CASE PRESENTATION
A 20-year-old woman presents with light sensitivity, decreased BCVA, and difficulty driving at night. The patient has a 5-year history of superficial keratitis, which has been responsive to pulsed topical corticosteroids. Refractive and therapeutic contact lenses, artificial tears, temporary punctal occlusion (epiphora), and treatment with cyclosporine ophthalmic emulsion 0.05% (Restasis, AbbVie), cyclosporine ophthalmic emulsion 0.09% (Cequa, Sun Ophthalmics), and lifitegrast ophthalmic solution 5% (Xiidra, Bausch + Lomb) have failed to resolve her symptoms. She is wearing glasses at present. Her current drug regimen consists of cyclosporine ophthalmic solution 0.1% (Vevye, Harrow) instilled twice per day and varenicline solution nasal spray 0.03 mg (Tyrvaya, Viatris) administered three times per day.
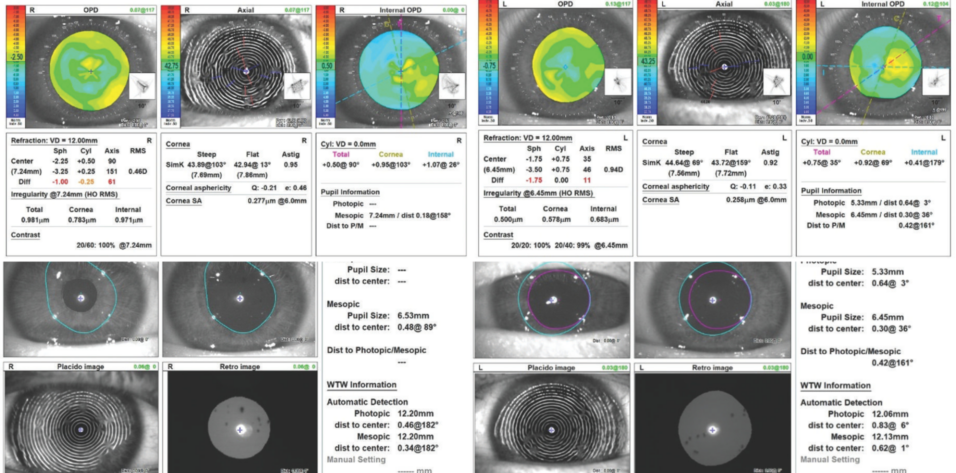
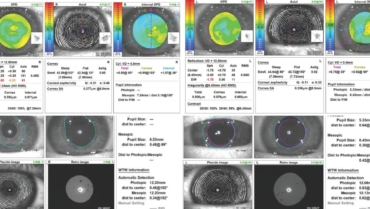
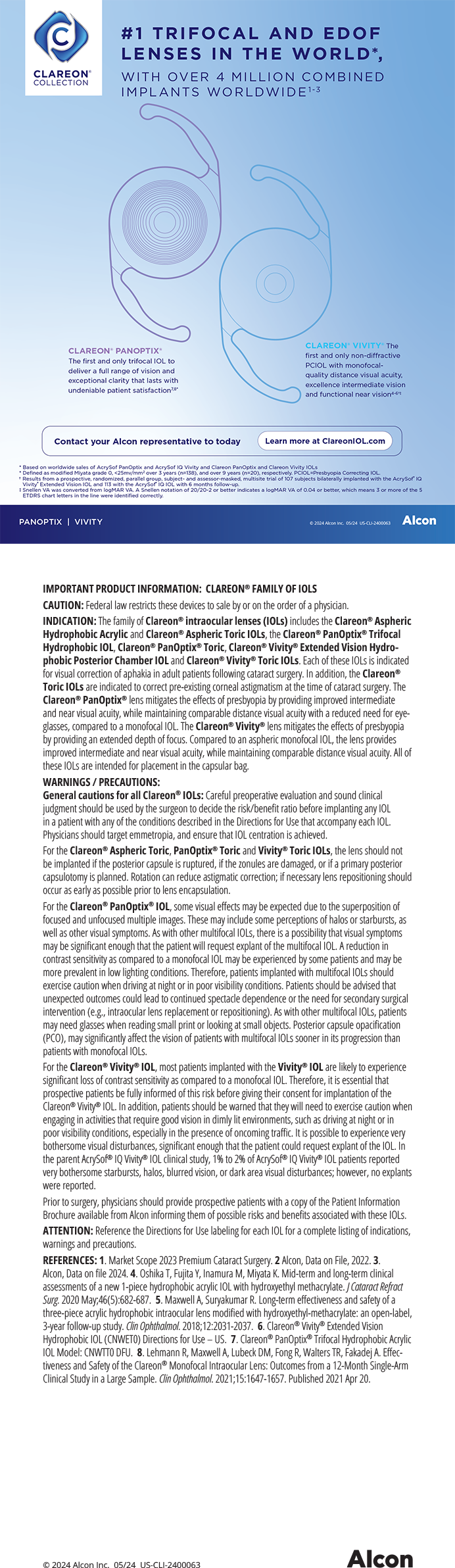
The patient’s current glasses prescription is -2.50 +0.50 x 090º = 20/40 OD and -3.25 +0.75 x 035º = 20/40 OS. Upon examination, her manifest refraction is -2.50 D spherical equivalent = 20/30 OD and -2.50 +0.25 x 035º = 20/25 OS. Her IOP reading is 14 mm Hg OU. An analysis with retroillumination (Figure 1), corneal topography (Figure 2), and an assessment of optical quality (Figure 3) are performed. The remainder of the examination is normal.

