With next-generation technology and inventive surgical maneuvers debuting at a rapid clip in the realm of refractive cataract surgery, it is easy for time-tested techniques such as manual limbal relaxing incisions (LRIs) to fly under the radar. However, today more than ever, astigmatism management at the time of cataract surgery is essential to providing our patients with the best possible uncorrected vision. Leaving any viable option off the table is ill-advised.
There are several methods of managing astigmatism at the time of cataract surgery, including implanting toric IOLs and executing laser arcuate incisions, but the simplest and most cost-effective is the manual LRI. Although manual LRIs can be less predictable than other options, they are a tried-and-true strategy for correcting low levels of corneal astigmatism. Every cataract surgeon who is committed to maximizing refractive outcomes should be knowledgeable about and proficient at performing this particular type of corneal relaxing incision.
Despite the critical role that LRIs can play in modern refractive cataract surgery, data from the 2016 ASCRS Clinical Survey suggested that this essential technique is underutilized and perhaps even underappreciated.1 To help mitigate that discrepancy, I have developed a primer aimed at clarifying the five Ws—the who, what, why, when, and where—of this basic yet critical incisional technique.
Tips and Pearls
- Manual limbal relaxing incisions (LRIs)—and LRIs in general—can produce a hyperopic shift of about 0.20 D, so it is sometimes advisable to choose a higher-powered IOL than is suggested by the IOL power calculation.
- Any bleeding from corneal neovascularization can blunt the desired flattening effect of the LRI.
- A slight undercorrection can instantaneously be adjusted by creating a new LRI central to the existing one or lengthening the existing LRI (Figure).
- If an overcorrection occurs, it is safest to wait 2 to 3 months before performing any enhancements. To treat an overcorrection, consider a bandage contact lens initially if any gape exists. If that does not work, suturing the LRI can mitigate the effect. Eventually, the patient may need an LRI in the opposite axis.
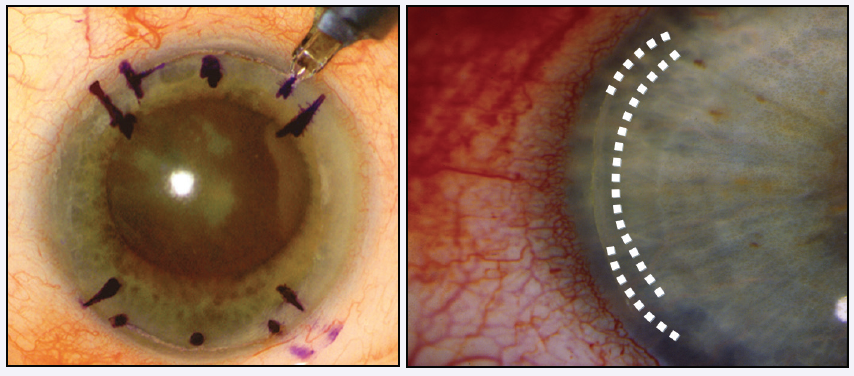
Figure. Treatment for undercorrection of astigmatism can be achieved by creating a new LRI central to the existing one or by lengthening the incision.
THE 5 Ws OF LRIs
1. Who performs LRIs? Surprisingly, fewer surgeons than one would think perform LRIs. According to the 2016 ASCRS Clinical Survey, of the 524 respondents, 28% did not perform any relaxing incisions, and only about 55% performed manual LRIs.1 Some reported performing only manual LRIs, some disclosed that they performed only laser arcuate incisions, and a minority revealed that they performed an even mix of manual and laser LRIs. Equally revealing is the finding that only 48% of surgeons-in-training and those with less than 5 years in practice reported having performed an LRI during residency. This statistic stems from a portion of the 2016 ASCRS Clinical Survey that focused solely on the experiences of young eye surgeons (YES; n = 393). Notably, the survey also reported that 60% of the 370 respondents considered their exposure to manual astigmatic relaxing incisions in residency to be inadequate.
2. What is an LRI? LRIs are partial-thickness penetrating incisions that are typically placed within 1 mm of the limbus and, as such, can more accurately be named “peripheral corneal relaxing incisions.” These incisions can effectively correct upwards of 1.25 to 1.50 D of total corneal astigmatism. A preset depth of 600 µm can be used, as can a variable depth with pachymetry set at 90% of the thinnest pachymetry reading. Either option can be employed, along with one of the well-established nomograms (Koch/Wang, Nichamin Age and Pachymetry Adjusted Intralimbal Astigmatic [NAPA], and Donnenfeld) to effectively address regular corneal astigmatism. The Koch/Wang and Donnenfeld nomograms are both more simply applied formulas that I carry with me as a resource so that, if I need them in the OR, I know I have them handy. The NAPA nomogram is a pachymetry- and age-adjusted formula, and while this nomogram is more expansive, it really allows the surgeon to better customize the lengths of the LRIs based on age and orientation of the astigmatism. Both the NAPA and Donnenfeld nomograms are available at www.LRIcalculator.com.
LRIs are cost-effective, as they require a low capital investment in just a few instruments: an astigmatic gauge, LRI marker, and LRI knife. Further enhancing the cost-effectiveness of this technique is the fact that some astigmatic gauges have a built-in astigmatic marker. LRIs are an excellent means by which to fix low amounts of astigmatism (< 1.00 D) when a toric IOL is not available, and for the patient, they are also a less expensive option than a toric IOL.
3. Why should you perform manual LRIs? One of the important features of the manual LRI is its speed, usually taking less than 5 minutes to perform. Moreover, manual incisions are ergonomically friendlier for the surgeon and more comfortable for the patient than laser arcuate incisions.
