Sponsored By


Over my years in practice, the way in which I align toric IOLs has changed significantly. In the beginning, when I first started implanting toric IOLs, I used a completely manual technique. But as technologies became available to aid in planning and aligning toric IOLs, I quickly realized the advantages that such a sophisticated technology could have on my patients’ outcomes.
In this article, I share not only my own personal evolution in toric IOL alignment technique but also the impact that incorporating lens alignment technology has had on my surgical results.
EVOLUTION OF ALIGNMENT TECHNIQUES
When I first started using toric IOLs to correct astigmatism, the only technique that was available to align these lenses was a manual one. At this early time in my experience, patients would sit in an upright position, and, as accurately as I could, with their heads moving and tilting and their eyes blinking, I tried to mark the 180º axis with a corneal marker. As one could imagine, during surgery the lens was not always aligned properly, requiring me to go back into the eye at a later time to reposition the lens. Another side effect of this technique was that my patients often had residual corneal astigmatism.
I then incorporated a slit lamp into the equation, using the actual slit beam itself to mark the cornea for the target axis (Figure 1). Although my results improved, I still had a significant number of cases of misalignment and patients who experienced residual corneal astigmatism.
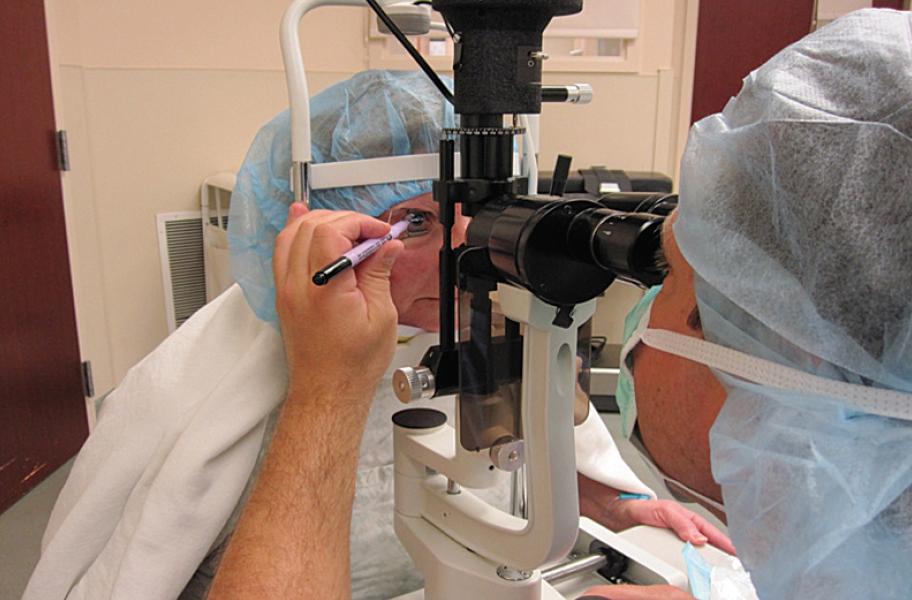
Figure 1. The author marking the 180º axis with a corneal marker while the patient is seated in an upright position at the slit lamp. In this earlier technique, the slit beam was used as a guide to mark the axis.
When CALLISTO eye (Carl Zeiss Meditec) became available in 2013, I was an early adopter. I still had to utilize the slit lamp and manually mark the 180º axis as a reference, because the markerless software for CALLISTO was not yet available in the United States. I then could rely on the CALLISTO software to produce a reference image and a target axis that was specific to the patient’s own ocular anatomy.
The last step in my evolution in toric IOL alignment would be to go markerless. That is where the ZEISS Cataract Suite has come in. This integrated platform includes the CALLISTO eye, the IOLMaster 500 or 700, FORUM, and the OPMI LUMERA family of microscopes (Figure 2). The beauty of CALLISTO eye is that it integrates the information from the IOLMaster into the OPMI LUMERA microscope. Said another way, it takes the image generated by the IOLMaster, compares it with the intraoperative image that is obtained at the time of surgery, and, using limbal vessels as guides, pairs those two images very closely so that they can be precisely matched. This compilation image is then injected into the ocular of the LUMERA 700 microscope, creating a visual aid for toric IOL alignment.

Figure 2. Components of the ZEISS Cataract Suite, as positioned in the author’s operating room.
CALLISTO eye uses an integrated data injection system (IDIS) to overlay the visual aid in the oculars of the operating microscope. This computer-assisted surgery technique has helped me with incision placement and size, including main, sidecut, and limbal relaxing incisions; capsulorrhexis size and placement; and, of course, IOL axis adjustment. Figure 3 depicts what I see when I am using the CALLISTO eye in the OR for capsulorrhexis: On the left is the capsulorrhexis circle and, on the right, the target axis line.
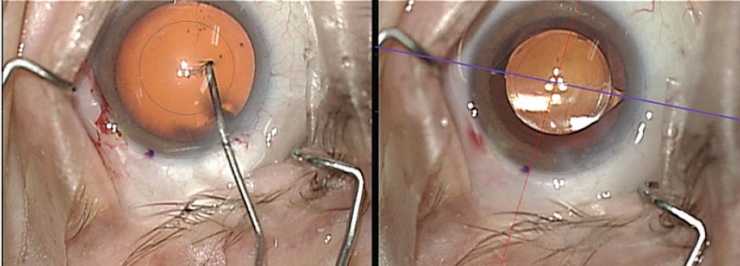
Figure 3. The integrated data injection system of the CALLISTO eye allows the overlay of visual aids in the oculars of the operating microscope.
