Lisa Brothers Arbisser, MD

The story begins with appropriate preoperative informed consent. There is no significant inherent risk to the choice of a toric implant other than minor added manipulation during placement. I do not hesitate to recommend these IOLs, even to monocular patients or for high-risk eyes, but I am certain to inform patients that astigmatism management is an inexact science, even with the most modern equipment and most experienced surgeon. I tell them that, rarely, more than one surgery is required to achieve the aim.
AVOIDING PROBLEMS
Patients must discontinue wearing their contact lenses until preoperative measurements are stable. The health of the ocular surface must be optimized, and irregular astigmatism should be weeded out. It is important to diagnose and treat anterior membrane dystrophy, if present, with superficial keratectomy. The use of modern nomograms accounting for posterior corneal curvature is key.
In the OR, besides the usual time out to ensure that the correct lens has been selected and the topography maps are hanging within view, I think it is extremely helpful to have an intraoperative keratoscopic light reflex to confirm the steep axis. This step can be as simple as the mire projected by the circular end of a sterile safety pin, as time-efficient and cost-effective as my Mastel light ring, or as quantitative as aberrometry to avoid transcription errors and to strive for uniform perfection.
HANDLING MISALIGNMENT
Unexpected, unavoidable outcomes herald detective work. Were the measurements accurate? Was the correct lens placed? Is the lens aligned on the intended meridian? Assuming that these sources of error are ruled out, the online resource astigmatismfix.com (thanks to John Berdahl, MD, and David Hardten, MD) will provide the answer on how to rotate or, so rarely, exchange the lens. As wonderful as this resource is, however, a more modern approach is the Barrett Rx formula (https://www.apacrs.org/barrett_rx105). Surprisingly, people often see better uncorrected than the refraction would imply, so the first step is to be sure the patient is sufficiently dissatisfied with the outcome to accept the small but real risk of repeat surgical intervention.
Lisa Brothers Arbisser, MD, demonstrates the forward optic capture of a toric IOL that rotated off axis.
Especially if a lens has rotated from the ideal position where it is thought to have been placed, I recommend waiting a couple of weeks to allow the bag to shrink but not scar around the implant, making the final position more likely stable. Under topical anesthesia, I would mark the final axis and confirm it with intraoperative keratoscopy. Next, using only paracentesis incisions, I would instill a cohesive ophthalmic viscosurgical device to expand the bag. A two-handed technique can free and rotate the lens to the ideal axis. Keratoscopy will provide both a corneal and lenticular mire, the ovals of which should appear 90º opposed. The procedure concludes with manual irrigation and removal of the viscoelastic. I favor an intracameral injection of moxifloxacin (off label) as well.
Despite talk in favor of inserting a capsular tension ring in cases of a spontaneously rotated toric IOL, I have found this strategy to be unreliable. If a lens rotates more than once, I would forward capture it while leaving the haptics in the bag (see video above). There is a very small risk of iris chafing postoperatively with this maneuver. An alternative would be to perform a hyaloid-sparing posterior capsulotomy and to capture the optic into Berger’s space. Capture will ensure stability.
Daniel H. Chang, MD

Since a misaligned toric IOL can result from preoperative (ie, inaccurate measurements), intraoperative (ie, poor positioning), or postoperative (ie, rotation) mechanisms, I take steps to prevent each of these potential causes. Preoperatively, I measure the axis of astigmatism with both a biometer (at least twice) and a topographer. Intraoperatively, I manually register my axis of correction using preoperative iris imaging to ensure a proper transfer of information. During surgery, I create a triplanar wound, center and size my capsulorhexis for complete IOL overlap, remove viscoelastic from behind the lens, rotate and align the IOL, and seal the wound meticulously. Although not all misalignment is caused by rotation, wound leakage, hypotony, and subsequent globe compression (from applying eye drops or rubbing the eye) can transmit an external force to the IOL, thus inducing rotation.
FIRST STEP
Whenever dealing with decreased UCVA postoperatively, I first determine whether the BCVA is reduced. If so, I determine what the limiting pathology might be—whether it is ocular surface/corneal, IOL/capsular, macular, or other pathology—and I treat it accordingly. If the BCVA is good, the problem is purely refractive, in which case I determine if the patient is symptomatic. When it comes to correcting refractive error, the patient’s satisfaction is my primary endpoint. If he or she is happy, then I am happy, and we are done. If the patient is unhappy, then I consider an enhancement.
