OVDs offer the unique dual characteristics of the viscosity commonly observed in fluids and the elasticity typically found in gels or solids (see Characteristics of an Ideal OVD). OVDs are integral to a wide range of ophthalmic surgeries because they can be used to create space, protect intraocular tissue, and facilitate surgical maneuvers.1
OVDs are indispensable to cataract surgery; they can aid with capsulotomy creation and nuclear manipulation.2 They also have applications in cornea, glaucoma, retinal, pediatric, and strabismus surgeries and globe repair. Although invaluable, OVDs are not without potential complications, such as secondary glaucoma, capsular block syndrome, capsular bag distension, anterior pseudo-uveitis, IOL crystallization, and calcific band keratopathy.3
This article provides insights into the effective selection and usage of OVDs, along with an overview of emerging products in this field.
CLASSIFICATION OF OVDs
OVDs may be divided into several categories according to the products’ rheological properties and origins. See the Table for a comparative analysis of OVDs based on Arshinoff’s classification.4
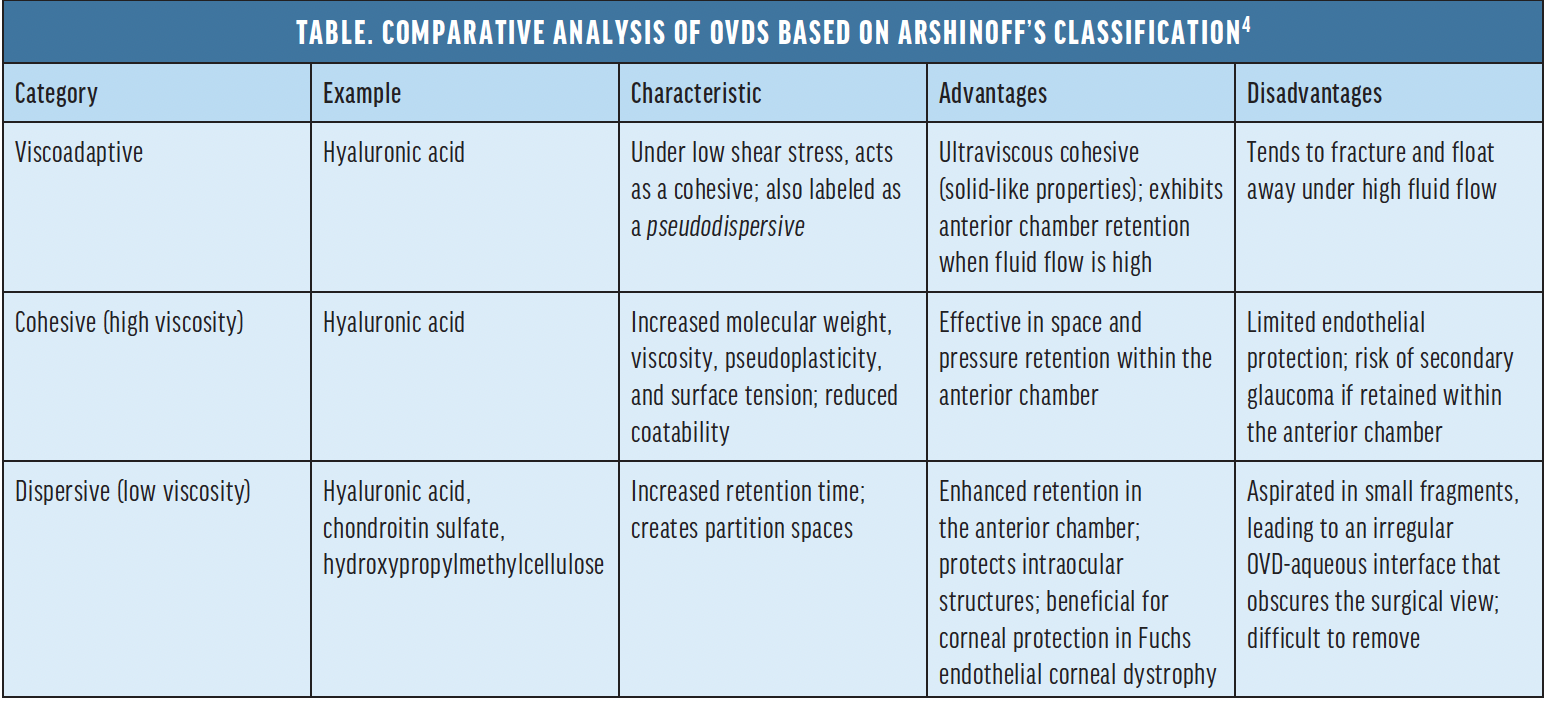
Cohesive OVDs. Composed of high–molecular-weight hyaluronic acid, cohesive OVDs are viscous, maintain their form, and are easily removed postoperatively. They are particularly useful for capsulorhexis.5
Dispersive OVDs. These products have a low molecular weight. They spread readily within the eye to form a protective barrier between surgical instruments and the corneal endothelium.6
Viscoadaptive OVDs. A hybrid between cohesive and dispersive products, viscoadaptive OVDs may be used for multiple surgical steps.
