Case Presentation
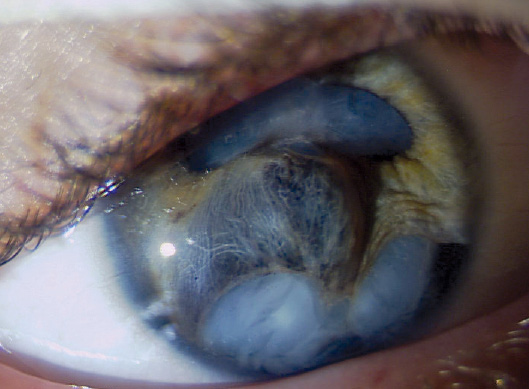
Figure 1. This 11-year-old boy developed a traumatic cataract after sustaining a BB gun injury to his right eye.

M. EDWARD WILSON, MD
This surgical case highlights some of the differences between blunt trauma in a child and the same injury in an adult. A child is more likely to get compression/rebound rupture of anterior segment structures and less likely to sustain a ruptured globe. Iridodialysis and a ruptured anterior lens capsule are common, and retinal dialysis is also seen at times. Hydrated lens material turns white quickly but does not usually cause sustained inflammation. As in this case, a delayed repair is best—after the initial hyphema and inflammation from the trauma have subsided. Because optical biometry is not possible, immersion A-scan and keratometry are used to select the IOL, with an aim, at this age, of emmetropia.
Briefly, my surgical approach would be as follows. Using blunt and viscodissection, I would sever the synechiae between the iris and the anterior lens capsule. I would repair the iridodialysis using 10–0 polypropylene horizontal mattress sutures and Hoffman pockets later in the surgery, after IOL placement.
I would perform bimanual irrigation and aspiration of the hydrated lens material (no phacoemulsification needed). I often use the opening of the ruptured anterior capsule to gain access to the lens material (it will have a fibrotic and stable edge) and will delay any capsulorhexis reshaping until later in the surgery.
I would remove vitreous; in cases such as this one, it has often prolapsed into the anterior chamber in areas of zonular rupture. In anticipation of vitreous-lens cortex admixture, I frequently pair the vitrector (25 gauge) with the bimanual irrigation handpiece. The vitrector can be easily alternated from aspirate-only for lens material to cut-and-aspirate when vitreous is present. This approach avoids the surprise of suddenly having vitreous engaged in the bimanual aspiration handpiece.
In-the-bag IOL implantation is usually possible in these cases. The pediatric zonule stretches and rebounds, often leaving less extensive zonular rupture than anticipated. Because each case is different, I would be prepared to use a variety of possible techniques to ensure the IOL's stability.
A primary posterior capsulotomy would need to be considered for this patient, because trauma cases (even at age 11) often develop fibrotic posterior capsular opacification soon after surgery.

LAMA AL-ASWAD, MD
The patient's visual potential is unknown, but it would be important to the give him the best possible outcome.
I approach cases such as this one by planning for phacoemulsification (most likely irrigation and aspiration because an 11-year-old cataract is soft even if it is traumatic) with the IOL placed in the bag or sutured to the sclera, depending on the status of the bag. Iridodialysis repair and goniosynechialysis will also be necessary.
My first step would be to inject triamcinolone acetonide (Kenalog; Bristol-Myers Squibb) to be sure that there was no vitreous in the anterior chamber that required an anterior vitrectomy. Next, I would evaluate the extent of the anterior capsular rupture and the stability of the zonules. I would then perform an ab interno iridodialysis repair with multiple McCannel sutures to facilitate access to the lens after performing anterior synechialysis to separate the iris from the capsule without tearing it.
I would perform gentle hydrodissection with balanced salt solution and then with an ophthalmic viscosurgical device (OVD) to support the lens in case of a posterior capsular rupture. I would remove the cataract with I/A using a low bottle height while evaluating the anterior capsule, posterior capsule, and zonules. If the capsule and the zonules were intact, then I would implant a single-piece IOL. A capsular tension ring (CTR) would be indicated if the zonules were compromised. If the posterior capsule has ruptured, then I would suture the IOL to the sclera. Finally, I would perform goniosynechialysis to remove obstruction to the trabecular meshwork, because the synchiae formed less than 6 months ago.

