In the early 1940s, Tsutomu Sato, MD, of Tokyo, Japan, attempted to correct the refractive error of a myopic patient by making a series of incisions on the endothelial surface of the cornea. The treatment was later found to damage the cornea, and the procedure was abandoned. In the 1970s, Svyatoslov N. Fyodorov, MD, of Moscow, Russia, discovered serendipitously that the tiny cuts made by shards from a broken eyeglass actually improved a 13-year-old boy's nearsightedness. Intrigued by this unusual finding, Dr. Fyodorov set out to create purposeful radial incisions in the cornea in order to flatten and reshape it. In so doing, he pioneered what would become an entirely new field of ophthalmology: refractive surgery.
In 1976, researchers at IBM (Armonk, NY), seeking a more economical method for creating microchips for the burgeoning computer industry, created a new wavelength of laser light (193 nm). They named it excimer, because the wavelength originated from an excited dimer of argon and fluorine gases. This wavelength was soon adapted for reshaping the cornea with a laser, and, when later combined with the microkeratome, an entirely new field of laser refractive surgery emerged—LASIK.
Today, ophthalmologists can correct myopia, hyperopia, and astigmatism with a combination of incisions, laser applications, and/or implantable IOLs and have thereby eliminated the need for eyeglasses and contact lenses for millions of people. Despite incredible technological and medical advances, a large proportion of patients over the age of 40 still require spectacle correction after refractive surgery due to presbyopia.
DEFINING PRESBYOPIA
To understand current approaches to the surgical treatment of presbyopia, we first must define the condition. Presbyopia literally means “old eyes” and refers to the loss of accommodation that occurs with aging. The anatomical and physiological changes that occur with accommodation (miosis and convergence) increase the power of the natural lens and enable eyes to focus at near. The amplitude of accommodation, however, decreases from birth to the age of 75 years.
Most people notice the effects of this loss of accommodation by the age of 45. So predictable is the loss of accommodative amplitude that physicians can estimate an individual's age by the amount of residual accommodation (3.5 D at 45 years of age, 1.75 D at 55 years of age, and 0.5 D at 65 years of age). By the age of 75 years, a person has no measurable amplitude of accommodation at all.
Does this increase in lens power result from axial movement of the lens or a change in its shape? Research has demonstrated the latter in the form of a forward bulging of the lens' anterior surface. German scientist Hermann von Helmholtz, MD, theorized that the lens increases its anterior curvature by contracting the ciliary body in response to a blurred image on the retina. The contraction of the longitudinal muscle fibers of the ciliary body, in turn, constricts the ciliary ring and thereby relaxes the tension on the zonules of the crystalline lens. As a result, the lens becomes rounder with more plus power.
According to the standard, accepted theory of Dr. Helmholtz, as the human crystalline lens ages, it becomes more sclerotic, resists deformation, and, therefore, becomes incapable of increasing its anterior curvature. Recently, Ronald A. Schachar, MD, of Dallas, Texas, proposed that this loss of accommodation is instead due to the increased size of the crystalline lens. He holds that, as the lens grows over time, crystalline fibers are laid down at the equatorial zone, much like rings on a tree. According to Dr. Schachar, by the time a person reaches 40 years of age, enough lens material has accumulated within the capsular bag that little room remains within the ciliary space for lens movement. If his theory is correct, increasing the ciliary space may allow the restoration of accommodation.
