
One of the most difficult things to assess is the quality of vision patients are experiencing. Owing to the array of diagnostics available for use in the clinic, the eye care field has become proficient at detecting cataracts, presbyopia, dry eye disease (DED), and other causes of refractive error. Incredible advances in surgical technologies have provided new ways to address these issues, yet missing has been an ability to understand how well the optical system is working as a whole. Absent that piece of the puzzle, we have become quite able to achieve 20/20 outcomes (or close) after cataract or lens surgery, primary refractive procedures, and a host of combined procedures, but we may not always optimize the quality of that vision.
AT A GLANCE
• One of the most difficult things to assess is the quality of vision patients are experiencing. Owing to the array of diagnostics available for use in the clinic, the eye care field has become proficient at detecting cataracts, presbyopia, dry eye disease, and other causes of refractive errors.
• The AcuTarget HD instrument directs a low-level laser to the back of the eye and measures the amount of light that returns by way of a double-pass system. The integrated software analyzes the amount of dropout to provide a measurement of the total optical system’s performance.
• An obvious application of OSI is for cataract patients, particularly to detect dysfunctional lens syndrome so that early intervention can be planned.
QUALITY OF VISION
Much discussion recently has centered on improving surgeons’ ability to hit the refractive target precisely, accurately, and repeatedly. In cataract surgery, improvements have elevated the likelihood of improved postsurgical vision. In refractive surgery, that outcome is an expectation, and anything short of the best vision possible may be considered a failure. Similarly, advances in the correction of presbyopia have helped to provide functional near and distance vision to patients. Expectations of improved postsurgical vision almost regardless of the procedure being performed have yielded a greater emphasis on the quality of the resulting vision.
In short, patients do not just want 20/20 vision; they want to be 20/happy. In my view, this changing paradigm provides a strong rationale for understanding the optical quality of our patients’ visual systems using ocular scatter index (OSI) testing. The AcuTarget HD instrument (AcuFocus), the tool I use to measure OSI, is currently thought of as useful for assessing dry eye disease and looking for early cataracts. There may be additional indications for this diagnostic tool, however, that will ultimately help clinicians design treatment plans that address both the quantity and the quality of refractive correction.
BACKGROUND
The AcuTarget HD instrument directs a low-level laser to the back of the eye and measures the amount of light that returns by way of a double-pass system. The integrated software analyzes the amount of dropout to provide a measurement of the performance of the total optical system. In the setting of perfect axial alignment with no opacities and no irregularities that would disrupt the transmission of light, the amount of returned light would be equal to the amount projected. In the presence of cataracts, astigmatism, aberrations, vitreous opacities, or other abnormalities, OSI provides a quantitative assessment of the visual system’s overall ability to project and receive light.
What is important to understand about the AcuTarget HD instrument is that, although the principle is to measure backscattered light, the analysis is based on what is occurring at the retinal plane. As a result, OSI gauges what a patient is seeing considering all the various elements of his or her visual system.
Originally, the AcuTarget HD instrument was developed by AcuFocus in collaboration with Visiometrics for the purpose of facilitating patient selection for the Kamra inlay (AcuFocus). Because the inlay uses a 1.6-mm aperture, any opacities or irregularities in the central portion of the cornea will negate its effectiveness. In addition, even small amounts of DED in that central region will dramatically affect the implant’s ability to restore near vision. Thus, OSI helps to screen out patients who are unlikely to benefit from the inlay as well as to identify others who may benefit from additional corrective measures to optimize the visual plane before they receive the inlay.
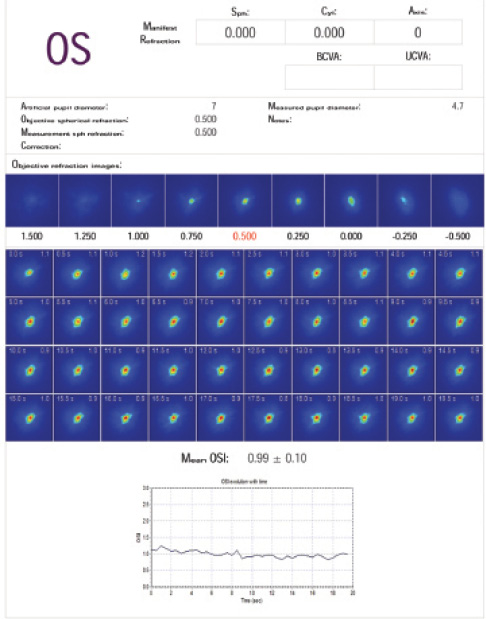
Figure 1. Normal tear examination.
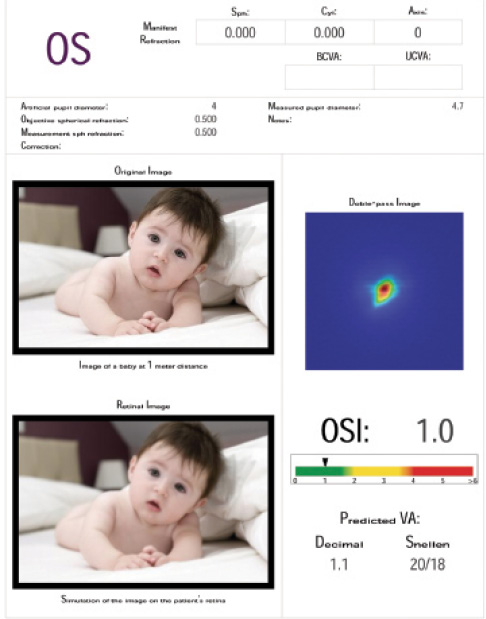
Figure 2. Normal OSI scan.
