
Many surgeons overlook the fact that patients frequently perceive pain as part of the cataract procedure. Patients’ fear of pain is common to any ocular surgery. With LASIK, for example, after its price, the fear of pain and blindness is a barrier to patients’ having the procedure. In an era when the tools and techniques of cataract surgery have elevated its potential to provide excellent results, patients’ concern about pain is a real factor in terms of how they perceive the procedure and its outcome.
INTRAOPERATIVE VERSUS POSTOPERATIVE PAIN
Most intraoperative causes of pain can be controlled with careful planning and a well-executed protocol. The nuances of ocular anesthesia (eg, how much, what type, and its timing) should be based on the individual case. Much research has been dedicated to intraoperative surgical pain, and there are evidence-based protocols for helping to avoid and control pain during the actual procedure.1,2
Pain that occurs postoperatively, on the other hand, is subject to many variables, even in routine, uncomplicated cases. Because every eye has different nerve endings, every patient’s response to pain will be different. Moreover, every surgical procedure differs, so the trauma that it causes to the eye is specific. Most patients feel no discomfort after a routine cataract surgery, but some may experience severe pain after the same procedure.
Although increased IOP after cataract surgery—especially in the immediate postoperative period—is a potential cause of pain, I have found that the most common cause of postoperative pain is drying of the ocular surface from the preservatives in perioperative drops, exposure during surgery, and wound creation. Regardless of the cause, severing the corneal nerves and exposing the epithelial cells to stress can produce a spectrum of feelings from a mild, scratchy, foreign body sensation to a strong pain reaction. Drying of the corneal surface can be mitigated to some extent, but it is a fairly common aspect of ocular surgery and can occur in routine cases.
Surgical complications introduce another source of postoperative pain. For example, during insertion, the speculum may abrade the epithelium. Alternatively, when touching the eye to stabilize it during wound creation, the surgeon may accidentally induce a corneal abrasion. Seemingly innocuous maneuvers can have unfortunate but potentially serious consequences.
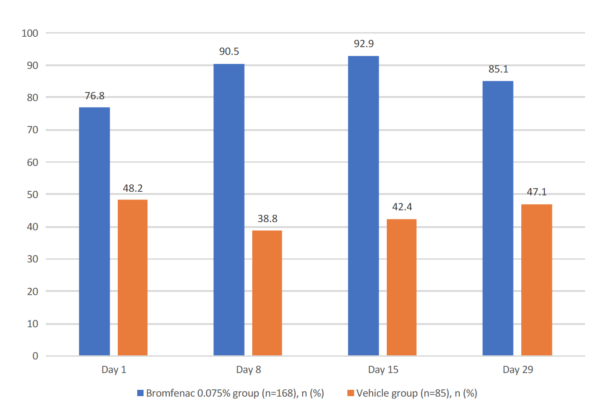
Figure. Percentage of subjects with a visual analog scale pain score of 0 at each postsurgical assessment. The difference between the Bromfenac 0.075% group and vehicle group was statistically significant at all time points (P < .001).
Several risk factors influence the development of postoperative inflammation, although it is often difficult to predict who is at risk. Nevertheless, excessive inflammation can lead to conditions such as cystoid macular edema.3 Modern cataract surgery techniques have lowered the potential for inflammatory responses; rates of cystoid macular edema, for example, are significantly lower in cases where small-incision techniques and phacoemulsification are used (about 0.1% to 2.33% of cases)4,5 compared with intracapsular (60%) and extracapsular techniques (15% to 30%).6 Although use of a femtosecond laser may further reduce the risk,7 inducing some degree of inflammatory response by virtue of intraocular maneuvers is an unavoidable consequence of eye surgery.
A PROACTIVE APPROACH
Refractive cataract surgery patients expect not only great visual outcomes but also a positive overall experience. Ophthalmologists concerned about their reputation and practice growth must evaluate patients’ experiences to ensure that both their clinical outcomes and their satisfaction are top tier.
In my practice, I take a very proactive approach to managing potential pain. In the immediate preoperative period, patients receive proparacaine and tetracaine to numb the ocular surface, followed by a diluted bupivacaine solution, which penetrates deeper into the eye to numb the internal structures. Most of my patients do not require intravenous anesthesia for pain relief, but I often provide midazolam and fentanyl to alleviate their anxiety. Some surgeons like to operate under greater sedation using low-dose sublingual ketamine. Deep-sedating agents like propofol are typically reserved for patients who have difficulty staying still.
