

Electroretinogram (ERG) testing has largely been confined to laboratory and clinical study settings. The need to program parameters (eg, luminance level, stimulus type, pattern size) specific to the pathology of interest into the test has been overly burdensome for ERG testing to be practical for daily use. The availability of a mobile ERG unit (Diopsys NOVA ERG and VEP Vision Testing System; Diopsys) has dramatically changed this situation by providing preprogrammed settings that greatly facilitate its use in an in-office setting.
Prior to cataract surgery, opacified media can make it difficult to evaluate the retina and determine whether cataract surgery will improve vision. Even an optical coherence tomography scan may not provide reliable information in patients with a dense cataract. Ultrasonography can be used to evaluate retinal anatomy, but it is unable to provide functional information that is useful for the assessment of potential vision. Interpretation can also be difficult.
In these cases, the use of full-field electroretinography (ffERG) provides objective information that allows us to evaluate the functional capacity of the retina. Poor ffERG indicates a poor prognosis for improved vision after surgery. Although flicker ffERG cannot highlight the exact location of underlying pathology, it can return valuable information on the health of the cone cells and, therefore, the potential for improved vision after cataract surgery.
STUDY PROTOCOL
We are currently conducting a study using flicker ffERG in the preoperative evaluation of cataract patients. Specifically, we are looking at the relationship between preoperative ERG testing and postoperative visual acuity.
Preliminary results indicate that, in eyes with normal maculae, the flicker ffERG results are the same before and after cataract surgery, demonstrating that cone activity is essentially unchanged regardless of the media opacity. We are using the flicker ffERG module on the Diopsys NOVA device to assess the activity of retinal cones in patients with a dense cataract, either with or without concomitant macular degeneration.
We are now attempting to analyze pre- and postoperative ffERG results (Figure) in patients with macular degeneration to determine if their ERG abnormalities remain unchanged after IOL surgery.
CLINICAL APPLICATIONS OF ERG TESTING
Flicker ffERG
Thus far, it appears that the better the flicker ffERG response is, the better the chance is that functional vision will improve after cataract extraction. Flicker ffERG gives relevant information about the cones’ response in the presence of dense cataracts that is useful for determining the visual prognosis and managing patients’ expectations.
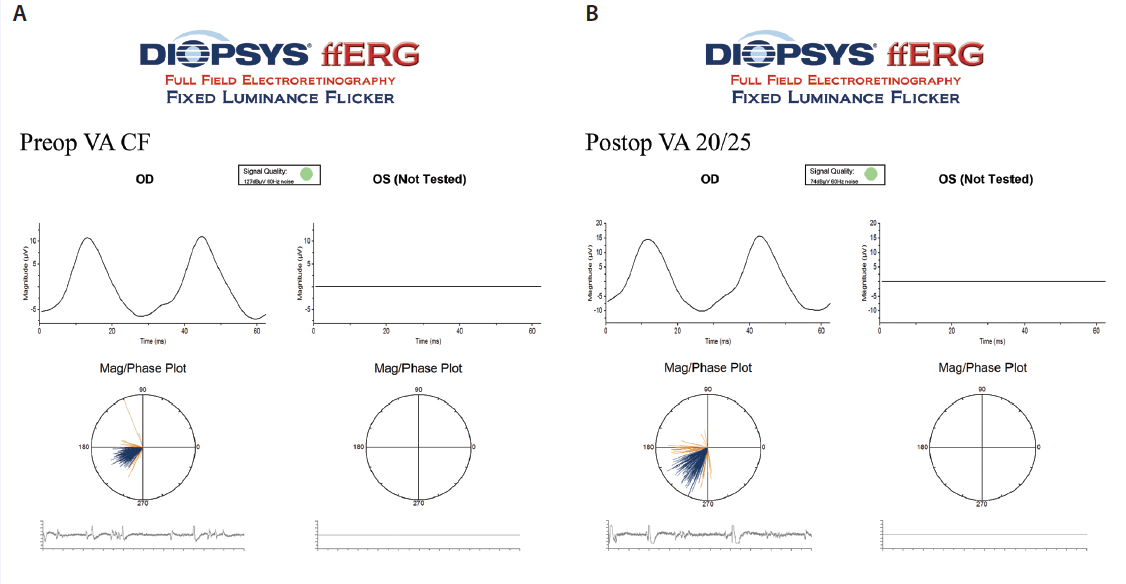
Figure. Preoperative visual acuity ffERG (A) and postoperative visual acuity ffERG (B).
These results provide a rationale for expanding the use of flicker ffERG to any patient with a disorder affecting the cones’ integrity (eg, eyes with diabetic retinopathy). Flicker ffERG may give significant information prior to cataract surgery and help surgeons avoid postoperative surprises.
Pattern ERG
Although not a focus of our current study, the Diopsys platform also has pattern ERG capability. This function provides information about the relative health of the retinal ganglion cell complex. Because patients must be properly refracted for 24 inches for this test, which can be affected by media opacity, pattern ERG is not useful in the setting of a dense cataract. For observing patients with glaucoma or glaucoma suspects, however, pattern ERG can have enormous value as a means of feedback on the efficacy of treatment.
The fundamental goal of managing patients with glaucoma or at risk of developing the disease is to maintain an optimal IOP, but how is that target determined? Currently, the only way to know if pressure is adequately controlled is to monitor the visual fields, evaluate the optic nerve on clinical examination, and assess the nerve fiber layer on optical coherence tomography. Yet, all three of these methods provide information only after significant cellular death has occurred. On the other hand, by providing a quantitative assessment of retinal ganglion cell stress, pattern ERG alerts the physician that therapy should be adjusted and IOP lowered before additional nerve fiber loss or visual field loss occurs.
By monitoring ganglion cell function, in-office ERG can guide therapeutic intervention and thereby preserve retinal nerve fibers.
CONCLUSION
In-office ERG is a user-friendly, objective method to evaluate retinal function. This information can be useful prior to cataract surgery and also to determine the adequacy of pressure-lowering medications in glaucomatous eyes.
Richard Mackool Jr, MD
• assistant director, The Mackool Eye Institute and Laser Center,
Astoria, New York
• (718) 728-3400
• richardmackool@aol.com
• financial interest: none acknowledged
Richard J. Mackool, MD
• director, The Mackool Eye Institute and Laser Center, Astoria,
New York
• (718) 728-3400; mackooleye@aol.com
• financial disclosure: speaker for Diopsys