POSITIVE AFFECTS ON POSTOPERATIVE OUTCOMES
In an analysis of my postoperative outcomes with toric IOLs, my colleagues and I have assessed results with manual alignment and with aid of the CALLISTO eye prior to and after incorporation of markerless technology. Below is a summary of these results.
Manual alignment without a slit lamp. Prior to 2010, all toric IOLs were implanted using a manual alignment technique. A former resident of mine conducted a retrospective study of 44 eyes that were marked while the patient was in an upright position. In each case, the horizontal axis was marked as accurately as possible with the patient sitting up. Afterward, the patient was laid down and their cornea was marked with a corneal marker.
Of the 44 eyes, 66% ended up within 5º of the target axis and 34% more than 5º of target axis. Additionally, 27.3% had 0.75 D or more of residual corneal astigmatism. These were fairly humbling results.
Manual alignment with a slit lamp. After I incorporated a slit lamp into my process for toric IOL alignment, I felt that I had better control of patients’ heads and I was using the actual slit beam itself to show where to mark the cornea for the target axis.
In another retrospective analysis of my results in 57 eyes treated prior to 2014 in which all patients were marked while seated at the slit lamp, 49% were within 3º of the target axis. However, 33% were still somewhere between 4º and 5º from the target axis and 17.5% were more than 5º off. Further, 38% experienced 0.75 D or more of residual corneal astigmatism.
Slit lamp plus CALLISTO eye. I analyzed my results using the slit lamp beam to mark the 180º axis and CALLISTO eye to determine the target axis. In this series of 65 eyes that were treated between September 1, 2013, and November 15, 2014, 63 had 2-week postoperative refractions and 57 had dilated postoperative examinations to confirm the axis placement at the slit lamp. Of those 57, 94.7% were within 3º of target axis. Of the three remaining eyes, 2 were within 4º and 1 within 6º of the target axis. This indicated a significant improvement in my results with the addition of CALLISTO.
Markerless alignment. In order to implement markerless toric IOL alignment, the addition of at least the IOLMaster 500 is required to obtain a reference image (Figure 4) to guide toric lens alignment. In this series, I looked at results in 74 eyes that had the axis confirmed between 2 and 3 weeks postoperatively with dilated exams at the slit lamp. What I found was that 87% of eyes were within 3º of the target axis, that 11% were within 4º of target axis, and that only one eye was 5º from the target axis.
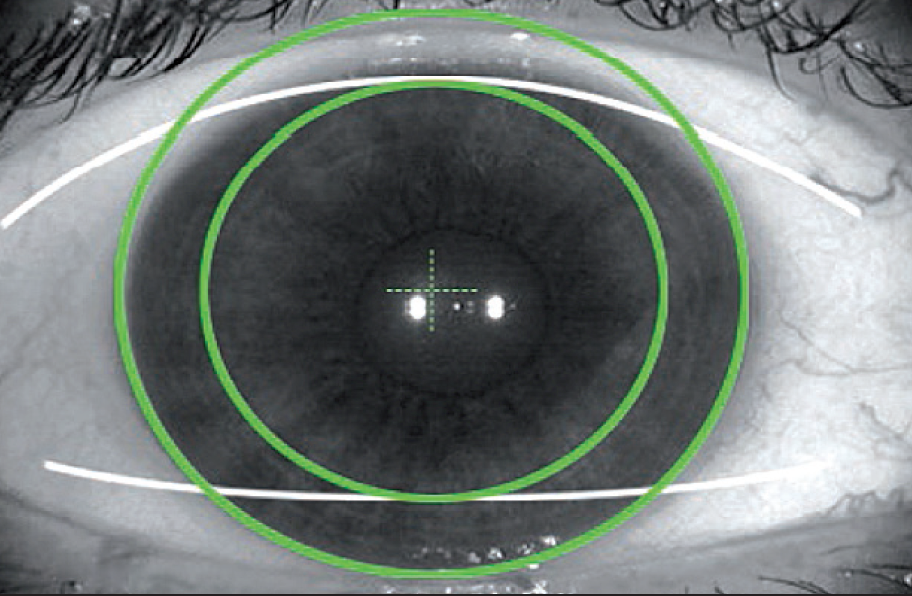
Figure 4. A sample reference image from the IOLMaster, used to guide toric IOL alignment.
CONCLUSION
In my experience, I have found that the CALLISTO eye has allowed me to reach the results with toric IOLs that I had been striving to achieve for many years. As my technique has improved, my results have improved, and with it so have my patients’ demands for premium and toric IOLs. This is evident in the number of eyes in which I have implanted with a toric IOL prior to and after incorporation of markerless technology: 44 eyes with manual alignment without a slit lamp, 57 eyes with manual alignment with a slit lamp, and 65 eyes with a slit lamp plus CALLISTO eye.
All in all, CALLISTO eye has been a useful tool in my practice, not only in toric IOL implantation but in routine cataract surgery.
The statements of the healthcare professionals giving this presentation reflect only their personal opinions and experiences and do not necessarily reflect the opinions of any institution with whom they are affiliated.
The healthcare professionals giving the presentation may have a contractual relationship with Carl Zeiss Meditec, Inc., and may have received financial compensation.