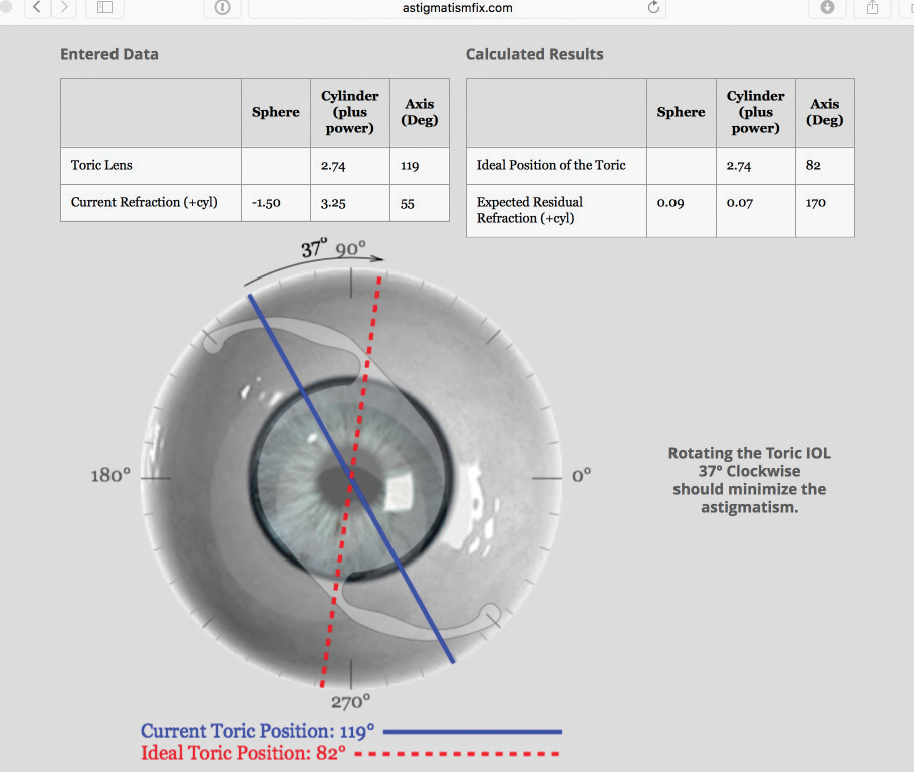
Figure. Output from astigmatismfix.com suggests that a 37º clockwise rotation will reduce the postoperative refraction from -1.50 -3.25 × 55º to +0.09 +0.07 × 170º.
HANDLING MISALIGNMENT
If the limited UCVA is indeed because of a misaligned toric IOL, the BCVA should be good, and the refractive spherical equivalent should be zero. If the spherical equivalent is not zero, then there must also be an IOL power issue. In that case, I will consider laser vision correction or, rarely, an IOL exchange or a piggyback IOL.
If the problem is purely a misaligned toric IOL, I first determine whether rotating the lens could correct the refractive error. The easiest way to make this determination is through the website astigmatismfix.com (Figure). If the output from this website suggests that I can reduce the clinical astigmatism close to zero through rotation/repositioning of the IOL, then that will be my preferred approach (barring significant previous intraoperative difficulties such as a floppy iris). If the calculations instead suggest that there will be significant refractive error regardless of how I rotate the IOL (ie, the toric power is too little or too much), then I will perform laser vision correction.
TIMING
The tricky part about addressing a misaligned toric IOL is the timing. Ideally, I like to wait for healing and refractive stability, but if I plan to reenter an eye, I prefer to do so sooner rather than later. It is difficult to determine an effective refractive approach, however, prior to achieving good BCVA. It therefore all comes back to surgery: the better the initial procedure is, the quicker the patient heals, and the earlier I can decide how to approach the misaligned toric IOL.
Steven Dewey, MD

Great care was taken preoperatively to accurately measure the astigmatism and account for the posterior aspect. The proper marks for aligning the toric lens were made. In the OR, the perfect capsulotomy was created, viscoelastic was thoroughly removed from behind the IOL, and the stroma was hydrated prior to final alignment of the lens so that pressurizing the globe would not displace the IOL from the intended position. Postoperatively, the toric IOL is misaligned. Now what?
DIAGNOSIS
Diagnosing a malrotated toric lens is best done with a manual refraction showing an oblique orientation of the new astigmatism compared to the original keratometry reading. I personally prefer the iTrace (Tracey Technologies) for its ability not only to diagnose a malrotated toric IOL through an undilated pupil, but also to plan the rotation to properly align the axis. The iTrace will account for improper original alignment, surgically induced astigmatism, or simple rotation after surgery (Figure).
