Canaloplasty describes a procedure in which a microcatheter is threaded through the Schlemm canal, followed by introduction of viscoelastic to dilate the canal and to flush the trabecular meshwork and collector channels. Fundamentally, what these maneuvers describe is an effort to restore physiologic outflow, in a sense winding the clock back and helping to rejuvenate the eye’s natural mechanism for promoting outflow of aqueous humor.
It is well known that, while most of the resistance in primary open-angle glaucoma occurs at the trabecular meshwork, other parts of the outflow system, including the Schlemm canal and collector channels, are often compromised. As a result, it makes sense to address the anatomy that drives glaucomatous pathology as comprehensively as possible. Because canaloplasty involves microcatheterization and viscodilation of 360° of the canal, it offers the opportunity to do that, albeit in a minimally invasive fashion that can be performed at the time of cataract surgery or as a standalone procedure.
Yet not all canaloplasty procedures are necessarily equal. The iTrack Advance (Nova Eye Medical) has several features that differentiate it from other systems (Figure 1). For one, it is the only device that can be passed through the canal for 360° in a single pass, minimizing instrument passes compared to navigating 180° at a time. As well, it has an illuminated tip, which gives instant feedback to the surgeon that the microcatheter is in the Schlemm canal.
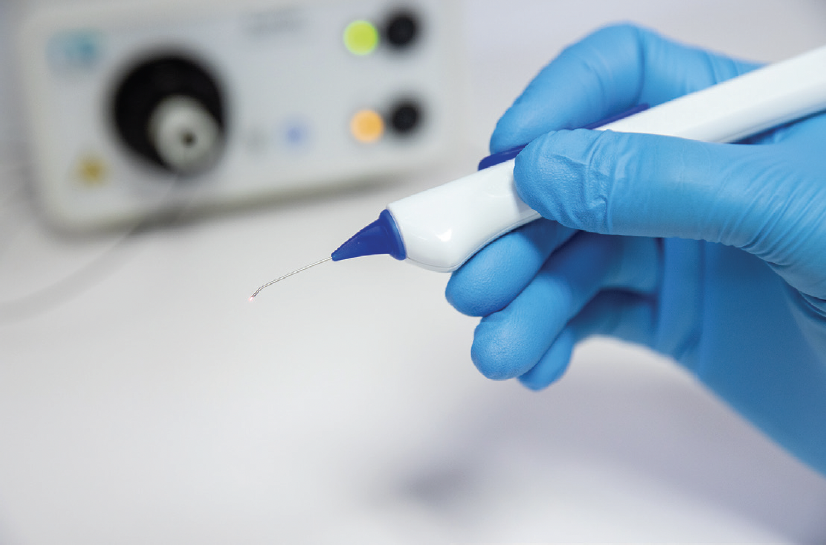
Figure 1. The iTrack Advance, shown here with the illuminated tip.
The iTrack Advance is associated with equivalent safety and efficacy as the original iTrack device, but it has been designed to facilitate easier adoption and use. For instance, the spatulated tip design allows easy access into the Schlemm canal, thereby eliminating the need to perform needle-based goniotomy for insertion of the microcatheter. It also has a rotatable nozzle, making it convenient for use by right- and left-handed surgeons alike. The actuator mechanism has also been improved for greater precision and accuracy for precise advancement and retraction of the microcatheter. In my hands, I have found the iTrack Advance device simple to use and straightforward to integrate into my surgical protocol.

