CASE PRESENTATION
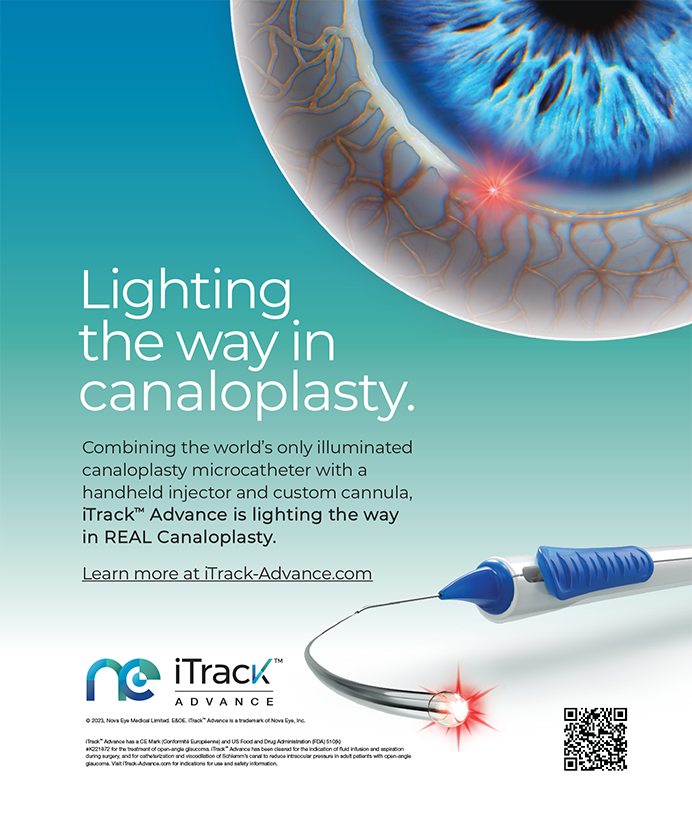
A 58-year-old male undergoes successful cataract surgery with the placement of an AcrySof Toric IOL (SN60T5; Alcon Laboratories, Inc., Fort Worth, TX) in one eye. The procedure almost completely eliminates his refractive cylinder and provides him with a UCVA of 20/20-1. During cataract surgery on his second eye, the posterior capsule ruptures as the surgeon is implanting the SN60T5 lens. The anterior capsulorhexis remains intact, but the posterior capsular tear is wide and extends across the entire posterior capsule (Figure 1).
How would you manage this case?
LISA B. ARBISSER, MD
The tear is unfortunately too extensive to be converted into a posterior curvilinear capsulorhexis. I would make a pars plana incision. With a bimanual approach using the vitrector posterior to the IOL's optic and a Sinskey hook through the paracentesis, I would slightly rotate the lens to match the dots to the marks for the steep axis while capturing the optic forward through the capsulorhexis and leaving the haptics in the bag (reverse optic capture). I would then instill washed Kenalog (preservative removed; Bristol-Myers Squibb, Co., Princeton, NJ) or Triesence (Alcon Laboratories, Inc.) through the paracentesis to be sure no vitreous was present around the edge of the IOL. I would amputate any connection posteriorly with irrigation through the paracentesis and the vitrector in the posterior segment always in full view. Assuming I used 20-gauge instrumentation, I would suture the sclerotomy and the peritomy with 8–0 Vicryl (Ethicon, Inc., Somerville, NJ). This approach should lead to a stable result with excellent management of the astigmatism.
I view the following alternatives as far less desirable. If the lens is left in position, fibrosis of the haptics might fortuitously secure the IOL in the bag. If there is no vitreous prolapse around the lens, the eye may do well. It will, however, be difficult to finish the case without any loss of anterior chamber stability, which will inevitably lead to vitreous herniation around the lens. I think the whole situation is too tenuous to depend on the lens' stability either intra- or postoperatively. In addition, this approach will resolve virtually none of the astigmatism, as the IOL is more than 10¼ off axis according to Figure 1. The surgeon will be unable to determine the final astigmatism intraoperatively, requiring subsequent treatment on the cornea according to the stable manifest refraction.
Another option is to remove the lens, because a one-piece acrylic IOL does not belong entirely in the sulcus. Compared with my preferred approach, explantation would pose a greater risk of vitreous traction, and a larger vitrectomy would likely be needed. A monofocal three-piece lens should be placed in the sulcus with the optic captured through the capsulorhexis for secure centration and stability. Using the topography and keratoscopy to guide a peripheral astigmatic keratotomy, I would then treat the corneal astigmatism after bringing the eye to a normotensive state while the patient was on the table. LASIK would be an option postoperatively if needed to optimize the refraction.
