The idea that patients have higher expectations for their outcome than at any time in the history of refractive surgery is nothing new. More and more, ensuring patients are having a good experience, in addition to providing excellent post-procedure vision, is less so a value-add to the services we provide, and more so a mandate. Indeed, a satisfied patient is a practice builder.1
There is now emerging evidence that patients associate their level of satisfaction with both the quality and efficiency of surgical care,2 and that confidence and trust in the clinical team is an important determinant of patient experience.3 Thus, the delivery of patient-focused care requires that we provide care in a particular way, not just sometimes or usually, but always.1
What Matters to Patients During Surgery
Especially in the age of social media, it is imperative that refractive surgeons think about every aspect of the patient experience. That includes having helpful, friendly, and knowledgeable staff to help guide the patient from the pre-procedure work-up all the way through the follow-up period and after. With the advent of social media sharing, one misstep in the office could literally be shared with thousands or millions of individuals. In addition to having confidence and trust in the staff, patients also want to feel confident in the technology that will be used during their procedure.
There are also a few aspects of the procedure that can help improve a patient’s experience. Below is my list of features patients want from their refractive vision correction, and how the SMILE procedure can help deliver a good experience.
No. 1: No Loss of Vision
The “black-out period” during a LASIK procedure describes the transient loss of vision occurring secondary to high IOP, which functions to block blood flow to the optic nerve. This can be disconcerting to patients and may cause them to move or jump when it happens, in turn leading to suction loss. Aside from the safety implications, patient movements might affect the alignment, thereby leading to unexpected outcomes. Because docking is performed on the cornea during a SMILE procedure, instead of the conjunctiva, less pressure is needed to maintain docking. As a result, SMILE provides for better control of IOP throughout the procedure (Figure 1).4 This may seem a rather trivial point, but maintaining proper alignment is fundamental for safely removing the lenticule.
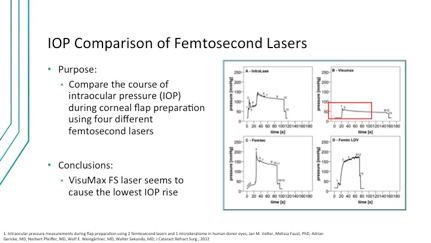
Figure 1. The VisuMax femtosecond laser induces the lowest rise in IOP during flap preparation.
No.2: No Hard Suction
While the suction used during SMILE is strong enough to maintain fixation, it is nevertheless gentle. The procedure uses a spherical contact interface to the cornea with minimal applanation that is only applied during the actual laser portion; as well, the VisuMax Laser (Carl Zeiss Meditec, Inc.) automatically finds visual axis centration, helping to ensure the correct alignment.
No. 3: No Pain