A Brief History of Canaloplasty
The earliest iteration of canaloplasty evolved from concepts that originated in viscocanalostomy and deep sclerotomy. As its name implies, viscocanalostomy involves injection of viscoelastic into Schlemm canal, in turn leading to disruptions of the inner wall. The technique, first described by Stegmann et al in 1999,1 involved a scleral dissection, followed by injection of viscoelastic via a metal cannula (see The Evolution of Canaloplasty). However, as the cannula was not flexible, only a limited portion of the canal on either side of the dissection site could be dilated. Furthermore, absent measures to dilate the canal for a full 360°, eyes undergoing viscocanalostomy were at risk for eventual re-collapse, which likely explains why longer-term efficacy was less than ideal.2
Early canaloplasty procedures sought to improve upon viscocanalostomy with the addition of a flexible microcatheter that was advanced though the canal using an ab externo approach. Following creation of a scleral flap, Schlemm canal was located and unroofed, followed by creation of a paracentesis for insertion of the microcatheter, which was then advanced for 360°. When the distal end re-emerged, a suture was attached; as the microcatheter was withdrawn through the canal, viscoelastic was injected every two clock hours using a screw-driven injector. Finally, the suture was detached from the microcatheter and tightened to provide durable patency before the rest of the surgical field was closed.
The Evolution of Canaloplasty
1999
Viscocanalostomy technique first described by Prof. Robert Stegmann (South Africa).1
2004
The world’s first canaloplasty procedure is performed by Prof. Robert Stegmann via an ab externo surgical technique, using the iTrack™ microcatheter.
2005
Lewis et al commence a prospective, three-year, multicenter study to investigate the effectiveness of canaloplasty in POAG patients.2
2011
Multicenter study by Lewis et al demonstrates the efficacy and safety profile of canaloplasty in patients with primary open-angle glaucoma at 36 months.2
2016
The world’s first canaloplasty procedures via an ab interno surgical technique are performed by Mahmoud A. Khaimi (USA) and Mark J. Gallardo (USA) using the iTrack™ canaloplasty microcatheter.
2023
FDA clearance of iTrack™ Advance, which combines the original iTrack™ canaloplasty microcatheter with a handheld injector.
1. Stegmann R, Pienaar A, Miller D. Viscocanalostomy for open-angle glaucoma in black African patients. J Cat Refract Surg. 1999;25:316-322.
2. Lewis RA, von Wolff K, Tetz M, et al. Canaloplasty: three-year results of circumferential viscodilation and tensioning of Schlemm canal using a microcatheter to treat open-angle glaucoma. J Cat Refract Surg. 2011;37(4):682-690.
Ab externo canaloplasty was an intriguing yet cumbersome approach to treating glaucoma. The surgery took about an hour, and it was predominantly indicated for very sick eyes. As well, the bail out, if anything went wrong during the procedure, was to convert to a trabeculectomy. As an anterior segment surgeon, it was just not a procedure that fit well with my practice, nor was it suitable for my patient population.
The ab interno variation of canaloplasty that we know today certainly owes its heritage to the ab externo technique, but it is much less invasive, making it appropriate for use in earlier glaucoma. With the introduction of the iTrack Advance, it is also a much simpler technique to learn and master. Like its predicate device, the fundamental principles are the same: introduction of a microcatheter and advancement in the forward direction for 360° in a single pass, thereby breaking herniations, followed by retraction while introducing viscoelastic, thus dilating the canal while also flushing the collector channels.
Designed to Restore Physiologic Function
The reason canaloplasty with the iTrack Advance is so intriguing is because it offers a trimodal mechanism of action, thereby treating all points of outflow resistance.3 Up to 75% of the resistance in primary open-angle glaucoma occurs at the trabecular meshwork, particularly in the juxtacanalicular area immediately adjacent to the Schlemm canal.4 Perhaps less well appreciated is that up to 90% of collector channels are blocked with herniated trabecular meshwork tissue in glaucomatous eyes.5 As well, the inner lumen of the Schlemm canal is often smaller in eyes with primary open-angle glaucoma, accounting for up to 50% of decreased outflow capacity.6,7 Intuitively, then, it makes sense to perform procedures that deal with the anatomy in the proximal and distal outflow pathways. This is precisely what the iTrack Advance procedure is intended to do.
The first mechanism associated with the iTrack Advance is introduced as the microcatheter mechanically breaks herniations in the canal. Notably, if obstructions occur, viscoelastic can be introduced to help clear the blockages. The iTrack Advance handpiece features a fully rotating nozzle, so if any part of the canal proves impassable, the microcatheter is easily reversed, the nozzle rotated, and the microcatheter then advanced in the opposite direction.
