A 34-year-old male engineer presents for LASIK. The patient only wears glasses because he lives at high altitude and cannot tolerate contact lenses. He loves cycling and skiing and considers his glasses to be a limitation.
His eyeglass prescription is -3.50 -1.50 × 020 OD and -3.75 -150 × 150 OS. In the refracting lane, the patient’s manifest refraction is identical to his eyeglass prescription, correcting to 20/20 OU. The slit-lamp examination is completely normal, and the patient’s general and ocular health are excellent. He takes no medications, has no significant family history, and does not smoke. Pachymetry readings are 555 µm OD and 565 µm OS.
He has done his research and politely asks very specific questions regarding his suitability for LASIK based upon the images that were just taken of his eyes and the technology that you use. Additionally, you performed LASIK on his mother 15 years ago, and he is wondering how things have changed since then.
The following article breaks from the usual format of the “Refractive Surgery Complex Cases Management” column. Instead of exploring the management of complications, this month’s article instead seeks to provide insight into the complexity of both the preoperative evaluation and discussion with a patient. A second article on this subject will appear later this year. For practical purposes, this initial piece concentrates on the patient’s questions regarding the image of his left eye (Figure). Although the answers pertain specifically to the iDesign Advanced WaveScan Studio System and Star S4 IR excimer laser (Johnson & Johnson Vision), the principles apply across the board.
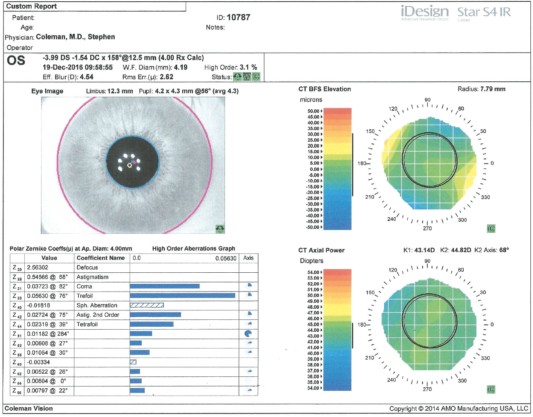
Figure. Measurements of the patient’s left eye with the iDesign Advanced WaveScan Studio and Star S4 IR excimer laser.
Patient’s First Question: My mom is very happy, but I do have a few questions. Looking at this picture of my eye, what do the numbers at the top left mean?
Dr. Coleman: That is your prescription, as determined by measuring the wavefront of your eye. This instrument directs an invisible infrared light to the back of your eye, and the emerging wavefront—or bundle of light photons—is captured and then calculated. As you can see, the measurements are made in increments of hundredths, not the 0.25 D steps that are typical for contact lenses and glasses. The measurement for your left eye or OS reads -3.99 DS -1.54 DC × 158º @ 12.5 mm (4.00 Rx Calc). This is a prescription based on a wavefront measurement, not a manifest refraction; it has been found that there is greatest correlation between the two (ie, when sitting in an examining room as opposed to sitting at an instrument) when the comparison is made using a 4-mm pupillary size.
In other words, this instrument is telling me what your exact prescription should be, based on the way your eye is, as opposed to your telling me what looks better when you are looking at an eye chart and answering the question, “Which is better, one or two?” That is how I determined your mom’s prescription. Today, we do it a little differently but still validate a person’s prescription by having him or her sit in a chair and answer the “which is better” question. Does that make sense? There is a lot of redundancy built into LASIK, lots of instruments, reading of old prescriptions, and looking at previous contact lens prescriptions, for example. Sometimes, some or none of these is available, but we do our best.
Patient’s Second Question: Thanks for explaining that. It seems that those measurements could be more accurate. What about the other numbers directly below the wavefront measurement?
Dr. Coleman: There is a time stamp to document that you are here now. The W.F. Diam (mm) 4.19 refers to the wavefront diameter in millimeters and reflects the size of the area where the wavefront information could be captured. It is usually very close to the size of your actual pupil. High Order 3.1% is a measurement of the part of your prescription that is not being addressed by your current glasses. Doctors refer to your nearsightedness and astigmatism as lower-order aberrations, those that we have been aware of and have been able to measure for a long time and that largely account for why you see the way you do. This instrument measures additional aspects of your prescription that are listed in the graph at the lower left of this image that we can talk about in a minute if you would like.
The Eff. Blur in the next line, 4.54, is shorthand for effective blur and represents the power of your eye in diopters as a single number, taking into consideration all of the aberrations of your eye, not just the nearsightedness and astigmatism. It is the same as what doctors refer to as spherical equivalent when determining the overall power of a person’s prescription using only nearsightedness and astigmatism. Effective blur is an aid to assessing the qualitative impact of the way higher-order aberrations affect how you see.
Patient’s Third Question: I do marathons. Is a diopter or “D” a unit that describes what it would take for me to get to the finish line?
Dr. Coleman: Good analogy. Eye doctors use diopters as a unit of measurement to determine what it takes to get a patient to 20/20, the finish line, or oftentimes beyond.
Patient’s Fourth Question: What does Rms Err.(µ): 262 mean?
Dr. Coleman: As an engineer, you actually may know more about this than I do, but it is the root mean square error, expressed in microns, for your left eye. This is a mathematical way of saying that an ideal wavefront would be flat and that, if a person sat at this instrument and we measured the emerging wavefront, the number would be zero if the patient had no prescription. The root mean square error is the difference between your measured wavefront and that of an ideal wavefront. The green status bars to the right of that allow the technicians to validate the accuracy of the pictures that they have just taken. The first bar confirms that the correct eye was imaged, the second bar confirms that the wavefront has been properly captured, and the third bar documents that the image has been properly centered.
Patient’s Fifth Question: The picture of my eye is really clear. What do those numbers right above it mean?
Dr. Coleman: The limbus, measured at 12.3 mm for your left eye, represents the border of your cornea, the clear part of your eye, and the sclera, which is the white part of your eye. A laser only affects a portion of the clear part, the cornea. We measure this primarily to assist the sophisticated tracking and guiding systems that lasers use during a LASIK treatment today. Your pupillary measurement has an average of 4.3 mm, and the exact measurements reflect the fact that not all pupils are perfectly round. Most are a bit elliptical, as yours is, and completely normal. This is all different from when your mother was here.
Patient’s Sixth Question: I am familiar with graphs as an engineer. What about the measurements on the lower left?
Dr. Coleman: That is a great question, one that most people do not ask, but this information can greatly help me to determine if and when a patient should have LASIK. The table represents the way that you see in mathematical terms. We use Zernike coefficients to deconstruct a patient’s wavefront. Defocus is the way laser doctors refer to nearsightedness, which is the primary reason that your vision is blurry, as indicated by the largest number, 2.56302. The second number, astigmatism, 0.54566, also contributes significantly to your vision. These are lower-order aberrations that are a part of your eyeglass prescription. Correcting these helps you to see better. In addition, your eye has imperfections that, on a smaller scale, blur your vision, as you can tell by the numbers. These include Zernike terms such as trefoil, spherical aberration, second-order astigmatism, and tetrafoil. Until recently, we have been unable even to measure these small imperfections in shape, but with wavefront technology, we are able to do so and hope to be able to consistently treat them with a laser.
Patient’s Seventh Question: How about the right side of this picture?
Dr. Coleman: We will go through that the next time I see you, and I will bring some friends on board.