Another factor that supports the usefulness of manual LRIs is that they can be performed on the spot or spur of the moment, which is not the case with toric IOLs or laser arcuate incisions. If intraoperative aberrometry indicates that a relaxing incision should be placed, a manual LRI can be executed right then and there. Also, if for some reason a laser incision cannot be performed, such as in an Asian patient whose eye is too small to fit the system’s interface mechanism, a manual LRI can be performed in its place.
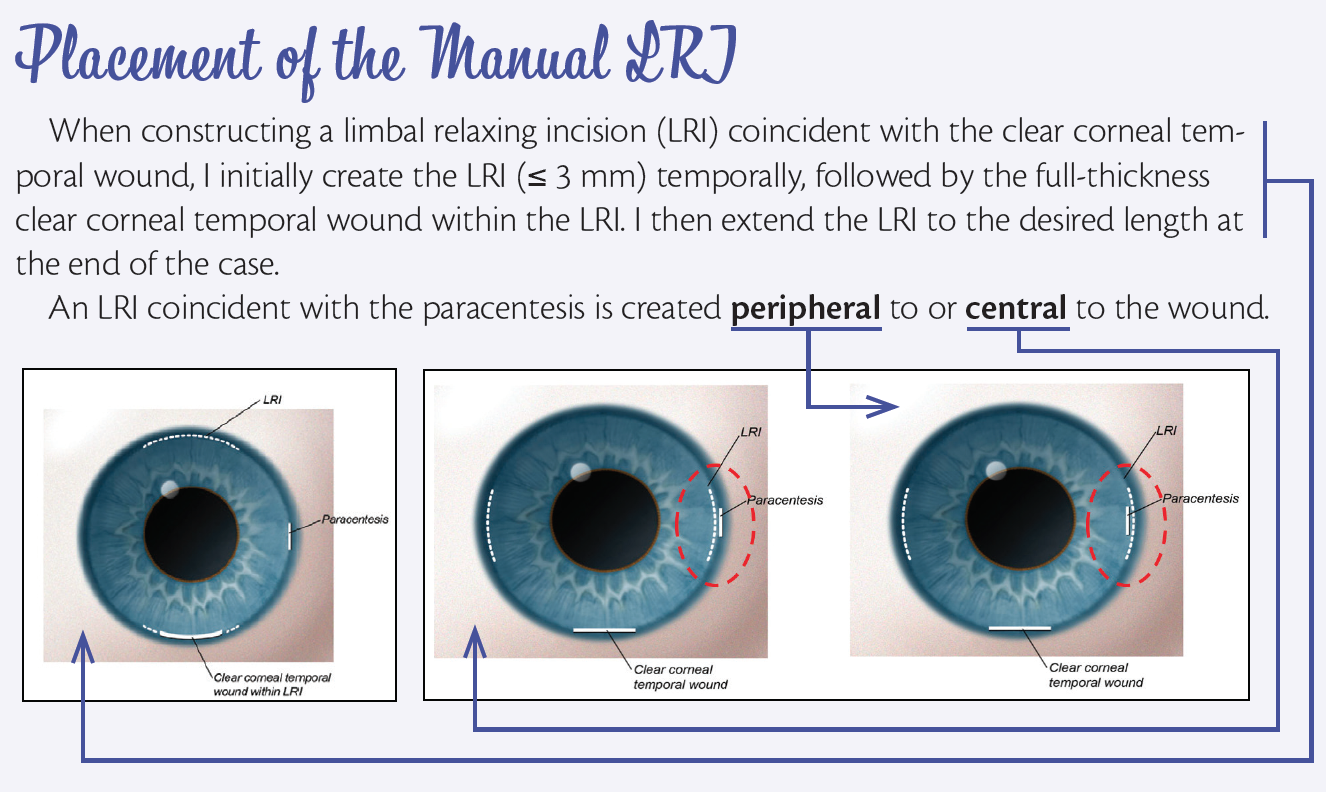
LRIs can be performed simultaneously with cataract surgery and can be made at several points during the procedure, including at the start of the case before making the phaco incisions, after the IOL’s insertion and before the removal of viscoelastic, or at the end of the procedure. A manual LRI can be made coincident with the clear corneal temporal wound or the paracentesis (see Placement of the Manual LRI) as needed, but if a single incision is called for, strategic placement of the LRI in the same meridian 180º away from the wound is preferred.
I make the LRI after inserting the IOL but before removing the viscoelastic or at the very end of the surgery in an eye hyperpressurized by balanced saline solution. The temporarily elevated IOP gives the eye some firmness and counter pressure to more readily perform the incisional procedure.
LRIs can also be performed independently from cataract surgery to correct up to about 1.25 D of postoperative residual mixed astigmatism. This additional procedure can significantly improve patients’ postoperative satisfaction. LRIs can also be employed to improve the outcome in, for instance, the case of a naive cornea with mixed astigmatism.
4. What if the LRI is coincident with the temporal wound with paired LRIs? In these cases, I create a short LRI temporally, within which I can create the primary temporal wound, and extend the LRI at the end of the case to the desired length. If it looks like the LRI might cross the paracentesis, my preference is to create the paracentesis peripheral to the LRI to prevent a wound leak, which is more commonly seen with centrally placed paracentesis wounds.
5. Where do you perform LRIs? This procedure can be done in the OR, in the LASIK suite, or even under the slit lamp in the case of an LRI adjustment.
CONCLUSION
Ultimately, the ability to manage astigmatism—including low levels of cylinder—at the time of cataract surgery is essential. Every cataract surgeon should be comfortable performing manual LRIs and have this technique as a part of his or her skillset.
1. ASCRS Clinical Survey 2016. http://supplements.eyeworld.org/h/i/289602006-ascrs-clinical-survey-2016. Published September 22, 2016. Accessed September 12, 2017.