During surgery, I favor Omidria (phenylephrine and ketorolac injection 1%/0.3%; Omeros) infused into the balanced salt solution to provide a constant stream of ketorolac and phenylephrine. The agent prevents pupillary miosis and has an anti-inflammatory effect. This FDA-approved product essentially replaces the off-label practice of injecting epinephrine into the balanced salt solution bottle. In clinical trials, the use of Omidria reduced the incidence of postoperative pain compared with placebo and, among patients who had pain, decreased its severity.8 Because ketorolac blocks the cyclooxygenase-1 and -2 pathways, Omidria further reduces the potential inflammatory response postoperatively.9
POSTOPERATIVE PERIOD
The bromfenac molecule is exceptionally well designed for ocular penetration and inflammation control.10 BromSite, a formulation of bromfenac in a DuraSite vehicle (Sun Ophthalmics), carries a specific indication for the prevention of ocular pain after cataract surgery. Although previous evidence suggested that earlier bromfenac formulations reduced postoperative pain, I find it reassuring to have supporting clinical data and an FDA trial (Figure).10,11
The DuraSite vehicle may provide additional benefits. The synthetic polymer improves the active ingredient’s penetration and retention time, and it is a mild lubricant. When it comes to pain management, little details matter. I find it important to educate patients that, although branded nonsteroidal anti-inflammatory drugs may cost more than generics, filling prescriptions as written is one of the most important elements of success and satisfaction following cataract surgery. Patient surveys show that postoperative pain is a strong predictor of how satisfied patients are with their cataract surgery experience.12
CONCLUSION
If taking steps toward preventing pain after cataract surgery is not the standard of care quite yet, I would still argue that it is an important part of the best practices for ensuring patients’ satisfaction. Reducing the potential for postoperative inflammation may also influence outcomes. The recent addition of a new medication that is specifically indicated to prevent (rather than treat) pain as well as reduce inflammation offers another mechanism by which to improve patients’ experience.
1. Kumar CM, Eke T, Dodds C, et al. Local anaesthesia for ophthalmic surgery. Joint guidelines from the Royal College of Anaesthetists and the Royal College of Ophthalmologists London; 2012.
2. Gedde SJ, Lee Y. Ophthalmic anesthesia. In: Naseri A, ed. Basic Principles of Ophthalmic Surgery. 3rd ed. San Francisco; American Academy of Ophthalmology; 2015.
3. Yonekawa Y, Kim IK. Pseudophakic cystoid macular edema. Curr Opin Ophthalmol. 2012;23(1):26-32.
4. Henderson BA, Kim JY, Ament CS, et al. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007;33(9):1550-1558.
5. Loewenstein A, Zur D. Postsurgical cystoid macular edema. Dev Ophthalmol. 2010;47:148-159.
6. Flach AJ. The incidence, pathogenesis and treatment of cystoid macular edema following cataract surgery. Trans Am Ophthalmol Soc. 1998;96:557-634.
7. Abell RG, Allen PL, Vote BJ. Anterior chamber flare after femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2013;39(9):1321-1326.
8. Hovanesian JA, Sheppard JD, Trattler WB, et al. Intracameral phenylephrine and ketorolac (OMS302) during cataract surgery maintains intraoperative mydriasis and reduces postoperative ocular pain – integrated results from two pivotal phase 3 studies. J Cataract Refract Surg. 2015;41(10):2060-2068.
9. Florio V, Cowan L, Prusakiewicz JJ, et al. Ocular tissue distribution of ketorolac after administration of OMS302 to dogs during IOL replacement. Electronic poster presented at: ASCRS/ASOA Symposium and Congress; April 17-21, 2015; San Diego, CA.
10. BromSite [package insert]. Cranbury, NJ: Sun Pharmaceutical Industries, Inc.; 2016.
11. Hosseini K, Walters T, DaVanzo R, Lindstrom RL. A randomized double-masked study to compare the ocular safety, tolerability, and efficacy of bromfenac 0.075% compared with vehicle in cataract surgery subjects. Clin Ophthalmol. 2016;21(10):2311-2317.
12. Fung D, Cohen MM, Stewart S, Davies A. What determines patient satisfaction with cataract care under topical local anesthesia and monitored sedation in a community hospital setting? Anesth Analg. 2005;100(6):1644-1650.




