Today, refractive cataract surgery generally produces excellent visual results, but its refractive predictability, although usually very good, lags behind that of laser refractive surgery. Patients' expectation of spectacle independence after cataract surgery continues to grow, however, especially among those who pay for premium lens implants. Likewise, cataract patients who previously underwent refractive surgery expect excellent visual acuity without correction. For these reasons, ophthalmologists must be able to provide their patients with precise laser vision correction to improve their UCVA after cataract surgery as needed.
Ophthalmologists should wait 1 to 3 months after the cataract procedure so that the patient's postoperative refraction will have stabilized and they can make an accurate assessment. With the Crystalens (Bausch + Lomb), surgeons should wait 3 months and then perform a YAG capsulotomy prior to a refractive corneal procedure, because the IOL's position can shift, resulting in a change in refractive error. A stable refraction should be documented at a minimum of two postoperative visits. Surgeons should also carefully evaluate patients' astigmatism using corneal topography and corneal elevation mapping.
Multiple options are available for refactive correction depending on the patient's residual refactive error, the stability and type of lens implant, and the overall health of the eye and the ocular surface. They include IOL exchange, piggyback IOLs, peripheral corneal relaxing incisions, and laser vision correction. This article concentrates on the use of the excimer laser.
CHOOSING A PROCEDURE
Patients with a spherical equivalent near plano may be good candidates for peripheral corneal relaxing incisions to reduce their residual astigmatism. If they have significant myopia or hyperopia with or without astigmatism, laser treatment is a better option. Patients with low degrees of myopia, hyperopia, or astigmatism can benefit from either surface ablation/PRK or LASIK. High degrees of residual refactive error may carry a greater risk of haze formation from PRK that could decrease visual acuity; such patients do better with LASIK. High hyperopia is also corrected less predictably with PRK than with LASIK.
In patients with ACIOLs or a lens implant that may be unstable due to precarious placement in the sulcus, the suction required for LASIK should be avoided in favor of PRK. Some femtosecond laser platforms offer reduced suction pressure and could be an option in these cases.
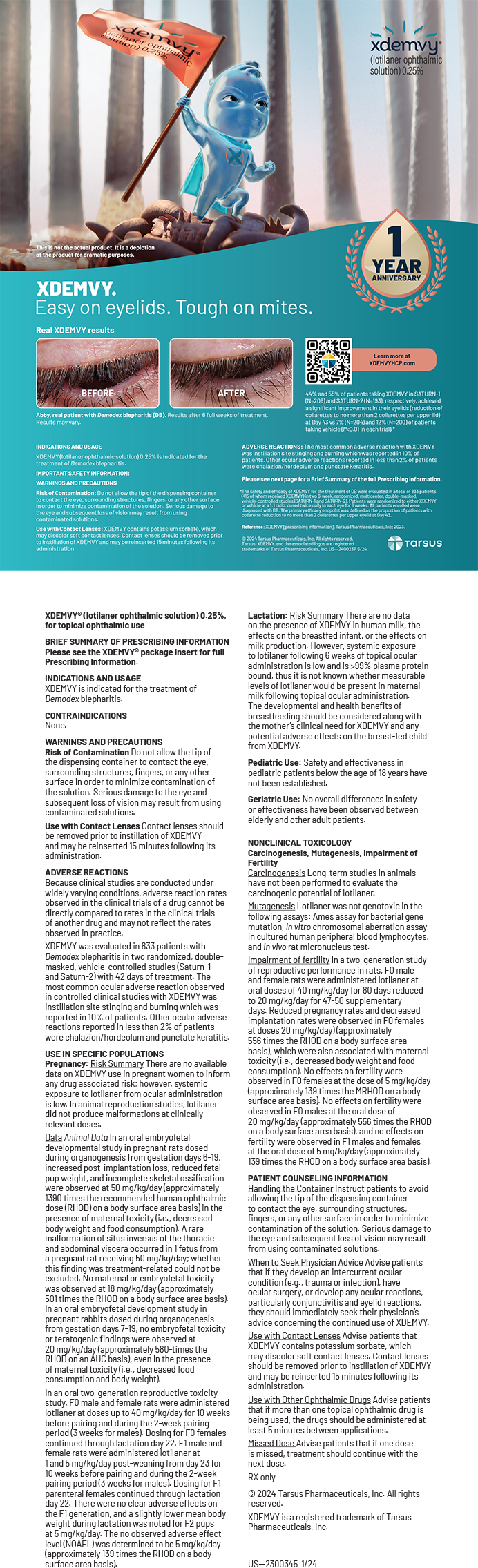
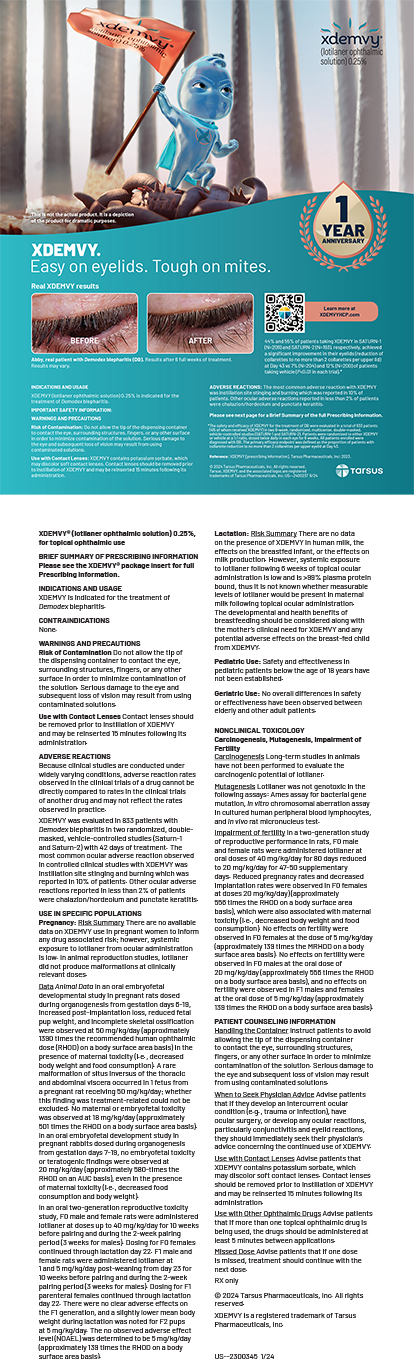