During cataract surgery, I routinely use dilute intracameral Vigamox (Alcon Laboratories, Inc.), but I would add one dose of oral moxifloxacin for prophylaxis, because there is a 10 times higher rate of endophthalmitis in cases complicated by anterior vitrectomy. I would expect a need for perioperative pressure control, particularly with the first option outlined for management, because a desire for low turbulence would necessitate an incomplete removal of the viscoelastic. Ultimately, the patient will likely do well but should have a retinal examination with scleral depression during the early postoperative period.
RICHARD E. BRAUNSTEIN, MD
The posterior capsular rupture precludes correct and stable positioning of the AcrySof Toric IOL. The area of capsular rupture suggests that the trailing haptic is currently not supported by any capsular remnant and may be in vitreous. Any attempt to rotate the lens toward the area of remaining peripheral posterior capsule will either enlarge the existing tear or result in increased residual astigmatism postoperatively. The lens should be explanted, because the single-piece AcrySof haptics can induce pigmentary dispersion and persistent inflammation when placed in the ciliary sulcus.
When removing the IOL, I would use a dispersive viscoelastic to try to tamponade the vitreous face and gently elevate the optic out of the bag. The lens could either be cut or folded and removed from the original incision, which could be enlarged slightly if necessary to facilitate atraumatic explantation. I would sweep the anterior chamber and inspect the wound carefully with a methylcellulose sponge to check for any vitreous in front of the anterior capsule. If vitreous were present, I would perform an anterior vitrectomy using a bimanual technique to drop the vitreous face posteriorly to allow for the IOL's safe placement in the ciliary sulcus. I would implant a three-piece foldable lens with an overall length of 13 mm and its power adjusted for placement in the ciliary sulcus.
I would address any residual astigmatism with surface ablation or LASIK 2 to 3 months postoperatively, depending on corneal thickness and topography. I would ensure refractive stability and proper wound healing prior to performing an additional refractive procedure.
JAMES A. DAVISON, MD
I will assume that the viscoelastic has largely been removed from behind the IOL's optic but that some of it remains in the anterior chamber. I will also assume that the anterior hyaloid membrane is intact and that both haptics are posterior to the anterior capsule. If an anterior radial tear had compromised the capsulorhexis' opening, I would recommend no additional rotations of the IOL.
Assuming an intact capsulorhexis, I would proceed as follows. First, I would lower the irrigation bottle to 50 cm above the eye but keep the irrigation flowing with the I/A tip in the anterior chamber as seen in Figure 1. Using a 3-mL syringe and a 30-gauge cannula, I would inject air into the anterior chamber at the paracentesis incision as I withdrew the I/A tip. The air would keep the chamber fairly full, thereby preventing capsular distortion and further disruption or prolapse of vitreous immediately after the I/A tip's removal. I would replace the air with ProVisc (Alcon Laboratories, Inc.) in a serial-exchange fashion—a little air withdrawn with the syringe and cannula followed by an injection of ProVisc. Three cycles of exchange would probably be required. I would leave the eye soft and the anterior chamber about 75% filled.
Next, I would gradually introduce a small amount of Viscoat (Alcon Laboratories, Inc.) underneath the IOL's optic and allow it to spread slowly across the anterior hyaloid membrane and push it slightly posteriorly. I would use just enough of the viscoelastic to create a normal anterior chamber depth and normal IOP. It is important at this stage not to overfill the anterior chamber.
By prying it forward with a cyclodialysis spatula, I would carefully prolapse the optic of the IOL anterior to the capsulorhexis' opening while trying to stay away from the anterior hyaloid membrane. Slowly, and with multiple steps, I would rotate the IOL the remaining 40¼ so that it was at the correct astigmatic orientation. By making many small movements, I should avoid having the posteriorly located haptics engage the posterior capsule in a significant way. It would be important, however, to watch for significant extensions in the posterior tear or any wrinkles or stress lines that might develop in the anterior capsule. I would stop rotating the lens if I encountered resistance or saw anything that might represent a threat to the anterior capsule's integrity.
After confirming that the bottle of balanced salt solution was located 50 cm above the eye, I would slowly re-enter the anterior chamber with the I/A tip to remove the viscoelastic. I would introduce air through the paracentesis incision as I withdrew the I/A tip and would make sure that the anterior chamber remained significantly formed. Using 30-gauge cannulas and 3-mL syringes, I would serially exchange the air for balanced salt solution. Upon confirming symmetric optic capture, I would pressurize the eye, complete stromal hydration of the incision, and again verify the optic's capture.
Six weeks after surgery, I would consider LASIK to treat the residual refractive error as needed, whether due to the optic's anterior location or incomplete rotation of the optic for astigmatic correction.