The second mechanism occurs as pressurized viscodilation is introduced while the microcatheter is being retracted. This step complements the mechanical disruption of adhesions in the Schlemm canal and helps dilate the canal.1,8,9 It also has the effect of stretching the trabecular meshwork, creating tiny microperforations to improve outflow facility. Finally, as a third mechanism, pressurized viscodilation flushes the collector channels.
As a stentless procedure that preserves trabecular meshwork anatomy, rather than an attempt to remove it or bypass it, the iTrack Advance procedure allows the surgeon to work with the physiology of the eye rather than around it. On the one hand, because no tissue is stripped during the procedure, it is theoretically repeatable and leaves other treatment options viable should they become necessary in the future. Equally as important, preserving the trabecular meshwork tissue maintains its physiologic role in regulating pressure dynamics.10
There is a growing body of evidence suggesting that a build-up of extracellular matrix proteins and banded fibrillar elements in the trabecular meshwork compromise its filtering capacity.11,12 Under normal conditions, endothelial cells in the trabecular meshwork help regulate levels of hyaluronic acid,13 which function to activate matrix metalloproteinases 2 and 9 to clear deposition of extracellular matrix.14 Low hyaluronic acid levels lead to conversion of the hyaluronic acid receptor to a form that is toxic to endothelial cells.15 Of note, hyaluronic acid levels are lower in eyes with primary open-angle glaucoma compared to healthy eyes.16 And so, any further reduction in the number of endothelial cells of the trabecular meshwork compromises the eye’s ability to regulate hyaluronic acid levels, and by extension, IOP.17-19 Conversely, delivery of synthetic hyaluronic acid via injection of viscoelastic during the iTrack Advance procedure helps restore physiologic levels, and thereby preserve its role in regulating pressure dynamics.
Of additional significance, the iTrack Advance is the only canaloplasty device that allows for up to 360° of catheterization in a single pass. Because there is no way of knowing where in the complex aqueous pathway obstruction is occurring, treating the entire circumference of the canal, and addressing the anatomy in at least three areas, ensures the best chance for restoring physiologic flow.
The iTrack Advance is also a titratable procedure, meaning the surgeon controls how much viscoelastic is delivered as the microcatheter is retracted. Rather than being a constant flow, the mechanism to deliver viscoelastic is controlled by a scrub nurse or technician in the room. In my cases, I like to deliver about two clicks per clock hour, which results in about 100 µL of viscoelastic in total. However, if desired, I can deliver more or less viscoelastic, depending on the anatomy of the individual patient.
Considerations for Patient Selection
One of the advantages of canaloplasty with the iTrack Advance is that there are many ways to define the ideal patient. Although a wide range of patients could benefit from the procedure, it appears to have the greatest benefit in early or mild to moderate glaucoma, before the angle has become fibrosed and sclerotic. We know from experience that the distal outflow system becomes increasingly compromised as the disease advances; if that is the case, then there should be increased benefit for rejuvenating the entire outflow pathway while portions of it are still viable.
1. Stegmann R, Pienaar A, Miller D. Viscocanalostomy for open-angle glaucoma in black African patients. J Cataract Refract Surg. 1999;25:316-322
2. Sunaric-Megevand G, Leuenberger PM. Results of viscocanalostomy for primary open-angle glaucoma. Am J Ophthalmol. 2001;132(2):221-228
3. Khaimi MA, Dvorak JD, Ding K. An Analysis of 3-Year Outcomes Following Canaloplasty for the Treatment of Open-Angle Glaucoma. J Ophthalmol. 2017;2017:2904272.
4. Goel M, Picciani RG, Lee RK, Bhattacharya SK. Aqueous humor dynamics: a review. Open Ophthalmol J. 2010;4:52-59.
5. Cha EDK, Xu J, Gong H. Variations in active areas of aqueous humor out#ow through the trabecular outflow pathway. Invest Ophthalmol Vis Sci. 2015;56(7):4850.
