six more cases. This increase in my efficiency has been wonderful.
My favorite aspect of the Zepto capsulotomy is that I was able use the subject-fixated, coaxially sighted corneal light reflex Purkinje method to create consistently round capsulotomies, perfectly centered on the patient’s visual axis, every time. The device revolutionized my ability to center the capsulotomy on the first Purkinje image with the patient fixating and allowed me to achieve a consistent 360º of anterior capsule overlap.
Zepto technology is now my preferred method for creating the all-important capsulotomy in premium cataract surgery, and I recently performed my 500th capsulotomy with the device.
LASER SOMETIMES
Because of my success with Zepto, we have returned one of the two femtosecond cataract surgery lasers we had in our practice. The remaining laser in our center is still used for clinical trials that require it. Someday, if the laser can consistently provide 360º of anterior capsule overlap, be integrated into my OR rather than in a second room outside the OR, and fit my surgical flow as nicely as Zepto, I may see its use increase again.
Whether I am doing a traditional cataract surgery with manual capsulorrhexis or a premium cataract surgery with the Zepto automated capsulotomy, I use the Purkinje method of centering the capsulotomy. I find it much easier to work right on the lens surface and not to combat parallax with eye movement, as when I am trying to follow a corneal mark manually. When the capsulotomy is centered well, it serves as a reference marker for the visual axis and IOL placement.
I now attempt to center the optic of any implant on the first Purkinje image along with achieving 360º of capsule overlap. This attention to centration of the capsulotomy allows the true hero of cataract surgery—the IOL implant—to do its best work for the rest of the patient’s life in a well-centered, nontilted manner.
1. Chang DH, Waring GO 4th. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol. 2014;158(5):863-874.
2. Thompson VM, Berdahl JP, Solano JM, Chang DF. Comparison of manual, femtosecond laser, and precision pulse capsulotomy edge tear strength in paired human cadaver eyes. Ophthalmology. 2016;123(2):265-274.

I Never Do Femto
(But I do reserve the right to change my mind.)
By Mitchell Gossman, MD
When laser cataract surgery first emerged in the early 2010s, it was interesting to me. I was an early adopter of other new and exciting cataract surgery techniques and technologies, such as the capsulorrhexis; phacoemulsification; foldable, toric, multifocal, and accommodating IOLs; diamond blades; each new generation of IOL power calculation formulas; and optical biometry. Adding to the appeal of potentially improved safety, efficiency, or efficacy of cataract surgery was my attraction to any advanced technology. This is a deep-seated trait in my own DNA: I’m a tech freak.
And yet, sometimes I still use pencil and paper in my plane’s cockpit (Figure 3).

Figure 3. High-tech glass cockpit with iPad and four GPS units, and still a sticky note is attached to the yoke.
THE WRONG ANSWERS
Nevertheless, I have decided not to employ femtosecond technology at this time—but I do reserve the right to change my mind.
So why not now? Let me attack this question by taking on some of the wrong answers.
Fear. One of the attractions of the technology is the possibility of greater safety via simplicity. You dock the device to the eye to perform the most technically challenging parts of the procedure, namely the creation of the corneal incision, limbal relaxing incisions (LRIs), capsulotomy, and nuclear division—all at the press of a pedal. Because this is simpler than creating these by hand with conventional instrumentation, fear is no reason not to use femto.
Availability. Granted, it would be easier to use the device if it were already available at an ambulatory surgery center (ASC), rather than obtaining it via a roll-on/roll-off, rental, or purchase option. But getting the laser is simple.
THE RIGHT ANSWERS
So why not use femto currently? Here are the right answers, for me, step by step.
Clear corneal incisions. Manual CCIs made with metal or even diamond blades are extremely low-cost, effective, and fast. They are readily sealable. I see no advantage to using a laser to cut tissue here, and in fact many femtosecond laser users skip this step.
LRIs. Limbal relaxing incisions made with a diamond blade are reasonably safe and effective. It would seem to follow that femtosecond-created LRIs would be just as safe and effective and should be more precise, but I have seen no evidence yet that they are even equally effective. Furthermore, because we are past the days when toric multifocal IOLs were unavailable and performance of in-office LRIs was occasionally needed based upon a refraction, I currently see little need for LRIs in general. I believe that patients with a projected postoperative refractive astigmatism of 1.00 D or greater are best served by a toric IOL or planned postoperative laser or LRI, rather than attempting to treat meaningful amounts of astigmatism with bigger LRIs.
It is arguable that LRIs have a role for low amounts of astigmatism. In my opinion though, 0.25 to 0.50 D of astigmatism is mere visually insignificant noise that is not worth treating, especially when based upon preoperative projections rather than a refraction. This leaves 0.75 D of cylinder as what I would consider to be a reasonable femtosecond laser treatment, filling the gap between trivial astigmatism and toric IOL territory. This is too small a target for such an expensive device.