Figure 1. Retroillumination of both eyes shows the corneal lesions and Placido images.

Figure 2. Corneal topography and irregularity indices of both eyes.

Figure 3. An assessment of both eyes with the Damian Gatinel Optical Quality Analysis Software on the OPD-Scan III (Nidek).
The most likely diagnoses are myopia with astigmatism, Thygeson superficial punctate keratitis (SPK), and rosacea with ocular involvement. The patient wishes to improve her vision and asks what her options for treatment are. How would you proceed?
—Case prepared by Karl G. Stonecipher, MD

JAY S. PEPOSE, MD, PHD
Thygeson SPK is a bilateral, chronic, recurrent disease with a natural history of exacerbations and remissions that may span years or even decades. Disease activity is associated with photophobia, epiphora, burning, and foreign body sensation, with pathognomonic corneal lesions characterized by discrete, grouped, round to oval, granular, chalk-like intraepithelial opacities and minimal to no conjunctival injection. Thygeson SPK is generally responsive to treatment with topical calcineurin inhibitors and corticosteroids. With the latter medications, however, a very slow taper may be required, and injudicious use can prolong the disease.
The etiology or etiologies of the condition remain enigmatic. Two cases with positive viral cultures have been reported,1,2 but the findings have not been corroborated by additional cases or polymerase chain reaction studies.3 Perhaps in the future, more information regarding disease etiology can be obtained with molecular diagnostic techniques that are hypothesis-free and analyze all the nucleic acid in a sample, such as shotgun metagenomic next-generation sequencing (also called metagenomic deep sequencing). Unmasked, uncontrolled reports of a clinical response of Thygeson SPK to topical antivirals4 are indeterminate and require rigorous confirmation via masked, controlled, prospective studies.
During exacerbation, the grouped lesions develop a raised, elevated center. They stain with fluorescein and vital dyes and may break through the corneal surface, leading to irregular astigmatism, elevated irregularity indices, and poor predicted image quality, as occurred in this case. The patient has presumably lost lines of BCVA. A gas permeable contact lens overrefraction might help differentiate between the component of vision loss due to irregular astigmatism and that due to optical scatter from corneal opacities. A brief, intensive course of topical corticosteroids could be initiated to see if treatment leads to disease remission and an increase in her BCVA.
Laser scrape or phototherapeutic keratectomy has been combined with PRK for the simultaneous treatment of Thygeson SPK and underlying refractive error.5-8 In this case, PRK, unlike LASIK, could regularize the ocular surface and ablate any viral or other subepithelial antigens that theoretically might play a role in disease immunopathogenesis. This hypothesis is supported by a case report of recurrent Thygeson SPK 17 months after PRK, with opacities located only outside the laser ablation zone and no central lesions6 and another patient who experienced a recurrence in the eye treated with LASIK but not in the contralateral eye treated with PRK.8 Other case reports, however, have described disease recurrence both inside and peripheral to the PRK ablation zone,7 akin to failed attempts at preventing recurrence through debridement.9
Because confocal microscopy has shown an abundance of dendritic cells in the basal epithelial cell layer and subepithelial nerve plexus10 and reflective keratocytes in the anterior stroma,11 it may be prudent to apply mitomycin C (MMC) following excimer laser ablation in an effort to minimize the transformation of activated keratocytes into myofibroblasts, with associated corneal haze or scarring. The patient should be informed that her Thygeson SPK may recur following PRK. Consideration should be given to continuing the long-term prophylactic use of topical cyclosporine.

STEPHEN A. WEXLER, MD
Thygeson SPK is a presumed inflammatory disease of the superficial cornea characterized by recurrent episodes of discomfort and photophobia. The clinical appearance typically involves round or oval grey lesions in the epithelium that stain slightly with fluorescein. The disease usually does not have much effect on the individual’s visual acuity, but this patient has experienced a loss of BCVA.
Several case reports have shown that patients who have Thygeson SPK can do well with PRK versus LASIK surgery.1,3,4,6 Although I have not seen a patient with this level of visual involvement, I have performed PRK on several individuals with low-grade, typical Thygeson SPK in the past and achieved good refractive results and an improvement in their symptoms.
This patient has minimal refractive error and no contraindication to PRK surgery. I would recommend PRK with MMC using my standard technique of 25% ethyl alcohol applied for 20 seconds for epithelial removal. I usually prescribe steroid treatment for 2 weeks following surgery but would consider extending the duration for the patient. I would also consider prescribing oral tetracycline to treat her rosacea.

