
Endocyclophotocoagulation (ECP) and the endoscope (Endo Optiks and BVI) needed to perform the procedure are great additions to the toolbox of any ophthalmologist caring for patients with glaucoma. Because IOP is the balance of how much aqueous is produced and how quickly it drains, clinicians can decrease pressure by reducing inflow, improving outflow, or a combination of both. ECP reduces inflow, and the procedure is especially useful in patients with narrow angles and mild to moderate disease. A randomized study compared 626 patients who received ECP at the time of phacoemulsification with 81 patients who underwent phacoemulsification alone.1 Three years postoperatively, the combined group demonstrated an 18% reduction in IOP in addition to a 58% reduction in the number of medications used, whereas the phaco-only group showed a 4% increase in IOP and no change in medication usage.
AT A GLANCE
• Endocyclophotocoagulation reduces aqueous inflow, and the procedure is especially useful in patients with narrow angles and mild to moderate disease.
• The author combines ECP with cataract surgery and microinvasive glaucoma surgery to maximize IOP control.
• The endoscope provides excellent visualization in many types of ophthalmic surgery.
When possible, I combine ECP with an iStent Trabecular Micro-Bypass Stent (Glaukos) to give my patients the synergistic benefit of an outflow and an inflow procedure in addition to the known IOP-lowering benefits of phacoemulsification. In my experience, combining procedures gives patients excellent IOP control and reduces the number of medications they require without affecting the safety profile of cataract surgery alone.
CAREFUL TECHNIQUE EQUALS BETTER OUTCOMES
Key to a smooth ECP procedure, I find, is always having an extra vial of viscoelastic on hand. After removing the cataractous lens and placing the IOL, I use viscoelastic to inflate the sulcus until I have excellent visualization of the ciliary processes (Figure 1). I position the laser close to the structures to increase the effect, and I maintain that same distance from each ciliary process. I have the laser on constantly but am very light on the pedal so that I can release it as soon as I see any whitening.
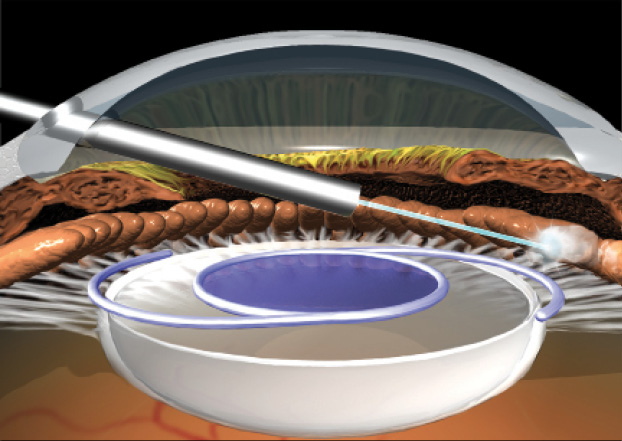
Figure 1. ECP performed over the IOL.
(Images courtesy of Endo Optiks and BVI.)

Figure 2. With treatment, the ciliary processes whiten and shrink.
The goal with ECP is to whiten and shrink the ciliary processes, not to maintain laser treatment until the processes pop (Figure 2). I find the latter to be too aggressive and to result in excessive inflammation and prostaglandin formation. A light cautery technique is much less proinflammatory. Again, clear visualization is essential, as is treating only the ciliary processes and not the posterior iris.
Although careful technique helps reduce inflammation, I prescribe aggressive prophylaxis. I ask the anesthesiologist to include methylprednisolone sodium succinate (Solu-Medrol; Pfizer) or hydrocortisone sodium succinate (Solu-Cortef; Pfizer) in the intravenous therapy administered, which gives an initial boost of anti-inflammatory medication. In addition, I typically prescribe difluprednate ophthalmic solution 0.05% (Durezol; Alcon) after surgery. I find that these steps suffice for nearly all patients if the technique is careful and are much easier than dealing with the bleeding or hyphemas that often follow more invasive glaucoma procedures.
ENDOSCOPE: RETURN ON INVESTMENT
Many of my colleagues do not appreciate the secondary gains of having an endoscope in their surgical suite. The instrument can be useful to all surgeons in a surgical center, not just those performing ECP. The endoscope is incredibly small and easy to use, and it permits surgeons to visualize areas of the eye that otherwise would be impossible to see.
Watch it Now
Mark Packer, MD, performs endocyclophotocoagulation as an adjunct to cataract surgery in a glaucomatous eye.
One example is a retained lens fragment that is difficult to locate, because it is in the sulcus or in the angle. The endoscopic camera makes it possible to visualize the sulcus directly. Similarly, many cataract surgeons work on sclera-fixated lenses. Even after measuring from the clinical scleral limbus where the entrance and exit points are, it is a relatively blind pass. The camera on the endoscope allows the surgeon to view the exact point of entry into the eye, thus providing assurance that the location is ideal and that no damage will be caused to the ciliary processes or the retina during entry or exit. In other cases, lens-based surgery must be performed despite corneal scarring or swelling, and the endoscopic camera will provide a clear view inside the eye.
THE FUTURE OF GLAUCOMA
Nonadherence to prescribed medical therapy is a notorious problem in glaucoma. I believe that treatment of this disease will become increasingly surgical in nature. A procedure that lowers IOP and reduces the burden of medication while maintaining a strong safety profile is a boon to patients and physicians. ECP, with its swift learning curve and high efficacy, is an excellent tool for all ophthalmologists.
1. Berke SJ, Sturm RT, Caronia RM, et al. Phacoemulsification combined with endoscopic cyclophotocoagulation (ECP) in the management of cataract and medically controlled glaucoma: a large, long term study. Paper presented at: American Glaucoma Society 16th Annual Meeting; Charleston, SC; March 4, 2006.
David A. Goldman, MD
• founder and CEO of Goldman Eye, Palm Beach Gardens, Florida
• (561) 630-7120; david@goldmaneye.com
• financial disclosure: consultant to BVI and Glaukos