Combination OVDs. Some procedures require the concurrent use of cohesive and dispersive OVDs to leverage the advantages of both.7 Combination OVDs meet this need.
CHARACTERISTICS OF OVDs
Viscosity. The term refers to a solution’s resistance to flow. Factors such as molecular size, concentration, applied force rate, and ambient temperature influence viscosity. Optimal viscosity facilitates precise instrument manipulation during surgical procedures.
Pseudoplasticity. This unique characteristic of OVDs allows them to transition from a viscous to a less viscous state under stress. Sodium hyaluronate exhibits pseudoplasticity more prominently than hydroxypropyl methylcellulose or chondroitin sulfate.
Viscoelasticity. This term describes a material’s ability to regain its original form after deformation. Viscoelasticity is crucial for mitigating the impact of surgeries such as phacoemulsification.
Rigidity. Also referred to as complex viscosity, rigidity relates to the resistance encountered when moving an object through a viscoelastic medium.
Surface adhesion. This characteristic defines how well an OVD coats a surface. Lower resistance and smaller contact angles indicate superior coating ability.
Viscoadaptability. This property allows a transition from a highly viscous state at slow movement rates to a more fluid state at faster rates. Products such as Healon5 (Johnson & Johnson Vision) have demonstrated high viscoadaptability.
Cohesion. This term refers to the bonding tendency among viscoelastic molecules, which is influenced by factors such as molecular size and pseudoplasticity.
Dispersiveness. This term describes the limited bonding tendency among molecules in certain OVDs.
Coating ability. Higher–molecular-weight OVD, especially those carrying negative charges such as sodium hyaluronate and chondroitin sulfate, tend to coat surfaces better.2
CHARACTERISTICS OF AN IDEAL OVD1
An ideal OVD is the following:
- Optically clear and transparent;
- Biocompatible and noninflammatory;
- Sterile, without inducing anterior chamber reactions;
- Economically viable; and
- Easy to remove postoperatively.
Rheological considerations
Stabilizing effect.At low shear rates, high viscosity aids in space preservation and tissue protection.
Mobilizing effect.Moderate viscosity at medium shear rates facilitates instrument manipulation.
Injectability.At high shear rates, reduced viscosity allows smooth injection of the OVD through a cannula with a fine diameter.2
1. Liesegang TJ. Viscoelastic substances in ophthalmology. Surv Ophthalmol. 1990;34(4):268-293.
2. Kaur K, Gurnani B. Viscoelastics. In: StatPearls [Internet]. StatPearls Publishing; 2023.
PATIENT-SPECIFIC CONSIDERATIONS FOR OVD SELECTION
Choosing the most appropriate OVD is crucial to successful surgical outcomes. The decision depends on factors such as the nature of the procedure, the patient’s ocular health, the surgeon’s experience, and product cost and availability.
Cataract surgery. OVDs are essential during phacoemulsification and extracapsular cataract extraction, and they can facilitate the capsulorhexis, hydrodissection, and nucleus manipulation.1
Glaucoma surgery. In procedures such as trabeculectomy, OVDs are instilled to protect the endothelium and maintain chamber depth.1
Corneal surgery. OVDs support trephination, protect intraocular structures, and help prevent damage during procedures such as keratoplasty.2
Viscoanesthesia. A synergistic combination of an OVD and lidocaine can serve as an intracameral anesthetic, extending the duration of the drug’s anesthetic effect.2
Viscomydriasis. Certain OVDs are effective in facilitating pupillary dilation during surgical procedures.
Intraoperative floppy iris syndrome. For patients receiving therapy with alpha-adrenergic blockers, the use of viscoadaptive OVDs during ocular surgery can assist with managing and stabilizing the pupil, thereby mitigating potential complications.
Retinal surgery. OVDs can facilitate safe membrane adhesion separation. Sodium hyaluronate is the preferred choice.1
Orbit and oculoplastic surgery. OVDs are useful in surgeries for congenital nasolacrimal duct obstruction and ptosis.2
Pediatric ophthalmology and strabismus surgeries. OVDs are used during the standard steps of pediatric cataract procedures. In strabismus surgery, OVDs can ease suture adjustments and reduce scarring.1
A BALANCED APPROACH TO OVD SELECTION
Every medical intervention demands a careful balance of potential benefits against associated risks. With OVDs, several considerations come into play.