RONALD R. KRUEGER, MD
This uncommon surgical case is instructive. In this article, we laser refractive surgeons have come to a fork in the road, so to speak, with regard to which procedure might best reduce the patient’s disease recurrence rate while also correcting her myopia. LASIK offers the benefit of rapid postoperative recovery, and some might argue that cutting the superficial corneal nerves with a flap might alleviate the recurrence of Thygeson SPK. In my opinion, however, LASIK would be the wrong choice.
I believe PRK would be a better strategy for two reasons. First, preoperative corneal topography shows paracentral irregular astigmatism, which indicates epithelial irregularity due to multiple reactivations of Thygeson SPK. Although topography-guided LASIK can effectively correct myopia and higher-order aberrations, the irregularity observed in this case is likely due to the epithelium, which would be better removed with a PRK procedure targeting the correction of only myopia. Second, the literature shows a lower rate of Thygeson SPK recurrence has been found after PRK, which removes the epithelium and superficial cornea, where the disease tends to reactivate.5,6,8
This was confirmed in a 32-year-old female patient of mine who had a history of bilateral Thygeson SPK and underwent laser vision correction for myopia with astigmatism. Her right eye underwent PRK and did not experience a disease recurrence. Her left eye, however, experienced recurrence within 10 months after undergoing LASIK,8 suggesting that surface ablation was the better choice. Additionally, in a case report where a recurrence of Thygeson SPK was experienced after PRK, the disease occurred in the periphery, outside the zone of PRK treatment.6 This indicates that the inflammatory signal of recurrence resided in the superficial cornea, which was ablated away. In a case series from India, PRK was not performed, but superficial epithelial keratectomy with a viral culture was performed in several patients with mixed results.12 Although Thygeson SPK might be associated with a viral etiology, there is also a genetic association with HLA-DR3, which is an immunogenic antigen. These findings help confirm an inflammatory source of the disease, but neither clearly explains its etiology or pathogenesis.
Although Thygeson SPK can be treated with a variety of topical antiinflammatory agents, evidence suggesting that PRK and phototherapeutic keratectomy can mitigate recurrence not only helps us with disease management but offers a vision correction solution for patients who have the condition.

WHAT I DID: KARL G. STONECIPHER, MD
PRK based on the patient’s manifest refraction and using the Wavelight EX500 laser (Alcon) was performed. The epithelium was removed mechanically, and topical MMC was applied for 12 seconds. Her rosacea was treated topically with compounded triple cream (azelaic acid 15%, ivermectin 1%, and metronidazole 1%) and photobiomodulation using low-light therapy (red and blue; Espansione).
The patient’s UCVA subsequently improved to 20/20 OU. She has remained symptom-free for 6 months on a regimen of twice-daily cyclosporine ophthalmic solution 0.1% in each eye and varenicline solution nasal spray as needed.
1. Braley AE, Alexander RC. Superficial punctate keratitis; isolation of a virus. AMA Arch Ophthalmol. 1953;50(2):147-154.
2. Lemp MA, Chambers RW Jr, Lundy J. Viral isolate in superficial punctate keratitis. Arch Ophthalmol. 1974;91(1):8-10.
3. Connell PP, O'Reilly J, Coughlan S, Collum LM, Power WJ. The role of common viral ocular pathogens in Thygeson’s superficial punctate keratitis. Br J Ophthalmol. 2007;91(8):1038-1041.
4. Nesburn AB, Lowe GH 3rd, Lepoff NJ, Maguen E. Effect of topical trifluridine on Thygeson’s superficial punctate keratitis. Ophthalmology. 1984;91(10):1188-1192.
5. Goldstein MH, Feistmann JA, Bhatti MT. PRK-pTK as a treatment for a patient with Thygeson’s superficial punctate keratopathy. CLAO J. 2002;28(4):172-173.
6. Fite SW, Chodosh J. Photorefractive keratectomy for myopia in the setting of Thygeson’s superficial punctate keratitis. Cornea. 2001;20(4):425-426.
7. Seo KY, Lee JB, Jun RM, Kim EK. Recurrence of Thygeson’s superficial punctate keratitis after photorefractive keratectomy. Cornea. 2002;21(7):736-737; author reply 737.
8. Netto MV, Chalita MR, Krueger RR. Thygeson’s superficial punctate keratitis recurrence after laser in situ keratomileusis. Am J Ophthalmol. 2004;138(3):507-508.
9. Tabbara KF, Ostler HB, Dawson C, Oh J. Thygeson’s superficial punctate keratitis. Ophthalmology. 1981;88(1):75-77.
10. Li J, Qiao J, Cai M, Wang L. Laser confocal microscopy findings of Thygeson superficial punctate keratitis. Chin Med J (Engl). 2014;127(3):597-598.
11. Watson SL, Hollingsworth J, Tullo AB. Confocal microscopy of Thygeson’s superficial punctate keratopathy. Cornea. 2003;22(4):294-299.
12. Priyadarshini SR, Roy A, Das S. Thygeson’s superficial punctate keratopathy: a review and case series. Indian J Ophthalmol. 2021;69(4):806-811.