HANDLING MISALIGNMENT
The first step in repositioning a toric lens is to allow enough time to pass for the capsule to shrink around the IOL, usually 3 weeks or so. I try to use the original sideport incision and typically encounter little resistance. Reopening the primary incision may create an unstable chamber or alter the induced astigmatism. In almost all cases, simple irrigation of the capsule will mobilize the toric lens, while the small incision helps to keep the chamber stable. I avoid viscoelastics to further reduce intraocular manipulations. I try to achieve complete lens rotation to ensure that the haptics do not restrict the final placement. A second sideport-type incision may be necessary to facilitate access for the IOL’s rotation and placement.
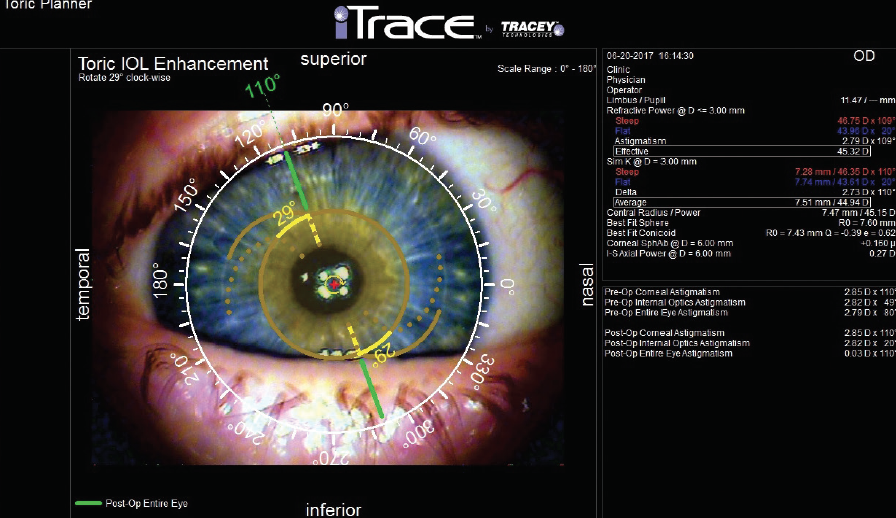
Figure. A patient presented with blurred vision following placement of a Tecnis Symfony Toric IOL (Johnson & Johnson Vision). The iTrace displays the current position of the toric lens (tan dots) and the desired position (green line shows the axis, and yellow lines show the necessary rotation). Diagnosis of the malrotation and the surgical plan for remediation were obtained through an undilated pupil. In this case, rotating the lens 29º clockwise will decrease the astigmatism by 2.82 D, essentially reducing the residual astigmatism to zero.
I have only had one toric lens malrotate a second time. In this instance, I carried out the same steps I just outlined, but I used reverse optic capture to lock the optic in place. Simple tilting of the optic will move one of its sides anterior to the capsulotomy. I then place the second side anteriorly by sliding the optic toward the side out of the capsule and displacing it anteriorly as it slides back into position. Rotation of the optic can still take place with patiently deliberate manipulations. I have not tried to use a capsular tension ring to stabilize a malrotatated toric lens.
I believe that “late” malrotation is a circumstance of failing to recognize the problem in its early stages. Within the first few months, the capsule can be reinflated and the optic rotated. Viscoelastic may be essential for this task. The difficulty is that, if the error in rotation is small, the lens will want to go back to the original position to conform to the fibrosis in the capsule. Reverse optic capture has been my method of achieving refractive stability in these cases. I would be even more reluctant to try a capsular tension ring under these circumstances.
In cases where the capsule is firmly fibrosed around the optic or if the capsulotomy will not permit reverse optic capture, the refractive error can be treated instead. Whether the patient simply needs an astigmatic treatment with incisions or a more complete refractive solution such as LASIK or PRK will depend on the clinical situation.
Kevin M. Miller, MD

An IOL can rotate if there is insufficient friction between it and the capsular bag to hold the lens in place. An IOL is most likely to rotate if the material has a slick surface and the capsular bag is relatively large. After implantation, the haptics of an IOL will tend to seek out the long axis of an oval-shaped bag. This is especially true of plate-haptic lenses, but it can occur with loop-haptic lenses as well.