Capsulotomy. The manual capsulorrhexis can be rapidly and safely performed with a needle or forceps, without undue concern about pupil size and iris expansion. The cost is negligible and the safety excellent. I also find it useful to get tactile and visual feedback when creating the capsulorrhexis to help assess zonular integrity. The femtosecond laser capsulotomy is extremely precise because it’s made by a machine, but is it worth the extra time and expense? I think it is not, in any but the rarest of cases.
It is my opinion that the postulated additional precision of refractive results—due to greater precision of effective lens position after surgery and to minimizing IOL tilt due to perfect lens overlap—are of a trivial degree against the background noise. It would require an extremely powerful study to uncover this slight benefit, and I submit that the amount would likely be clinically insignificant.
Nuclear division. Dividing the nucleus with the femtosecond laser has been hailed as a way to decrease the amount of energy expended in the eye to break up the lens. Unfortunately, studies that demonstrate a meaningful clinical benefit are lacking, aside from possibly reducing the degree of corneal edema and improving visual acuity on the first postoperative day.1
How to pay for the laser. I worry about how to achieve return on the large capital investment needed to acquire femtosecond technology. None of the ways to pay for it are attractive:
No. 1: Charge the patient extra. In the United States, this is expressly forbidden unless the entire procedure is paid for by the patient without the involvement of insurance payments.
No. 2: Perform LRIs to treat astigmatism with the laser. I’ve already explained why I think LRIs are a poor choice in most cases. Further, the cost is too high.
No. 3: Incorporate the femtosecond laser into a premium IOL channel (such as toric or multifocal IOL) and bundle the cost. Due to the law of supply and demand, with this approach fewer patients will opt for the lenses, the cost will come out of my fee, or both.
No. 4: Convince an ASC to provide the laser at no extra cost. This is not likely, as financial margins are tight already.
No. 5: Convince the hospital to provide the laser at no cost. This is being done in some US centers. I feel this is merely a symptom of hospital-based facility fees being too high and hospitals seeking a competitive edge.
CONCLUSION
With high cost to the patient comes higher expectations, potentially unreasonably high. Therefore, for all the reasons cited here, I have elected not to pursue femtosecond technology at this time. This may change if the costs come down, if further benefits emerge, and, most important, if it is demonstrated that there is a benefit for my patients that is worth the time and money—mine and theirs.
Would my negative opinion carry more weight if had I tried the laser technology first, before deciding not to adopt? Yes, to a degree, and I look forward to reading the opinions in this issue of those who have tried and given up the femtosecond laser. However, I’ve seen the femtosecond laser in action, been to meetings, and read the articles. The use of this technology is feasible for any cataract surgeon. My reasons for not using it involve cost, efficacy, and payoff for my patients—pure and simple.
Why I Abandoned Laser Cataract Surgery
Dissapointing outcomes led me to break up with this technology.
By Jorge L. Alió, MD, PhD, FEBOphth
Ten years ago, I was involved in the late stages of development for clinical application of the femtosecond laser in cataract surgery. At that time, I participated in and received direct information and education from both the company developing the technology, LenSx, and the main surgeon involved in the topic, Zoltan Z. Nagy, MD.1
I was enthusiastic then about the development of a technique that, it seemed to me, was going to be disruptive.2 I anticipated that it would change the practice of cataract surgery due to the application of new diagnostic imaging to cataract surgery and the introduction of control and precision in the performance of surgical maneuvers that previously had depended chiefly on the surgeon’s skills. I expected the laser to provide better cataract surgery results, along with safer surgeries, to the benefit of both patients and surgeons.