It is easy to understand that patients do not want a painful procedure. There is evidence that use of a curved versus a planar interface results in reduced pain (Figure 2).5 However, as we think about the population of patients now seeking refractive procedures, absence of pain may not be enough—today’s patients do not even want to experience discomfort during a procedure. Understanding the mindset of the modern refractive surgery patients means abandoning the old thinking of “no pain, no gain,” and replacing it with “no pain … no pain.” That is to say that patients who experience even the slightest discomfort may tell their friends and unduly ruin a hard-earned reputation.
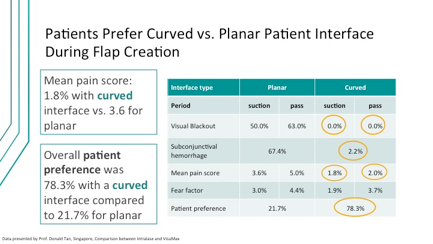
Figure 2. Several metrics suggest advantages with a curved versus a planar interface during flap creation.
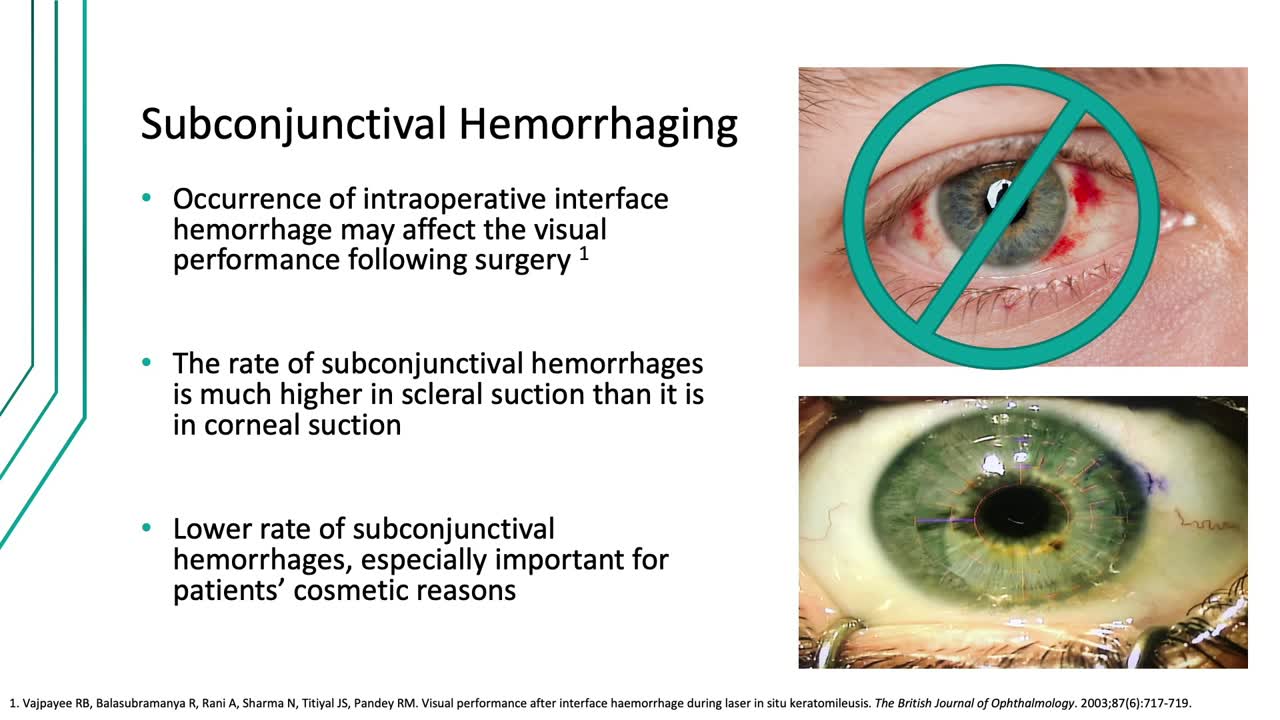
No. 4: No Subconjunctival Hemorrhaging
Speaking of mantras we should abandon, one of the axioms I heard when I started in ophthalmology was the redder the better, referring to the idea that blood inside the eye would help the healing process. On the one hand, the occurrence of intraoperative interface hemorrhage may affect the visual performance following surgery.6 More fundamentally, though, that kind of message just does not translate with today’s patients. It is our experience that the conjunctiva looks pristine following a SMILE procedure (Figure 3), which is a welcome difference compared with the transient red, bloodshot appearance that is not uncommon following LASIK. Fair or not, the patients’ perception of the cosmetic appearance will be used to judge the quality of the outcome.
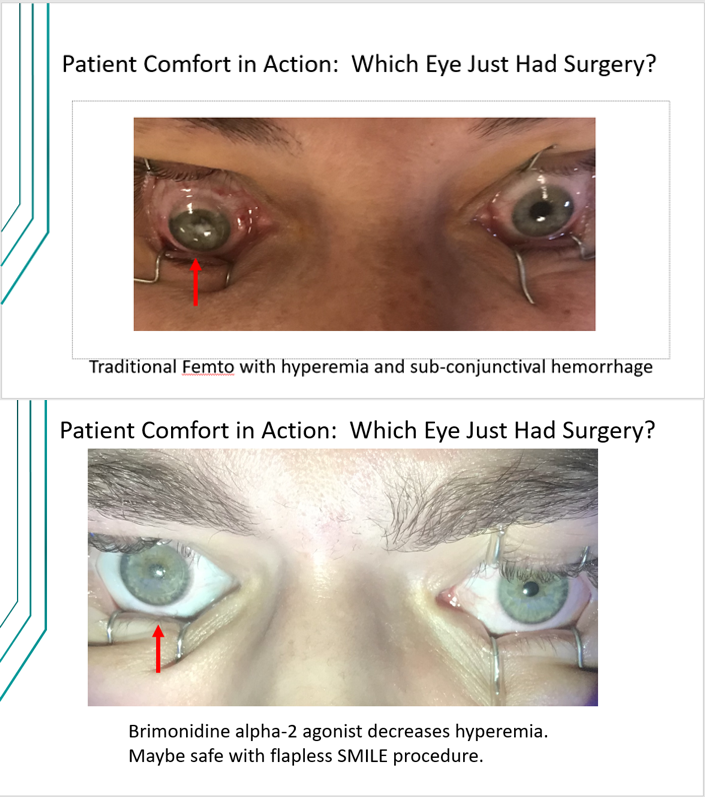
Figure 3.
No. 5: No Fear
Undergoing any procedure, including refractive correction, may induce anxiety. And so, whenever possible, we should help to assuage any fears the patient might have by explaining the various steps and maintaining good dialogue during the procedure. Learning to deliver comfort through communication is something that I have truly come to appreciate in working with patients over time.
Conclusion
There is no secret formula for assuring patients’ satisfaction, but there are steps all surgeons can take to improve the experience their patients have during a refractive procedure. In my view, it all starts with effective communication and getting the entire staff on the same page. Today’s patients are more demanding than ever before, and yet, the procedures at our disposal are more sophisticated and advanced than ever before. In many ways, the emergence of the SMILE procedure is rather serendipitous, as it appears to offer some distinct advantages over traditional forms of vision correction.
Click to Watch Dr. Wiley's Presentation
1. Prakash B. Patient satisfaction. J Cutan Aesthet Surg. 2010;3(3):151-155.
2. Tsai TC, Orav EJ, Jha AK. Patient satisfaction and quality of surgical care in US hospitals. Ann Surg. 2015;261(1):2-8.
3. Jones CH, O’Neill S, McLean KA, et al. Patient experience and overall satisfaction after emergency abdominal surgery. BMC Surg. 2017;17:76.
4. Vetter JM1, Faust M, Gericke A, et al. Intraocular pressure measurements during flap preparation using 2 femtosecond lasers and 1 microkeratome in human donor eyes. J Cataract Refract Surg. 2012; 38(11):2011-18.
5. [Data presented by Prof. Donald Tan, Singapore, Comparison between Intralase and VisuMax]
6. Vajpayee RB, Balasubramanya R, Rani A, et al. Visual performance after interface haemorrhage during laser in situ keratomileusis. Br J Ophthalmol. 2003;87(6):717-719.