The concept of a drainage device to surgically manage elevated IOP in patients with glaucoma usually conjures up the image of a Molteno Implant (Molteno Ophthalmic Limited, Dunedin, New Zealand).1,2 This device is composed of a silicone tube, one end of which is placed in the anterior chamber of the eye while the other end is connected to a plastic plate or is implanted some distance from the limbus. Although originally intended for use in eyes with complicated and advanced disease, the popularity of drainage devices as an alternative to trabeculectomy grew. During the past few years, their usage has changed significantly based on the results of various multiyear studies.3 The term drainage device (also referred to as a tube and plate device and tube shunt) now encompasses a wide variety of treatment options. With the technology currently in a state of evolution, it is a good time to learn what surgeons are using and what may soon be available.
HISTORY
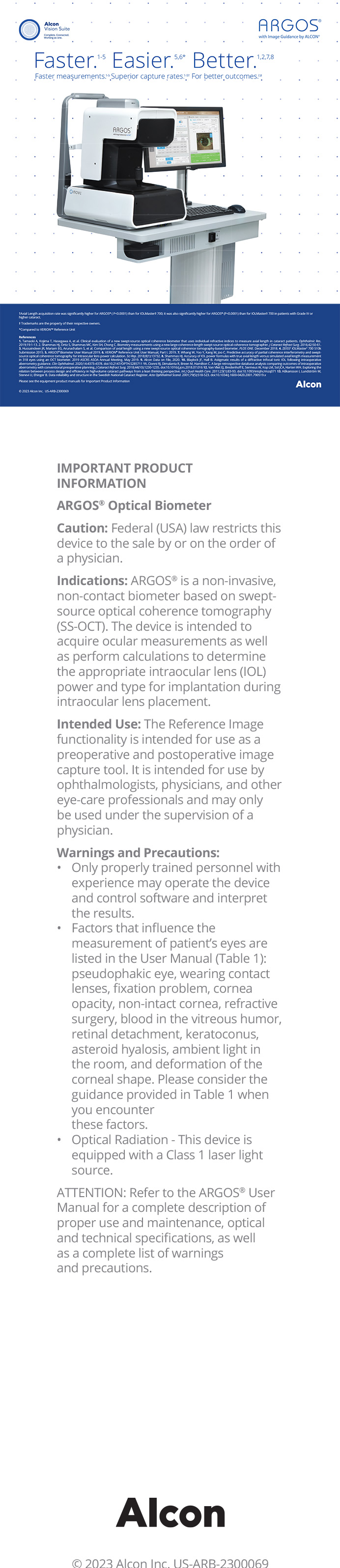
The original concept of a tube and plate device evolved soon after Tony Molteno, MD, introduced his implant in the early 1970s. In an effort to avoid the conjunctival erosion of the tube or plate, surgeons place the implant 10 mm from the limbus and cover the tube with a biologic tissue such as sclera, cornea, or pericardium. George Baerveldt, MD, recognized that the size of the plate matters and increased the surface area, which achieved greater pressure lowering.4 The double-plate Molteno Implant was developed for a similar purpose. With both devices, the open tube resulted in early postoperative hypotony unless the tube was temporarily occluded with absorbable sutures. Theodore Krupin, MD, and then A. Mateen Ahmed devised a modification of the valve at the base of the tube to prevent early hypotony. Currently, the single-plate Baerveldt glaucoma implant (Abbott Medical Optics Inc., Santa Ana, CA) and the Ahmed Glaucoma Valve (New World Medical, Inc., Rancho Cucamonga, CA) are the two most commonly used implants5 (Figure 1).
The indications for drainage devices have broadened during the past few years. Trabeculectomy was the gold standard for initial glaucoma surgery, and the use of drainage devices was limited to patients with a failed trabeculectomy or secondary glaucoma (ie, neovascular) for which trabeculectomy historically had a very low success rate. The landmark Tube Versus Trabeculectomy Study has helped to change this balance. The investigators randomized patients who required glaucoma surgery to either trabeculectomy with mitomycin C or a Baerveldt implant. The results showed that, despite a similar reduction in IOP and the use of supplemental medications, tube shunt surgery was more likely to maintain IOP control and to avoid persistent hypotony, the need for a reoperation for glaucoma, and a loss of light-perception vision than trabeculectomy with mitomycin C during the first 3 years of follow-up.6
TODAY AND TOMORROW
With broader indications and documented long-term advantages over trabeculectomy, drainage devices appear to be gaining in popularity among glaucoma surgeons. The trend has also encouraged the development of alternative devices. This technology has created new categories for IOP control. For example, the Ex-Press mini glaucoma shunt (Optonol Ltd., Neve Ilan, Israel) was designed to promote a more standardized trabeculectomy.7 The device features a 3-mm stainless steel tube with an outer diameter of 400 mm (Figure 2), and its external flange is designed to provide stability under the scleral flap in maintaining the sclerostomy. The efficacy of the device is similar to that of trabeculectomy, but when placed under a scleral flap, the former has fewer side effects.
Devices have also been developed for use in nonpenetrating surgery. The AquaFlow Collagen Glaucoma Drainage Device (STAAR Surgical Company, Monrovia, CA) is placed in the bed of the deep sclerectomy, adjacent to Descemet's window, to maintain the scleral lake. One of the more innovative devices in this category is the iTrack microcatheter (iScience Interventional, Menlo Park, CA) for use in the canaloplasty procedure. Upon identifying the canal space, the surgeon passes the microcatheter 360¼ along the canal and then attaches it to a 10–0 Prolene suture (Ethicon Inc., Somerville, NJ). As the ophthalmologist withdraws the microcatheter, he or she dilates the canal and collector system with viscoelastic. The suture is left in the canal to tension the meshwork and enhance aqueous outflow. The nonpenetrating procedure avoids the acute complications of filtering and tube shunt surgery, and 2-year data confirm the operation's efficacy.8,9
A number of drainage devices are in clinical trials. A trabecular-bypass approach with the iStent (Glaukos Corp., Laguna Hills, CA) shows real promise (Figure 3). This snorkel-shaped device is placed ab interno through the trabecular meshwork into the canal. Preliminary studies suggest that the iStent may have a role as an adjunct in cataract surgery.10,11 FDA approval is pending later this year.
The suprachoroidal space is another location under investigation by manufacturers. A device would be placed either ab interno or ab externo to allow aqueous egress into the suprachoroidal space.
CONCLUSION
Glaucoma surgeons have come a long way from simply creating a hole in the sclera and expecting a reduction in IOP from a bleb without scarring or other complications. Today, the term drainage device encompasses a broad range of surgical options that have enhanced outcomes while reducing side effects. The technology can only get better in the coming years.
Richard A. Lewis, MD, is in private practice in Sacramento, California. He is a consultant to Alcon Laboratories, Inc., and iScience Interventional. Dr. Lewis may be reached at (916) 649-1515; rlewiseyemd@yahoo.com.