I received the first femtosecond laser cataract surgery device (LenSx; Alcon) in Spain, which was installed in our office on October 11, 2011. I immediately began clinical studies to confirm the laser’s ability to improve the outcomes of cataract surgery. These studies compared laser cataract surgery to manual cataract surgery with a standard 2.2-mm incision and to microincision cataract surgery (MICS) performed through two 1-mm incisions. I was especially interested in the latter, as MICS had been the standard of my cataract surgical practice for a long time.3
DISAPPOINTING OUTCOMES
Our studies were quickly finished and published, and we had to admit, with disappointment, that laser cataract surgery did not provide better outcomes than manual conventional surgery in terms of visual results,4,5 speed of recovery, or refraction and optical performance of the eye following surgery.5-7
This was a disappointment because, in parallel, we had evidence that the highly significant increase in cost to our patients made it difficult or impossible for us to recover the added cost of using the femtosecond laser in cataract surgery. The introduction of laser cataract surgery technology resulted in important financial losses to our institution, as most of the cost had to be absorbed by us as an increased cost of providing cataract surgery.8
PATIENT PROBLEMS
Based on these outcomes and a lack of positive findings either on the clinical or financial level, we decided to abandon laser cataract surgery in 2013, as we determined that the situation was not sustainable. Our evidence of the negative cost-effectiveness of the technology was coincidentally confirmed by other authors.9-12
In many cases, patients became confused when confronted with the decision between conventional cataract surgery or femtosecond technology, especially with the major difference in respective costs. We were unable to guide their decisions by offering any clinical evidence in favor of using the technique with the higher cost, other than the fanciness of the new technology and the beautiful control of some of the surgical steps performed with the femtosecond laser. Many patients saw this much more as a benefit for the surgeon rather than the patient. Further, many of them declined to undergo surgery at all when they were confronted with a decision that they couldn’t understand. Therefore, not only were we unable to recover the cost of laser cataract surgery in most cases, but we were losing patients. In short, femtosecond laser technology was not a good marketing tool for us in our practice in Spain.
MY PRACTICE TODAY
Today, I use laser cataract surgery in certain environments, such as in the Arabian Gulf area where I also have a clinical practice. I enjoy the use of the diagnostic technology and the associated precision. This does not mean that my enjoyment is followed by a better outcome, but I do want to be involved with the femtosecond laser because I think that the future for laser cataract surgery will be better when the costs are reduced and it becomes more cost-effective. When that occurs, the femtosecond laser will probably once again become an additional tool for cataract surgery in our practice.
Laser cataract surgery itself is a beautiful technique. It generates and uses a huge amount of information that probably will find better applications in cataract surgery in the future. The main conceptual problem is that, on the contrary from what I expected, laser cataract surgery is not the disruptive technology I thought it would be at the beginning,2 but rather an alternative technology to assist in cataract removal. It is a technology that we can choose or not for our patients, without any clear benefit over standard clinical and surgical practice.
Laser cataract surgery may be useful as a marketing tool in some environments, but not all. The vast quantity of clinical information available to patients—including information about new technologies with no proven evidence of added efficacy and yet higher costs—may make patients more selective in some countries than in others, especially if they must pay out of pocket for the increased cost of this type of surgery.
I am sure that the femtosecond laser will be part of our practice in the future. However, its cost-benefit ratio must be improved, its accessibility increased, and better financial models developed to make it more suitable for modern cataract practices.
1. Garg A, Alio JL. Femtosecond Laser Techniques & Technology. New Delhi: Jaypee Brothers Medical Publishers; 2012.
2. Lindstrom RL The future of laser-assisted refractive cataract surgery. J Refract Surg. 2011;27(8):552-553.
3. Alio JL, Rodriguez-Prats JL, Galal A, Ramzy M. Outcomes of microincision cataract surgery versus coaxial phacoemulsification. Ophthalmology. 2005;112:1997-2003.
4. Nagy Z, Filkorn T, Takacs A, et al. Anterior segment OCT imaging after femtosecond laser cataract surgery. J Refract Surg. 2013;29(2):110-112.
5. Alio JL, Abdou AA, Soria F, et al. Femtosecond laser cataract incision morphology and corneal higher-order aberration analysis. J Refract Surg. 2013;29(9):590-595.
6. Alio J, Soria F, Abdou A. Femtosecond laser assisted cataract surgery followed by coaxial phacoemulsification of microincisional cataract surgery: differences and advantages. Curr Opin Ophthalmol. 2014;25(1):81-88.
7. Alio J, Soria F, Abdou A, Peña-Garcia P, Fernandez-Buenaga R, Javaloy J. Comparative outcomes of bimanual MICS and 2.2-mm coaxial phacoemulsification assisted by femtosecond technology. J Refract Surg. 2014; 30(1):34-40.
8. Alio JL, Abdou A, Arias Puente A, Zato MA, Nagy Z. Femtosecond laser cataract surgery: updates on technologies and outcomes. J Refract Surg. 2014;30(6): 420-427.
9. Abell RG, Darian-Smith E, Kan JB, Allen PL, Ewe SY, Vote BJ. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg. 2015;41(1):47-52.
10. Feldman BH. Femtosecond laser will not be a standard method for cataract extraction ten years from now. Surv Ophthalmol. 2015;60(4):360-365.
11. Bartlett JD, Miller KM. The economics of femtosecond laser-assisted cataract surgery. Curr Opin Ophthalmol. 2016;27(1):76-81.
12. Abell RG, Vote BJ. Cost-effectiveness of femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery. Ophthalmology. 2014;121(1):10-16.