IOL SELECTION
To reduce the occurrence of rotation, I recommend choosing a lens that is less likely to rotate. My experience during the early days of the STAAR Surgical plate-haptic toric IOL was that it tended to rotate a lot. After the company increased the length of the haptics on its lower-powered toric IOLs and frosted their edges, rotations were virtually eliminated. Unfortunately, the STAAR Toric lens comes in only two powers and has a truncated cylinder optic, so it is not very popular these days.
The AcrySof IQ Toric IOL (Alcon), the second toric lens to enter the US market, has a tacky surface that resists rotation. Of approximately 1,000 implantations, I have had only three lenses rotate. The Tecnis Toric 1-Piece IOL (Johnson & Johnson Vision), the third to market, has a polished surface that is more likely to rotate than the AcrySof IQ Toric lens. I have had to reposition three Tecnis Toric IOLs in fewer than 100 implantations.
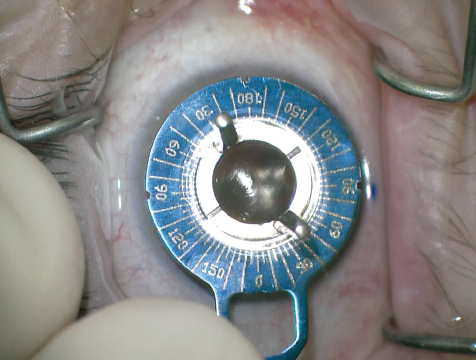
Figure 1. After making a reference mark at 6 o’clock with the patient sitting upright, Dr. Miller uses an Epsilon toric marker to mark the steep axis of postoperative corneal astigmatism.
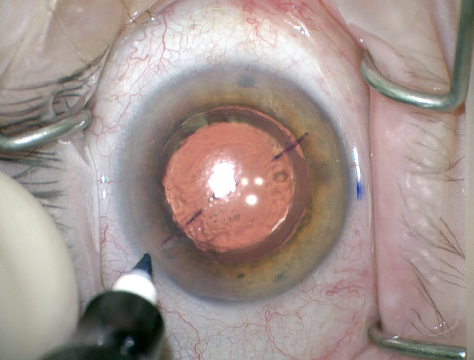
Figure 2. The surgeon dots the limbus on both sides, because the corneal marks will tend to fade as surgery progresses. The limbal marks can be adjusted one way or the other if the corneal marks are not perfectly centered.
INITIAL ORIENTATION
To avoid having to reposition a lens, make sure it is oriented on the correct axis at the end of surgery. Some rotations are, in fact, misalignments. It is important not to confuse the steep and flat meridians of the cornea. Always orient the lens to the steep corneal meridian. Also, do not implant a toric lens on the steep axis of manifest astigmatism. At the end of surgery, remove all of the OVD from the eye. If any burps out of the capsular bag, it might rotate the IOL.
I do not routinely dilate the pupil the day after surgery. I would not go back to the OR to reposition a toric lens even if I observed a sizable rotation at that examination. If the manifest astigmatism is unexpectedly high 1 to 2 weeks later, however, then I will perform dilation and check the orientation of the lens. If it is less than 10º off, I may consider leaving the IOL alone and prescribing glasses for any residual refractive error.
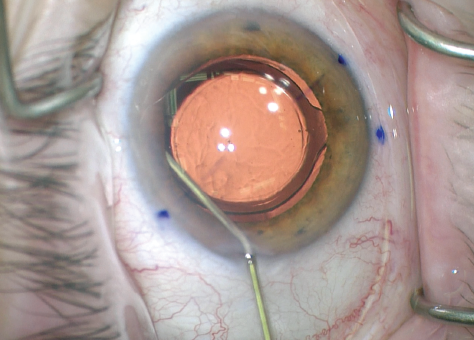
Figure 3. After reopening the phaco incision, the surgeon viscodissects open the capsular bag with a high-viscosity ophthalmic viscosurgical device (OVD).
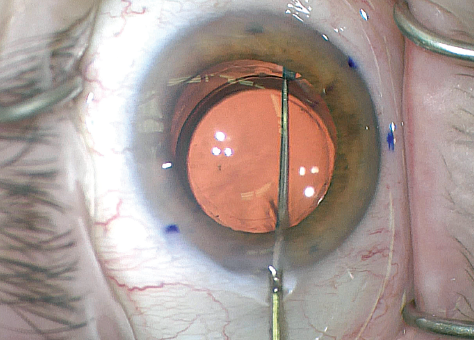
Figure 4. Dr. Miller spins the lens several times to break all capsular adhesions. The inside of the capsular bag is inherently tackier several weeks after the initial surgery. He then aligns the toric lens with the steep corneal axis.