JOHN F. DOANE, MD
The first option would be to rotate the current lens clockwise approximately 30¼ to 40¼. Based on Figure 1, rotation might not leave enough posterior capsule for the IOL's long-term or rotational stability, because the midpoint of the one-piece IOL's acrylic haptic will be positioned at the apices of the posterior capsular tear. If by remote chance the IOL is stable after testing, expectant observation would be required to determine if the solution will be acceptable in the long term. I would inform the patient preoperatively that this approach is the least complicated as far as intervention but the least certain as far as long-lasting stability. I test stability intraoperatively by means of quick movements of the IOL in all directions after grasping the perilimbal area with two toothless forceps located 12 clock hours apart.
If at the time of the surgery after rotating the IOL I found it to be unstable, then I would remove the lens by bisecting it with Osher IOL Scissors (Storz item No. ET1306; Bausch & Lomb, Rochester, NY). I would have instructed the patient beforehand that I had two tasks to complete after removing the toric IOL. The first would be to place an appropriate three-piece IOL in the sulcus. A limited anterior vitrectomy might be necessary in this case, so it should be part of the consent process. The next step would be managing the corneal astigmatism. One approach would involve concurrent limbal relaxing incisions to treat the approximately 2.00 to 2.50 D of astigmatism. Alternatively, I could perform laser vision correction 6 weeks after surgery.
JOHNNY L. GAYTON, MD
I explain to patients with astigmatism that they are paying for astigmatic management. I then correct the astigmatism by "whatever means necessary." Patients understand that they may need laser ablation or relaxing incisions postoperatively in order to completely resolve their astigmatism. I also inform them that I may or may not use a toric lens. Explaining these matters preoperatively makes postoperative discussions much easier.
In this case, I am very concerned about the lack of support from the capsular bag. If the toric lens placed ultimately dislocates, the patient will be at high risk of developing cystoid macular edema or a retinal detachment. Usually, a small posterior capsular tear does not interfere with the use, positioning, and centration of a single-piece lens. In this case, however, the posterior capsular defect is so large that I would switch to a three-piece acrylic lens. I would place the IOL in the sulcus with the optic trapped by the anterior capsulorhexis.
In my hands, limbal relaxing incisions are not as predictable as toric lenses and are not as reliable in correcting 1.50 D or more of astigmatism, especially in young and middle-aged patients. Because this patient is 58 and has at least 2.00 D of astigmatism, I would plan to address his astigmatism with laser vision correction postoperatively, unless contraindicated by the eye's corneal thickness and topography. I evaluate patients' topography, tear film, and corneal thickness preoperatively. Consequently, I would know intraoperatively if laser vision correction were contraindicated. If it were, I would perform intraoperative limbal relaxing incisions. I would then address the residual astigmatism with an astigmatic keratotomy about 8 weeks postoperatively.
Both laser vision correction and incisional keratotomy will take several months to achieve the goal of minimal cylinder. The patient will therefore need a significant amount of handholding and explanation by the technicians and me. Every member of the clinical team will need to understand how astigmatism is managed so the patient is not given a confusing message. Ultimately, by these methods, the patient and I should be pleased with the final outcome.
Section Editors Robert J. Cionni, MD; Michael E. Snyder, MD; and Robert H. Osher, MD, are cataract specialists at the Cincinnati Eye Institute in Ohio. They may be reached at (513) 984-5133; rcionni@cincinnatieye.com.
Lisa B. Arbisser, MD, is a clinical adjunct associate professor with the John A. Moran Eye Center at the University of Utah in Salt Lake City, and she is in private practice with Eye Surgeons Assoc. PC in the Iowa and Illinois Quad Cities. She has received honoraria from Alcon Laboratories, Inc. Dr. Arbisser may be reached at (563) 323-2020; drlisa@arbisser.com.
Richard E. Braunstein, MD, is an associate professor of clinical ophthalmology with the Edward S. Harkness Eye Institute at Columbia University Medical Center in New York. He is on the speakers' bureau for Alcon Laboratories, Inc. Dr. Braunstein may be reached at (212) 326-3320.
James A. Davison, MD, is the president of Wolfe Eye Clinic in Marshalltown, Iowa. He is a paid consultant to Alcon Laboratories, Inc. Dr. Davison may be reached at (641) 754-6200 ext. 1025; jdavison@wolfeclinic.com.
John F. Doane, MD, is a clinical assistant professor with the Department of Ophthalmology at the Kansas University Medical Center in Kansas City, and he is in private practice with Discover Vision Centers in Kansas City, Missouri. He acknowledged no financial interest in the products or companies mentioned herein. Dr. Doane may be reached at (816) 478-1230; jdoane@discovervision.com.
Johnny L. Gayton, MD, is in private practice with EyeSight Associates in Warner Robins, Georgia. He is on the speakers' bureau for Alcon Laboratories, Inc. Dr. Gayton may be reached at (478) 923-5872; jlgayton@aol.com.