Finally, a thorough ocular examination is essential to assessing the complete health of the eye with a special emphasis on the ocular surface. Excessive meibomian gland disease and blepharitis can be treated preoperatively with eyelid hygeine, oral omega-3 supplements, topical azithromycin, and oral doxycycline or minocycline. If the eyelids cannot be adequately cleaned up, LASIK should be avoided. Physicians should also evaluate the health of the corneal epithelium and the tear film. Patients with evidence of significant dry eye disease need preoperative treatment with topical cylosporine, ocular lubricants, and possibly punctal occlusion. If the corneal epithelium continues to stain with either fluourescein or lissamine green dye, LASIK should be avoided. PRK may be performed selectively on these patients if the corneal staining is minimal.
DETERMINING THE TARGET
Calculating how much correction to program into the laser requires an accurate and stable refaction. Usually, the manifest refraction is sufficient, and a cycloplegic refraction is not nessessary after lens implantation. The surgeon should accurately assess the patient's visual requirements to determine if he or she desires distance vision without correction versus monovison with planned myopia in one eye. For patients receiving the Tecnis Multifocal 1-Piece IOL (Abbott Medical Optics Inc.), the author generally aims for very mild hyperopia such as +0.50 D versus -0.25 D with the Crystalens or AcrySof IQ Restor IOL +3.0 D (Alcon Laboratories, Inc.). Fortunately, most patients have a very low residual refractive error after cataract surgery, so the refractive target is easy to hit.
PAYING FOR AN ENHANCEMENT
The financial models for premium IOL patients differ among surgeons but generally take three forms. In the first, patients who choose a premium lens pay a higher price that includes the cost of a laser enhancement versus those undergoing cataract surgery with a standard monofocal IOL. The second model charges patients separately for postoperative LASIK only when it is needed, and the cost of the laser treatment is normally somewhat discounted from the usual LASIK price. In the third model, the cataract surgeon does not perform laser refractive surgery but refers the patient to colleagues who do. The primary cataract surgeon may cover all or part of the cost of the refactive procedure, or he or she may try to arrange a reasonable price that is charged by the refractive surgeon.
CONCLUSION
Laser vision correction after cataract surgery is a highly precise refractive option. Until ophthalmologists can acheive the same degree of refractive predictability from cataract procedures as from laser refactive surgery, their access to an excimer laser will continue to be important.
Jonathan B. Rubenstein, MD, is vice chairman and the Deutsch family professor of ophthalmology at Rush University Medical Center in Chicago. He is a consultant to Alcon Laboratories, Inc., and to Bausch + Lomb. Dr. Rubenstein may be reached at (312) 942- 2734; jonathan_rubenstein@rush.edu.