

As a practice leader and cataract and refractive surgeon, you are no stranger to the uphill battle of maintaining efficiency. Ophthalmology, once known for its streamlined operations, now faces a new era of obstacles. Staffing shortages, increased training demands, and reduced reimbursement rates have created a high-pressure environment that requires you to deliver an exceptional patient experience with fewer resources.
This article offers strategies for improving patient flow and enhancing clinical efficiency through benchmarking, while keeping the patient experience at the forefront.
BENCHMARKING FOR EFFICIENCY
Benchmarking is a valuable tool for identifying areas of improvement within your practice. For instance, if you or your staff notices a significant increase in patient wait times, benchmarking against industry standards can help identify the underlying cause. Implementing strategies to reduce wait times can then improve overall efficiency.
Understanding ratios and their impact on workflow allows you to use benchmarks as metrics for continuous improvement and take control of your practice’s efficiency.
CAVEATS OF BENCHMARKING
Remember that benchmarking serves as a directional tool. Before using benchmarks to make clinical or business decisions, review the following guidance:
- Understand the definitions and formulas behind each benchmark to ensure accurate comparisons.
- Recognize that ratios are derived from two numbers; understanding these numbers can help you affect meaningful change.
- Avoid overreacting to benchmark results. Instead, seek to understand the reasons behind the metrics and use multiple benchmarks to guide your decisions.
- Use benchmarking to draw comparisons, set goals, develop tactical plans, and implement improvements.
As the English mathematician and biostatistician Karl Pearson noted, “That which is measured improves. That which is measured and reported improves exponentially.” Benchmarking allows you to measure your practice’s efficiency and share these metrics with your colleagues and staff. When done correctly, this process can enhance your practice’s efficiency and build confidence among your team and patients.
PROVIDER PRODUCTIVITY MEASURES
The 25th to 75th percentile range is relevant in assessing performance and identifying opportunities for enhancement. Key productivity measures such as net collections, doctor days, patients per day, and collections per visit offer insights into your practice’s performance and efficiency. These benchmarks vary between highly medical practices and primarily elective or refractive practices. Thus, it is crucial to compare apples to apples.
TECHNICIAN BENCHMARKS
Examining workup, wait, dilation, and doctor exam times provides valuable information on the efficiency of technician workflow. Evaluating benchmarks by exam element and electronic health record (EHR) usage can identify areas for improvement (Table 1).

STRATEGIES FOR CLINICAL EFFICIENCY
Patient Intake
Consider ways to streamline the patient check-in process. Automating appointment confirmations via text and email with a link to complete preregistration and health history can be highly effective. Your clinic can also call patients before their visit to document their medical history, allergies, and medications and complete a review of systems. This saves precious chair time, helps avoid bottlenecks, and provides a personal touch.
Previous Notes
Reduce patient wait times by teaching technicians how to minimize time spent reviewing previous notes. Train each technician to examine the last reason for the patient’s return and the indicated need for the day’s appointment. If a patient is referred for a consultation, the referring physician’s notes should be in the patient record and reviewed beforehand. Technicians should also avoid “precharting” without the patient present to ensure the accuracy of information.
Video Consults
To improve patient education and enhance their understanding of refractive surgery options, consider leveraging digital media or video calls before surgical consultations. A surgical coordinator can call a new patient, welcome them to the practice, and inform them about what to expect at a cataract evaluation. The surgical coordinator can also email links to educational videos (eg, “What Is a Cataract?”) to improve the patient experience and speed up the exam. These touchpoints help patients feel connected, informed, and confident when they come in for their consultation.
CUSTOMER RELATIONSHIP MANAGEMENT AND AI
Leveraging customer relationship management technologies and AI transcription for data capture can improve workflow efficiency. Many EHR vendors are integrating AI transcription technology into their software to record patient conversations and upload relevant clinical information into the chart.
ROADMAP TO ENHANCED EFFICIENCY
Another strategy for enhancing workflow efficiency is to emphasize effective communication and reevaluate practice templates. Layer schedules to identify bottlenecks and effectively coordinate staff, technology, and resources. The objective is to use these data to identify where adjustments should be made to the scheduling templates to maximize the number of patients while minimizing wait times and friction points (Figure). (Editors’ note: For additional workflow guidelines, see the sidebar.)