RICHARD J. MACKOOL, MD
Figure 1 displays a large inferior iridodialysis, and the inferior iris appears to be extremely thin and likely atrophic. Iridodialysis repair by suturing of the thin, dialyzed margin of the peripheral iris to the angle may therefore be difficult to achieve, and doing so may leave the patient with serious postoperative glare. To prevent this, the insertion of an artificial iris device (available with a compassionate use exemption) into the inferior lens capsule is likely to be required. Iridodialysis repair would then become less important, although it might still reduce glare by obstructing light rays that would otherwise pass beneath the inferior lens capsule/artificial iris and through the zonular region.
My approach would therefore be as follows and would depend greatly on the intraoperative findings. First, I would inject a highly retentive OVD, insert iris retractors through the inferior limbus to reposition the dialyzed iris, expand the pupil, and adequately expose the underlying cataract. Next, I would stain the anterior capsule by “painting” the dye directly onto the capsule with the side of the cannula. I would then identify the margins of the preexisting anterior capsular opening and, if possible, incorporate the defect into a capsulorhexis. If not, I would perform the capsulorhexis in a location that preserved anterior capsule for positioning of the artificial iris and IOL. If zonular deficiency were present, I would insert capsule retractors to stabilize the capsule-zonule complex before completing the capsulorhexis.
Using either an I/A tip or, more likely, a bimanual technique, I would aspirate the soft/mature cataract. If the zonule were deficient and I had successfully created a capsulorhexis, I would inject an OVD, insert a CTR, and then insert and suture one or two capsular tension segments to the sclera using either a polyester or Gore-Tex suture (W.L. Gore & Associates; off-label usage).
Next, I would insert the artificial iris device and either amputate the atrophic/dialyzed iris or, more likely, suture it to the region of the iris root. I find that using a gonioscopy lens permits accurate placement of the multiple double-armed sutures, thereby preventing the formation of anterior synechiae that compromise outflow.
I would insert the IOL into the capsular sac. I should note that, if zonular and/or capsular issues did not permit this, suturing a posterior chamber IOL to the sclera would be required.
The final step, if necessary, would be pupilloplasty by suturing. Depending on the pupil's size and location after execution of the previous steps, either a purse-string or interrupted (Siepser) suture(s) could be employed.