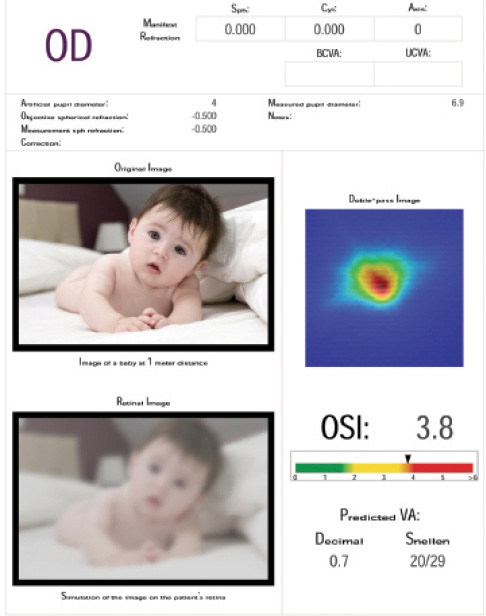
Figure 3. Abnormal OSI scan showing lenticular changes.
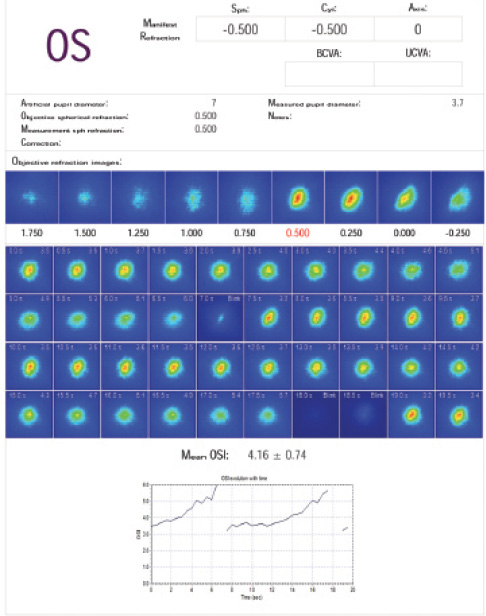
Figure 4. Sawtooth abnormal tear scan.
OTHER APPLICATIONS
Many patients who underwent refractive surgery are now presenting with various stages of presbyopia to seek an enhancement of their overall vision. Using the OSI in conjunction with topography, the surgeon can decide whether the patient will be best served by an inlay, monovision, or refractive lens exchange. For example, a patient who has a normal topography and a normal AcuTarget HD DED test but an overall increased OSI has dysfunctional lens syndrome and is probably best suited for refractive lens exchange. If the same patient has a normal OSI score, he or she may be a good candidate for the Kamra inlay or a monovision adjustment. A poor DED test should raise concerns about choosing a multifocal IOL. IOL calculations may not be as accurate as desired, and the quality of the postoperative vision may be compromised.
One of the more obvious applications of OSI is for cataract patients, particularly to detect dysfunctional lens syndrome so that early intervention can be planned. The ability of presbyopia-correcting IOLs to achieve an optimal refractive outcome depends on whether any issues (ie, in the cornea, at the lens, or in the vitreous) are affecting the optical system’s ability to refract light. This raises the example of the patient who presents with a degree of vision loss that does not quite correlate with the severity of the cataract. If the OSI indicates an issue that does not match what would be expected based on the media opacity, further investigation may be warranted.
Premium IOL patients may benefit tremendously from OSI testing. Typically, they have very high expectations of a truly refractive outcome. Before surgery, OSI can help detect poor candidates for a premium IOL and patients who may have DED that needs to be treated. After surgery, OSI can help determine why a patient did not achieve his or her refractive goal.
In the DED testing mode, the instrument takes a reading every 0.5 seconds for 30 seconds to provide an assessment of the health of the tear film over time. This information can be additive in the assessment of suspected DED, but it may be even more important in surgical patients. With a healthy tear film, the resulting test will produce a flat line because of a steady surface index. If DED is present, however, the test will result in a sawtooth-appearing pattern: the index climbs with evaporation of the tear film (peak) and drops when the patient blinks to restore it (valley). If a DED pattern is detected in a multifocal IOL candidate, I know I have to delay surgery and address the issue (Figures 1-4). I also know that biometry, keratometry, and topography readings are going to be prone to error.
CONCLUSION
In my colleagues’ and my practice, the AcuTarget HD instrument is a dynamic testing tool that we use frequently to determine the best course of corrective action. With a post-LASIK patient looking to optimize his or her vision, for example, the results of OSI testing may help us determine whether to pursue a lenticular or a corneal procedure. Using the instrument in regular practice, however, comes with important caveats.
OSI is excellent at showing the effect of the total optical system. Aberrations, dry eye, opacities, and corneal scars do not compromise testing accuracy; instead, the potential presence of these issues is the very reason to perform the testing. However, OSI must be paired with other diagnostic modalities to reap the full benefit. It flags an optical problem as well as provides an index of its severity but does not indicate the nature of the issue or where it is located. When used in conjunction with other testing platforms and the clinical workup, OSI testing allows me to home in on the real source of the problem so that I can plan appropriate correction. The additional information provided by the AcuTarget HD instrument will ultimately provide a means to plan corrections that consider both the quantity and the quality of the final outcome.
Alan R. Faulkner, MD
• founder and physician CEO with Aloha Laser Vision in Honolulu, Hawaii
• (808) 792-3937; dralan@alohalaser.com
• financial disclosure: consultant to AcuFocus, speaker/consultant to Alcon; speaker for Bausch + Lomb; a participant in clinical trials for Refocus,; a shareholder in Strathspey Crown/Alphaeon


