
In the early days of endothelial transplants, making a graft for Descemet stripping automated endothelial keratoplasty (DSAEK) required an equipment investment that was too large for most individual surgeons. The grafts also took hours to prepare. Eye banks therefore began preparing the tissue, and these institutions continued to provide prepared tissue as many of us surgeons went on to embrace Descemet membrane endothelial keratoplasty (DMEK).
Eye banks acquire and process donor corneal tissue, cut it to the surgeon’s desired size, mark it for accurate placement, and load it in an insertion device. By taking those four steps out of our hands, eye banks saved us hours of time and eliminated our risk of losing money if we damage the tissue ourselves during preparation.
AT A GLANCE
• Pre-Descemet endothelial keratoplasty (PDEK) offers all the advantages of Descemet membrane endothelial keratoplasty and Descemet stripping automated endothelial keratoplasty with none of their disadvantages.
• Recently, as a collaborative innovation to advance PDEK, the first prepared graft for the procedure was jointly produced by two nonprofit organizations with a shared mission to restore sight to the blind and visually impaired. As more partner eye banks offer prepared PDEK grafts, a larger number of patients may be able to undergo the procedure.
• The author believes PDEK will become the corneal transplant procedure of choice, particularly for patients with a history of complex surgery or glaucoma.
Now, we are learning the advantages of another procedure, pre-Descemet endothelial keratoplasty (PDEK). In addition to endothelium and Descemet membrane, PDEK grafts have a microscopic layer sometimes called the Dua layer. Recently, as a collaborative innovation to advance PDEK, the first prepared graft for the procedure was jointly produced by two nonprofit organizations with a shared mission to restore sight to the blind and visually impaired: Vision Share (www.visionshare.org), a global leader in eye banking and advancing new transplantation procedures, and the Lions Eye Institute for Transplant & Research (LEITR; www.lionseyeinstitute.org), one of the world’s largest combined eye banks and research centers, located in Tampa, Florida.
As more partner eye banks offer prepared PDEK grafts, a larger number of patients may be able to experience the advantages of the procedure.
ADVANTAGES OF PDEK
PDEK offers all the advantages of DMEK and DSAEK with none of their disadvantages. Like DMEK, PDEK offers faster recovery and better visual results than traditional full-thickness corneal transplantation. PDEK also has a low rejection rate. The frequency of steroid drops decreases within a few months, and full weaning from steroid drops in a year or less is expected.
Unlike DMEK, PDEK can be performed in patients who have undergone previous surgeries such as vitrectomy or Nd:YAG posterior capsulotomy. DSAEK is also an option for these patients, but they can get off steroids much sooner after PDEK than DSAEK, a crucial advantage for patients with glaucoma who can face uncontrolled IOP and additional surgery with prolonged steroid use.
A PDEK graft is thin and flexible, but it is thicker and stiffer than a DMEK graft, which makes the tissue easier to handle. In addition, without the need to select tissue from older donors for its stiffness, PDEK grafts can come from donors of any age. This expands the donor pool, allowing the use of younger grafts with more endothelial cells.
As PDEK becomes more widely used, I believe it will become the corneal transplant procedure of choice, particularly for patients with a history of complex surgery or glaucoma. The only limitations right now are the time required for the eye bank to process the tissue and a size limit of 7.5 mm for PDEK grafts.
CREATING A PDEK GRAFT
LEITR and Vision Share work closely with surgeons to innovate corneal transplantation. While working with these organizations on several projects, I discussed the use of PDEK in other countries and the need for commercially prepared PDEK tissue here in the United States. In response to my inquiries, individuals at LEITR explored the regulatory limitations to determine how to offer PDEK tissue commercially.
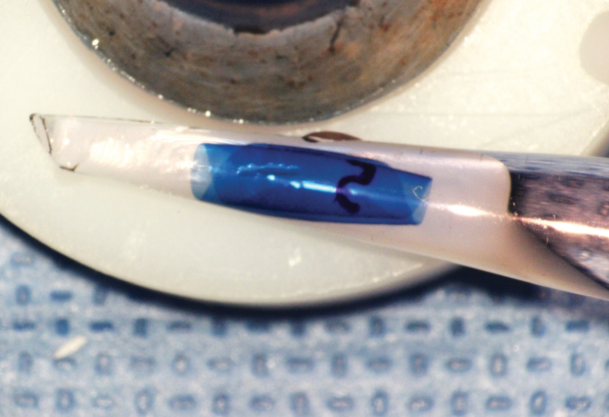
Figure. Stained, preloaded PDEK graft, prior to shipping to a surgeon from LEITR.
As part of the preparation, the graft is cut to the desired size, and the top is marked. The graft is loaded into an injector from which it will naturally unfold in the right configuration during surgery (Figure). Having the tissue preloaded in the injector and ready to unfold in the correct position saves time during surgery.
FIRST USE OF PREPARED PDEK GRAFT
I performed the first PDEK procedure using prepared tissue in a Canadian patient in her 60s who, in the winter, lives near my practice in Florida. She had previously undergone three failed corneal transplants, vitrectomy, and cataract surgery followed by an Nd:YAG capsulotomy. The patient was rejecting her most recent transplant so severely that she required high-dose steroids, which in turn resulted in glaucoma that was uncontrolled despite the use of three medications. After spending a great deal of money on this series of treatments, the patient also had a recurrent ulcer from inflammation and steroid use. The affected eye was red with a drooping eyelid.
After the second ulcer recurrence, I suggested that we try a different approach. I proposed clearing up the cornea with a PDEK graft and performing transscleral cyclophotocoagulation with MicroPulse technology using the Cyclo G6 Glaucoma Laser System (Iridex) at the same time, potentially reducing her need for both steroids and glaucoma medication. Given the patient’s past surgeries and glaucoma, I thought that PDEK was her only good option.
The corneal procedure was simple and took only about 10 minutes. The preparation and preloading of the graft made it easy for me to unroll the tissue in the right position.
Two months after surgery, the hyperemia and all of the patient’s side effects were gone. She was no longer taking steroids, and she required no topical glaucoma therapy. Her vision will require a longer recovery because of scarring.
CONCLUSION
The patient discussed herein had such a complex history it necessitated she have both PDEK and MicroPulse transscleral cyclophotocoagulation. The combined surgeries got the patient off steroids, controlled her glaucoma, and resolved the recurrent ulcers. This home run would not have been possible without the dedication of LEITR and Vision Share to continually improve the surgical options available to people who are blind or visually impaired.