Figure. A visual representation of a layered schedule, designed to identify bottlenecks and optimize the coordination of staff, technology, and resources.
Additional Workflow Guidelines
To enhance your clinic’s efficiency further, consider implementing the following workflow guidelines:
- Designate a visual field technician;
- Assign technician roles by clinic session;
- Assign workup rooms to technicians daily;
- Develop a testing technician position; and
- Train surgical counselors to provide patient education and schedule surgical procedures.
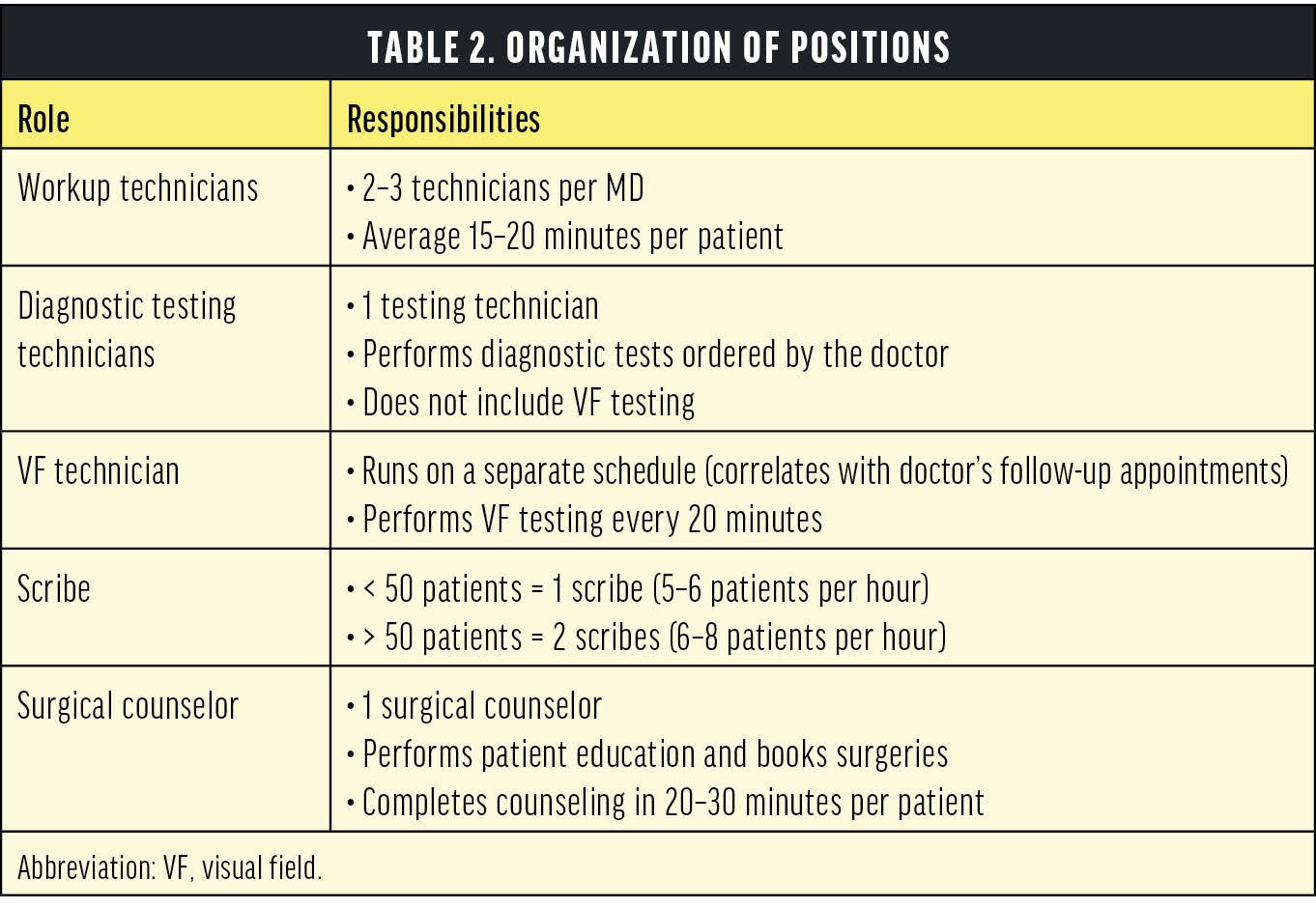
ORGANIZATION OF POSITIONS
Consider ways to improve the organization of your clinical positions (Table 2). For example, a scheduling template helps define and delineate the efficiency and responsibility of workup and diagnostic testing technicians, scribes, and surgical coordinators. Ensure each position is well trained, performing at the highest level, and utilizing their skills and abilities effectively. For example, train technicians to perform refractometry, thus allowing MDs and ODs to rely on accurate measurements. Cross-training your clinical team can help avoid gaps in coverage in unexpected situations.
TIME MANAGEMENT AND LEAN SIX SIGMA
The field of ophthalmology enjoys robust benchmarking metrics, but it is essential to understand how your practice performs and track your progress against your benchmarks. Following are three tips for effectively managing your practice’s time:
No. 1: Time Trials
Implement time trials and apply Lean Six Sigma principles to streamline operations and enhance patient interactions. Lean Six Sigma is a process improvement methodology that combines Lean principles, which focus on eliminating non–value-adding activities, with Six Sigma, which aims to reduce defects and variability by systematically removing waste and reducing variation in processes.1 In ophthalmology, Lean improvement involves analyzing current workflows, identifying inefficiencies, and implementing targeted improvements.
No. 2: Time Metrics
Develop systems to log patient wait times from the front desk, workup, and doctor exams. Work as a team to identify bottlenecks and brainstorm solutions to address them.
No. 3: Workplace Efficiency
Foster workplace efficiency by providing technical training and cross-training to optimize overall workflow.
IMPLEMENTATION AND CHANGE MANAGEMENT
Effective communication is essential when implementing scheduling updates and managing unusual situations. Designating a flow manager, such as a clinical director or lead technician, and using EHR software for tracking metrics can help you navigate changes successfully and enhance workflow efficiency. Openly communicating the reasons for each change and involving the team in decision-making can alleviate discomfort and gain support for the effort.
CONCLUSION
Efficient workflow management is crucial for delivering high-quality patient care. Implementing the strategies outlined in this article can improve your practice’s productivity, boost team morale, and enhance the patient experience. As Peter Drucker once said, “Time is the scarcest resource, and unless it is managed, nothing else can be managed.”
1. Kenton W. Lean Six Sigma: Definition, Principles, and Benefits. Investopedia. Updated July 1, 2024. Accessed August 2, 2024. https://www.investopedia.com/terms/l/lean-six-sigma.asp