CORRECTIVE MODALITIES
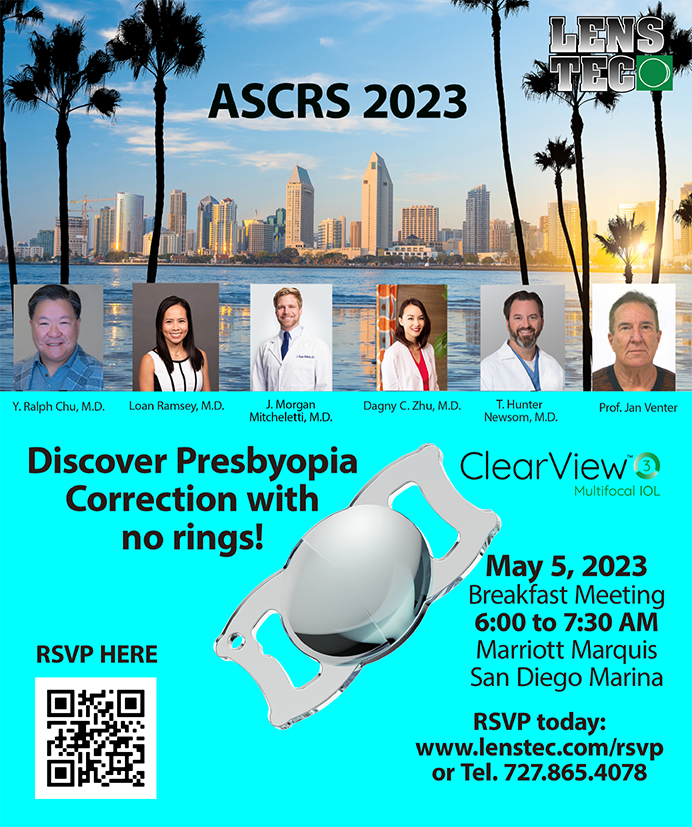
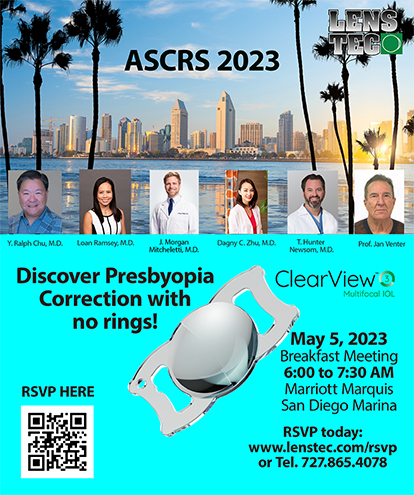
Ophthalmologists currently have five different approaches for the treatment of presbyopia: (1) bifocal/trifocal spectacles and bifocal/multifocal contact lenses; (2) anterior sclerostomy, or surgical incisions into the sclera overlying the ciliary body as a means of enlarging the ciliary space and facilitating movement of the lens; (3) the implantation of scleral expansion segments into four quadrants of the sclera overlying the ciliary body in order to increase the ciliary space; (4) the implantation of an accommodative IOL or of an IOL with a bifocal, multifocal, or toric optic (Figure 1); and (5) the application of laser or thermal energy to the cornea in order to make it aspheric in shape.
In part because patients frequently find spectacles or contact lenses inconvenient, ophthalmologists continue to seek an effective surgical means of correcting presbyopia. The techniques for anterior sclerostomy are still in the early stages of development, and we do not yet know the procedure's long-term results and benefits (Figure 2). Incisions into the cornea or sclera may cause healing difficulties, unnecessary weakening, or regression. We also do not know the long-term effects of exposing the uvea. Scleral expansion segments, meanwhile, pose new challenges in surgical technique, and patients may not accept the procedure's cosmetic outcome. These efforts to expand the ciliary space show promise, however, and deserve continued investigation.
Although the laser or thermal alteration of the corneal surface may be another method of restoring near focus, the challenges in altering the cornea pose some risks, such as irregular astigmatism, corneal damage, a regression of effect, and a lack of predictability. Procedures that could steepen and create an aspheric cornea, such as thermal keratoplasty, might be beneficial if they could be tailored to create the desired effect without these risks. Additionally, excimer laser technology may one day allow surgeons to etch a bifocal optic onto the corneal surface in order to improve the range of focus, but at present this technology is in its infancy.
Bifocal and multifocal lens implants have proven to be less than satisfactory so far. These IOLs must accomplish the challenging task of improving the range of vision while minimizing the potential for aberrations created by splitting light into several points of focus, which results in a loss of contrast. Aspheric IOLs show much promise in their ability to overcome these drawbacks. The toric IOL, by contrast, has been shown to improve the range of focus in the pseudophakic patient, and patients with pre-existing astigmatism may achieve some degree of pseudoaccommodation with these lenses. The future of presbyopic surgery may be an IOL that can either change position or increase power in response to a stimulus. Investigators are rapidly developing new lens designs that may restore accommodation. Without question, newer modalities of presbyopia surgery, including microchips, nanomotors, and materials not yet imagined, will solve today's challenges.
When we develop a successful surgical treatment for presbyopia, we will have achieved the total refractive correction of the eye, yet it may only be the beginning.Robert M. Kershner, MD, FACS, is Director of the Eye Laser Center in Tucson, Arizona. Dr. Kershner holds no financial or proprietary interest in any of the techniques or devices described in this article. He may be reached at (520) 797-2020; kershner@eyelasercenter.com.