6. Johnstone MA, Grant WG. Pressure-dependent changes in structures of the aqueous outflow system of human and monkey eyes. Am J Ophthalmol. 1973;75:365-383
7. Allingham RR, de Kater AW, Ethier CR. Schlemm’s canal and primary open angle glaucoma: correlation between Schlemm’s canal dimensions and outflow facility. Exp Eye Res. 1996;62(1):101-109.
8. Grieshaber MC, Pienaar A, Olivier J, Stegmann R. Clinical evaluation of the aqueous outflow system in primary open-angle glaucoma for canaloplasty. Invest Ophthalmol Vis Sci. 2010;51(3):1498-1504.
9. Smit BA, Johnstone MA. Effects of viscoelastic injection into Schlemm’s canal in primate and human eyes: potential relevance to viscocanalostomy. Ophthalmology. 2002;109(4):786-792.
10. Grant WM. Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol. 1963;69:783-801.
11. Acott TS, Kelley MJ. Extracellular matrix in the trabecular meshwork. Exp Eye Res. 2008;86:543-561.
12. Acott TS, Kelley MJ, Keller KE, et al. Intraocular pressure homeostasis: maintaining balance in a high-pressure environment. J Ocul Pharmacol Ther. 2014;30:94-101.
13. Entwistle J, Hall CL, Turley EA. HA receptors: regulators of signalling to the cytoskeleton. J Cell Biochem. 1996;61(4):569-577.
14. Umihira J, Nagata S, Nohara M, et al. Localization of elastin in the normal and glaucomatous human trabecular meshwork. Invest Ophthalmol Vis Sci. 1994;35(2):486-494.
15. Green KA, Yue BY, Samples JR, Knepper PA. Glaucoma Research and Clinical Advances: 2016-2018. In: Knepper PA, Samples JR, eds. Trabecular meshwork cell death in primary open-angle glaucoma. Amsterdam, The Netherlands: Kugler Publications. 2016:1-16
16. Knepper PA, Goossens W, Hvizd M, Palmberg PF. Glycosaminoglycans of the human trabecular meshwork in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 1996;37(7):1360-1367.
17. Alvarado J, Murphy C, Juster R. Trabecular meshwork cellularity in primary open-angle glaucoma and nonglaucomatous normals. Ophthalmology. 1984;91:564-579.
18. Alvarado J, Murphy C, Polansky J, Juster R. Age-related changes in trabecular meshwork cellularity. Invest Ophthalmol Vis Sci. 1981;21:714-727.
19. Grierson I, Howes RC. Age-related depletion of the cell population in the human trabecular meshwork. Eye (Lond). 1987;1:204-210.
The iTrack™ Advance has a CE Mark (Conformité Européenne) and US Food and Drug Administration (FDA) 510(k) #K221872 for the treatment of open-angle glaucoma.
INDICATIONS: The iTrack™ Advance is indicated for fluid infusion or aspiration during surgery. The iTrack™ Advance is indicated for catheterization and viscodilation of Schlemm’s canal to reduce intraocular pressure in adult patients with open angle glaucoma.
CONTRAINDICATIONS: The iTrack™ Advance is not intended to be used for catheterization and viscodilation of Schlemm’s canal to reduce intraocular pressure in eyes of patients with the following conditions: Neovascular glaucoma; Angle-closure glaucoma; Previous surgery with resultant scarring of Schlemm’s canal.
ADVERSE EVENTS: Possible adverse events with the use of the iTrack™ Advance include, but are not limited to: hyphema, elevated IOP, Descemet’s membrane detachment, shallow or at anterior chamber, hypotony, trabecular meshwork rupture, choroidal effusion, Peripheral Anterior Synechiae (PAS) and iris prolapse.
PRECAUTIONS: The iTrack™ Advance should be used only by physicians trained in ophthalmic surgery. Knowledge of surgical techniques, proper use of the surgical instruments, and post-operative patient management are considerations essential to a successful outcome.
For full safety information, visit: https://itrack-advance.com/us