Surgical objectives. The primary aim of the surgical procedure should inform the choice of OVD. For instance, if the principal goal is to protect the endothelium, a dispersive OVD may be most beneficial. In contrast, a cohesive OVD may be more suitable for a procedure requiring space maintenance.
Potential complications. Cohesive OVDs may elevate the risk of postoperative IOP spikes due to incomplete removal. Caution should therefore be exercised when using these products in glaucomatous and glaucoma suspect eyes.
The current literature. It is important for surgeons to remain abreast of the latest studies concerning the safety and efficacy of OVDs.8
NEW-GENERATION OVDS*
COHESIVE
StableVisc (Bausch + Lomb). Designed to maintain space in the anterior chamber, this OVD contains sodium hyaluronate and sorbitol for increased free radical scavenging capabilities.
DISPERSIVE
ClearVisc (Bausch + Lomb).This OVD is supplied in a 1.0-mL syringe and offers free radical protection with sorbitol.
Z-Celcoat (Carl Zeiss Meditec). This low-viscosity dispersive OVD is designed to provide protection during various surgical maneuvers.
DUAL-ACTION
TotalVisc (Bausch + Lomb).A dual-pack system features both a cohesive and a dispersive OVD for dual-action protection during surgery.
MULTIFUNCTIONAL
Visthesia Intra/Visthesia (Carl Zeiss Meditec).This OVD aids in creating and maintaining space in the anterior chamber and facilitates the even dispersion of lidocaine throughout the eye to all tissues.
INNOVATIVE DELIVERY SYSTEMS
CombiVisc (Carl Zeiss Meditec).This product offers a combination of a viscous-cohesive and a medium-viscosity dispersive OVD in two separate syringes.
TwinVisc (Carl Zeiss Meditec).This product combines a medium-viscosity dispersive OVD and a viscous-cohesive OVD in a single syringe, separated by a bypass stopper system.
*This is a curated selection and may not cover the full spectrum of new-generation OVDs.
POSTOPERATIVE CARE
It is crucial to monitor patients who have undergone surgery with an OVD. Two key metrics warrant attention.
IOP. Elevated IOP is a potential postoperative complication that can lead to glaucoma and subsequent vision loss. Timely monitoring facilitates prompt intervention to ensure that the IOP remains within or returns to a safe range.
Endothelial cell density. A healthy corneal endothelium is critical for maintaining corneal transparency. Given that endothelial cells do not regenerate, their preservation is crucial. Postoperative monitoring of endothelial cell density helps ensure that neither the surgical procedure nor the OVD induces significant endothelial cell loss.
FUTURE OUTLOOK
The landscape of OVDs is evolving (see New-Generation OVDs). Current research focuses on several areas.
Enhanced biocompatibility. Future iterations of OVDs may be designed for greater biocompatibility, thereby minimizing inflammatory responses and other potential complications.
An extended duration of action. Prolonging the effective duration of OVDs could offer advantages in complex surgical scenarios.
Multifunctionality. Beyond their traditional roles in space creation and tissue protection, future OVDs may incorporate additional features, such as drug-delivery mechanisms.
Tailored solutions. It may become possible to customize OVDs to individual patient profiles (eg, unique ocular conditions and surgical requirements).
1. Higashide T, Sugiyama K. Use of viscoelastic substance in ophthalmic surgery – focus on sodium hyaluronate. Clin Ophthalmol. 2008;2(1):21-30.
2. Kaur K, Gurnani B. Viscoelastics. In: StatPearls [Internet]. StatPearls Publishing; 2023.
3. Borkenstein AF, Borkenstein EM, Malyugin B. Ophthalmic viscosurgical devices (OVDs) in challenging cases: a review. Ophthalmol Ther. 2021;10(4):831-843.
4. Arshinoff SA, Jafari M. New classification of ophthalmic viscosurgical devices—2005. J Cataract Refract Surg. 2005;31:2167-2171.
5. Watanabe I, Hoshi H, Sato M, Suzuki K. Rheological and adhesive properties to identify cohesive and dispersive ophthalmic viscosurgical devices. Chem Pharm Bull (Tokyo). 2019;67(3):277-283.
6. Yildirim TM, Auffarth GU, Son HS, Khoramnia R, Munro DJ, Merz PR. Dispersive viscosurgical devices demonstrate greater efficacy in protecting corneal endothelium in vitro. BMJ Open Ophthalmol. 2019;4(1):e000227.
7. Tognetto D, Cecchini P, Ravalico G. Survey of ophthalmic viscosurgical devices. Curr Opin Ophthalmol. 2004;15(1):29-32.
8. Packer M, Berdahl JP, Goldberg DF, Hosten L, Lau G. Safety and effectiveness of a new ophthalmic viscosurgical device: randomized, controlled study. J Cataract Refract Surg. 2022;48(9):1050-1056.