WHAT I DID: LISA BROTHERS ARBISSER, MD
I used mannitol 0.25 g/kg intravenous push as a bolus 15 minutes prior to the first incision. I instilled a dispersive OVD and painted trypan blue under the OVD onto the capsule through a small clear corneal incision to begin to define the capsular tear. I was careful to prevent dye from flowing posteriorly through the zonulolysis. Then, I used a “dry” manual technique under OVD control to aspirate flocculent lens material rather than irrigate any fluid, given the unknown nature of the zonulodialysis and status of the posterior capsule and because there was no possibility of a continuous anterior capsulorhexis. I took great care to keep the eye normotensive and to cover the area of possible zonulolysis with a dispersive OVD throughout. I used triamcinolone acetonide (Triesence; Alcon) diluted 1:10 with BSS Plus (Alcon) to try to identify any prolapsed vitreous (Figure 2).
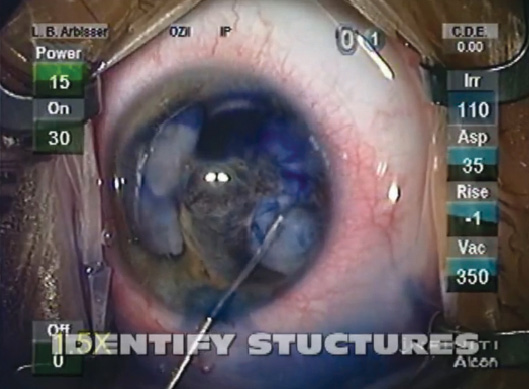
Figure 2. Dr. Arbisser used trypan blue dye to define the capsular tear and triamcinolone acetonide to try to identify any prolapsed vitreous.
As the lens material was aspirated, the posterior synechiae holding the dialyzed iris to the lens released, and gentle blunt and minimal sharp dissection reestablished normal planes to allow iris management. Using intraocular graspers, I gently pulled the superior iris in an attempt to open the superior angle and relieve peripheral anterior synechiae. To repair the iridodialysis, I placed two double-armed 10–0 Prolene horizontal mattress sutures (Ethicon) under a fornix-based flap. I draped the peripheral iris close to the scleral wall but allowed it to hang back enough to be clear of the trabecular meshwork. Then, I buried the knots. I used Vicryl sutures (Ethicon) to repair the fornix flap and securely cover the scleral sutures.
Inspection revealed a sufficient remaining envelope of anterior capsule for me to contemplate placing a three-piece IOL in the bag. The small zonulolysis remained stable, and I saw no vitreous prolapse. The posterior capsule remained essentially intact, and because the chamber was never allowed to shallow or deepen, the noncontinuous anterior capsular tears did not extend. I used two more 10–0 Prolene sutures with modified Siepser knots for a pupilloplasty, which covered the edges of the implant. Intracameral moxifloxacin hydrochloride (Vigamox; Alcon) and triamcinolone acetonide were instilled at the end of the case. Acetazolamide (Diamox; Wyeth Pharmaceuticals) appropriate to the patient's weight was given intravenously at the conclusion of surgery.
The patient did extremely well being slowly tapered off topical steroids, nonsteroidal anti-inflammatory drugs, and glaucoma medications. The IOP returned to normal off medication. His retina was normal, and I observed no peripheral abnormalities. His vision cleared to 20/60 with an opacifying posterior capsule.

Figure 3. Final result.
Three to 4 months postoperatively, I performed a Yag laser posterior capsulotomy on this cooperative boy. He rapidly achieved a UCVA of 20/25 and a BCVA of 20/20, and he received a prescription for progressive addition polycarbonate lenses. His family understands that they must be vigilant for traumatic glaucoma for his lifetime (Figure 3).
Both excellent cosmetic and functional outcomes can be achieved in cases such as this one by
• allowing a traumatic eye to calm first
• avoiding irrigation and turbulence
• identifying structures and reestablishing normal planes and relationships
• keeping the eye normotensive and preventing chamber collapse
• exposing the trabecular meshwork to permit function
• avoiding cautery
• never placing a single-piece lens where it can cause iris chafing
• restoring iris position n
Section Editor Lisa Brothers Arbisser, MD
• emeritus position at Eye Surgeons Associates, the Iowa and Illinois
Quad Cities
• adjunct associate professor, John A. Moran Eye Center, University
of Utah, Salt Lake City
• (563) 343-8896; drlisa@arbisser.com
• Financial disclosure: None acknowledged
Section Editor Audrey R. Talley Rostov, MD
• private practice with Northwest Eye Surgeons, Seattle
M. Edward Wilson, MD
• Miles professor of ophthalmology and pediatrics, Storm Eye
Institute, Medical University of South Carolina, Charleston
• (843) 792-7622; wilsonme@musc.edu
Lama Al-Aswad, MD
• assistant professor of clinical ophthalmology, Edward S. Harkness
Eye Institute, Columbia University College of Physicians and
Surgeons, New York
• (212) 305-1400; laa2003@columbia.edu
• Financial disclosure: None acknowledged
Richard J. Mackool, MD
• director, Mackool Eye Institute and Laser Center,
Astoria, New York
• (718) 728-3400, ext. 256; mackooleye@aol.com
• Financial disclosure: None acknowledged