HANDLING MISALIGNMENT
If you have to reoperate, it is important to remember that rotating a toric lens does not correct spherical refractive errors. If a spherical error is present, you will have to exchange the IOL or perform corneal refractive surgery. In my experience, most patients do not want to pay for keratorefractive surgery after they have paid for toric IOL services. Also, they likely will not want to have their misalignment “swept under the carpet” by a completely different type of surgery.
If you encounter a rotation that is substantial enough to warrant realignment, the fix is generally simple. Get back inside the eye within 3 to 4 months, preferably. Later surgery is possible but requires more dissection of the capsular bag. You will need to orient the plus cylinder axis of the toric IOL onto the current postoperative axis of corneal astigmatism. Note that this is not the axis calculated before surgery, and you do not need a calculator such as astigmatismfix.com to figure it out (Figures 1 and 2).
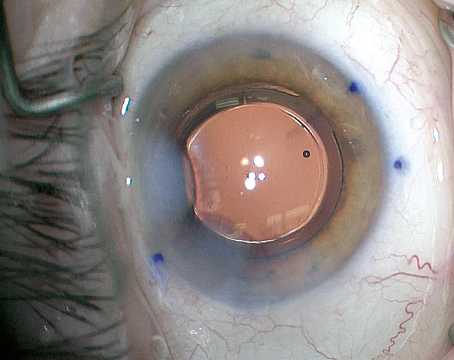
Figure 5. After removing all of the OVD, the surgeon confirms both incisions are hydrated and the IOL is properly oriented.
I like to reopen the phaco incision. When it heals once again, the same amount of corneal astigmatism will likely result. I fully dissect open the bag using a high-viscosity OVD such as Healon GV (Johnson & Johnson Vision; Figure 3). I do not want any capsular bag adhesions to remain that might impair proper orientation of the haptics (Figure 4). Once the bag is open, the lens can be reoriented with a Kuglen hook or another lens manipulator. If the eye is highly myopic or the axial length is high, the capsular bag will likely be large. In these cases, implantation of a capsular tension ring may help stabilize the orientation of the IOL. After that, I remove all of the OVD and rehydrate the incision (Figure 5).
I have never had to reposition a toric IOL twice (knock on wood).
Robert J. Weinstock, MD

The first and foremost considerations in these cases are the patient’s vision, refraction, and satisfaction. Many times, a patient whose toric IOL is significantly misaligned still has reasonable UCVA and no problems with or complaint about his or her vision. If the patient is happy and has good functional vision, my philosophy is to leave well enough alone and avoid further invasive maneuvers. When a patient with a misaligned toric IOL clearly expresses dissatisfaction and has lost a significant amount of UCVA, however, my attention turns to determining the best strategy for managing the problem. In large part, the decision centers on the answers to three questions:
1. How long has the lens been in the eye?
2. How far off is the toric IOL from its intended position?
3. What is the manifest refraction?
If the IOL was implanted 2 months ago or less, there is no significant fibrosis of the capsular bag, and the spherical equivalent is close to plano, I generally return to the OR and reposition the lens after opening the previous corneal wounds and inflating the bag with viscoelastic. Oftentimes, I will use intraoperative aberrometry for the final positioning of the IOL.
If the toric IOL was implanted more than 2 months ago, there appears to be a lot of capsular contraction and fibrosis of the capsule to the lens, and the residual astigmatism is less than 1.00 D, I will often choose either a manual limbal relaxing incision or a laser arcuate keratotomy created at the axis of the manifest refraction cylinder. For larger amounts of astigmatism, I will generally perform PRK to eliminate the refractive error or residual astigmatism.
If the spherical equivalent is not close to the intended target, rotating the IOL or placing a limbal relaxing incision alone will not correct the problem. In these cases, there are two options:
1. Exchange the IOL for a new toric lens with a different power, and place it in the correct axis.
2. Perform PRK to treat the residual astigmatic component and the myopic or hyperopic component that is present in the manifest refraction.
Multiple free software apps and online calculators are available to help determine the IOL’s intended position after the rotation, depending on the lens power and the manifest refraction.
The hardest part of surgical planning is deciding which technique to perform and what makes sense for the individual patient. The answer is not always clear, but with experience and thoughtful consideration, a misaligned toric IOL becomes an easily corrected problem and an opportunity to greatly satisfy the patient.